Niche-Specific Virulence: Comparative Genomics and Evolutionary Drivers of Pathogen Adaptation
This article synthesizes recent advances in understanding how virulence factors are shaped by ecological niches.
Niche-Specific Virulence: Comparative Genomics and Evolutionary Drivers of Pathogen Adaptation
Abstract
This article synthesizes recent advances in understanding how virulence factors are shaped by ecological niches. For researchers and drug development professionals, we explore the foundational concept that many 'virulence factors' are, in fact, niche adaptation factors selected by environmental pressures. We detail methodological approaches in comparative genomics and machine learning for identifying these traits, address challenges in distinguishing true virulence, and present validation through cross-niche comparisons. The synthesis underscores that a One Health perspective, integrating human, animal, and environmental reservoirs, is crucial for managing antibiotic resistance and developing targeted antimicrobial strategies.
Defining Virulence in Context: From Niche Factors to Pathogenic Traits
The traditional concept of "virulence factors" is undergoing a significant paradigm shift in microbial pathogenesis research. Historically, any bacterial structure or strategy that contributed to the infectious potential of a pathogen was classified as a virulence factor. This included capsules, flagella, pili, secretion systems, exotoxins, and iron acquisition systems [1]. However, the increasing interest in the human microbiota and comparative genomics has revealed a critical insight: harmless commensal organisms frequently possess the very same structures and strategies to compete in complex biological ecosystems [1]. This observation challenges the fundamental definition of virulence factors and suggests that many such factors might be more accurately described as "niche factors" – essential adaptations for survival in specific environments, whether pathogenic or commensal.
This distinction is not merely semantic but has profound implications for how we understand host-microbe interactions, develop therapeutic interventions, and regulate probiotic products [1]. The emerging framework necessitates a more precise vocabulary that distinguishes between factors causing damage to the host and those that simply enable microorganisms to persist in their ecological niche. This article examines the conceptual shift from virulence factors to niche factors through the lens of comparative genomics and experimental studies, providing objective data and methodologies that illuminate this evolving paradigm.
Conceptual Framework: Distinguishing Niche Adaptation from Pathogenesis
Defining Characteristics and Functions
The distinction between virulence factors and niche factors hinges on their fundamental purpose and distribution across microbial species.
Table 1: Comparative Features of Virulence Factors and Niche Factors
| Feature | Virulence Factors | Niche Factors |
|---|---|---|
| Primary Function | Cause damage to host; access sterile body sites | Promote colonization, survival, and competition in a specific ecological niche |
| Presence in Commensals | Rare or absent in harmless commensals | Common in both pathogens and commensals occupying similar niches |
| Host Damage | Directly cause tissue damage or dysregulate immunity | Do not inherently cause damage; may become detrimental in compromised hosts or abnormal locations |
| Examples | Cytolytic toxins, invasins, superantigens, neurotoxins | Bile tolerance systems, attachment mechanisms, nutrient acquisition systems, immune evasion in non-sterile sites |
| Regulatory Implications | Prohibit use in probiotics | Generally acceptable for probiotics unless context indicates risk |
This conceptual framework finds practical application in regulatory science. European Food Safety Authority (EFSA) guidelines require evidence that "virulence factors" are absent in novel commensals proposed for use as probiotics [1]. A literal interpretation could mistakenly prohibit the use of beneficial microbes like Bifidobacterium breve due to the presence of TadIV pili, which function as niche factors in the gastrointestinal tract despite being classified as virulence factors in pathogens like Yersinia enterocolitica [1].
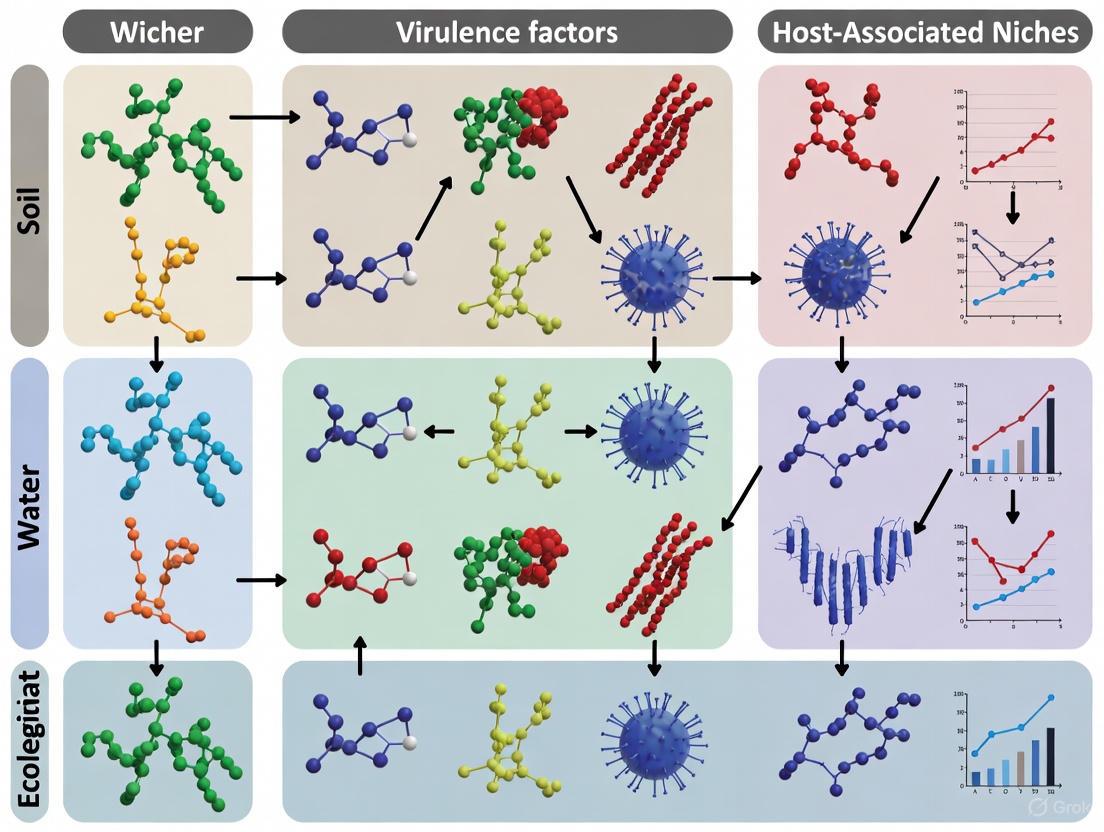
Visualizing the Conceptual Relationship
The following diagram illustrates the relationship between virulence factors, niche factors, and their shared characteristics in pathogenic and commensal microorganisms.
Genomic Evidence: Comparative Analyses Across Ecological Niches
Recent advances in whole-genome sequencing and bioinformatics have enabled large-scale comparative studies that illuminate the genetic basis of niche adaptation [2]. These investigations reveal how similar genetic tools are deployed by both pathogens and commensals, supporting the niche factor concept.
Large-Scale Genomic Comparisons
A comprehensive comparative genomic analysis of 4,366 high-quality bacterial genomes isolated from various hosts and environments demonstrated significant variability in bacterial adaptive strategies [2] [3]. Human-associated bacteria, particularly from the phylum Pseudomonadota, exhibited higher detection rates of carbohydrate-active enzyme (CAZyme) genes and adhesion-related factors, indicating co-evolution with the human host [2]. In contrast, environmental isolates showed greater enrichment in genes related to metabolism and transcriptional regulation, highlighting their adaptability to diverse external environments [2].
Table 2: Genomic Feature Distribution Across Ecological Niches (Based on 4,366 Bacterial Genomes)
| Genomic Feature | Human-Associated | Animal-Associated | Environment | Clinical Isolates |
|---|---|---|---|---|
| Carbohydrate-Active Enzymes | Higher detection rates | Moderate detection rates | Variable | Elevated in human pathogens |
| Adhesion Factors | Enriched | Present | Less common | Highly enriched |
| Antibiotic Resistance Genes | Variable | Significant reservoirs | Less common | Highest detection rates |
| Metabolic Pathway Genes | Host-adapted | Host-adapted | Highly diverse | Constrained |
| Immune Evasion Factors | Enriched | Present | Rare | Highly enriched |
These findings align with the niche factor hypothesis, demonstrating that many genes traditionally classified as virulence factors are actually niche-specific adaptations. For instance, bile salt hydrolase (BSH) activity, initially characterized as a virulence factor in Listeria monocytogenes, is also present in many commensals marketed as probiotics [1]. This widespread distribution suggests BSH primarily functions as a gastrointestinal niche factor rather than a dedicated virulence mechanism.
Within-Host Evolution Studies
Investigations of bacterial evolution within host environments provide compelling evidence for the niche factor concept. A detailed study tracking the evolution of a single multidrug-resistant Klebsiella pneumoniae clone across 110 patients during a 5-year nosocomial outbreak revealed strong positive selection targeting key virulence factors [4]. The research demonstrated convergent evolutionary trajectories dominated by reduced acute virulence and recurrent changes in iron uptake regulation, capsule production, and lipopolysaccharide composition – changes that likely represent clinical niche adaptations [4].
Notably, mutations in genes associated with capsule production (wcoZ, wzc), lipopolysaccharide synthesis (manB, manC), and iron utilization (sufB, sufC, fepA/fes) showed significant signs of positive selection, with a nonsynonymous vs. synonymous substitution ratio (dN/dS) of 49.7 for genes with three or more independent mutations [4]. These adaptive changes often resulted in trade-offs during gastrointestinal colonization, highlighting how niche-specific optimizations can simultaneously enhance fitness in one context while reducing it in another.
Experimental Approaches: Methodologies for Differentiation
Comparative Genomic Workflow
The following diagram outlines a standardized workflow for conducting comparative genomic analyses to identify niche-specific adaptations across bacterial isolates from different ecological sources.
Detailed Experimental Protocol:
Genome Collection and Quality Control: Obtain high-quality bacterial genomes from public databases (e.g., gcPathogen) [2]. Implement stringent quality control: exclude sequences assembled at contig level; retain genomes with N50 ≥50,000 bp; ensure CheckM completeness ≥95% and contamination <5%; remove genomes with unclear source information [2].
Ecological Niche Annotation: Categorize genomes based on detailed metadata of isolation sources: "human" (clinical samples, human tissues), "animal" (livestock, wildlife), and "environment" (soil, water, air) [2]. This classification enables analysis of adaptation to different ecological contexts.
Functional Annotation: Predict open reading frames using Prokka v1.14.6 [2]. Annotate functions using:
- COG database for general functional categories (RPS-BLAST, e-value <0.01, coverage >70%)
- dbCAN2 for carbohydrate-active enzymes (HMMER, e-value <1e-5)
- VFDB for virulence factor identification (ABRicate with default parameters)
- CARD for antibiotic resistance genes [2]
Phylogenetic Analysis: Construct maximum likelihood phylogenetic trees using 31 universal single-copy genes identified by AMPHORA2 [2]. Perform multiple sequence alignment with Muscle v5.1 and tree construction with FastTree v2.1.11 [2].
Statistical Comparison: Convert phylogenetic trees to evolutionary distance matrices using R package ape [2]. Perform k-medoids clustering to identify population structure. Calculate enrichment of specific functions across ecological niches using hypergeometric tests with multiple testing correction.
Machine Learning Application: Employ algorithms (e.g., random forests, support vector machines) to identify signature genes associated with specific niches [2]. Use Scoary for gene presence/absence association testing [2].
Phenotypic Validation Assays
Genomic predictions require phenotypic validation to confirm the functional role of putative niche factors:
Mucoviscosity and Capsule Production: Quantify capsule expression using India ink staining and sedimentation assays [4].
Serum Survival: Assess serum resistance by incubating bacteria in fresh human serum and monitoring viability over time [4].
Iron Utilization: Evaluate siderophore production using chrome azurol S assays and measure growth under iron-limited conditions [4].
Biofilm Formation: Quantify biofilm production using crystal violet staining in microtiter plates [4].
Infection Potential: Assess virulence alterations using Galleria mellonella infection models, monitoring survival curves and bacterial loads [4].
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for Virulence/Niche Factor Studies
| Reagent/Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Bioinformatics Databases | VFDB, CARD, PATRIC, COG, dbCAN | Virulence factor, resistance gene, and functional annotation | Comparative genomics, VFAR analyses |
| Genomic Analysis Tools | Prokka, ABRicate, Scoary, AMPHORA2 | Genome annotation, gene presence/absence testing, phylogenetic marker identification | Functional annotation, association studies |
| Alignment & Phylogenetics | Muscle v5.1, FastTree v2.1.11, MEGA v11.0.13 | Multiple sequence alignment, phylogenetic tree construction | Evolutionary analysis, molecular phenetics |
| Metabolomic Pathways | MetaboAnalyst 6.0, KEGG, HMDB | Metabolic pathway enrichment analysis | Metabolomic adaptations across niches |
| Phenotypic Assay Reagents | Chrome azurol S, India ink, Crystal violet | Siderophore detection, capsule staining, biofilm quantification | Functional validation of niche adaptations |
Case Studies: Exemplifying the Conceptual Shift
Bacterial Systems: FromListeriato Probiotics
The bile tolerance system BilE in Listeria monocytogenes was initially characterized as a virulence factor because it contributes to gastrointestinal survival and is regulated by the master virulence regulator PrfA [1]. However, similar bile tolerance mechanisms must exist in commensal organisms inhabiting the bile-rich regions of the GI tract [1]. This realization prompted reconsideration of BilE as a niche factor required for gastrointestinal survival, which happens to play an important role in the infectious lifestyle of the pathogen [1].
Similarly, bile salt hydrolase (BSH) activity in L. monocytogenes was described as a PrfA-regulated virulence factor [1]. However, deletion of bsh genes reduces the ability of the organism to colonize by diminishing bile coping capacity, and BSH activity is also present in many commensals marketed as probiotics [1]. This distribution across pathogens and commensals strongly supports its reclassification as a niche factor.
Fungal Systems:Cryptococcus neoformansAdaptations
Molecular phenetic and metabolomic analyses of Cryptococcus neoformans isolates reveal distinct adaptive strategies between clinical and environmental niches [5]. Clinical isolates demonstrate enriched sulfur metabolism and glutathione pathways, likely representing adaptations to oxidative stress in host environments [5]. In contrast, environmental isolates favor methane and glyoxylate pathways, suggesting adaptations for survival in carbon-rich environments [5].
These niche-specific metabolic specializations illustrate how the same microorganism utilizes different biochemical pathways to thrive in distinct ecological contexts. The clinical adaptations enhance virulence in human hosts but originated as niche-specific optimization rather than dedicated virulence mechanisms.
Emerging Frontiers: Virulence Factor Activity Relationships (VFARs)
The concept of Virulence Factor Activity Relationships (VFARs) represents a predictive framework for ranking microbial risks based on structural and functional characteristics of virulence factors [6]. Similar to quantitative structure-activity relationships (QSARs) for chemicals, VFARs leverage bioinformatics databases and tools to compare newly identified virulence factors against known references for virulence prediction [6].
More than 20 bioinformatics databases and tools have been developed over the last decade with dedicated virulence and antimicrobial resistance prediction capabilities [6]. Key resources include:
- PATRIC: Integration and visualization of virulence factors across 22,000 whole genome sequences [6]
- VFDB: Distribution of virulence factors in distinct categories with inter-genera comparison capability [6]
- CARD: Curated collection of antibiotic resistance gene sequences with detection software [6]
- VirulenceFinder: Detection of virulence genes based on whole-genome sequencing data [6]
These tools enable researchers to apply VFAR approaches to rank and prioritize organisms important to specific niches, combining genomic data with engineering and economic analyses for comprehensive risk assessment [6].
The conceptual shift from virulence factors to niche factors represents a fundamental evolution in our understanding of host-microbe interactions. This refined perspective acknowledges that many microbial factors traditionally viewed through a lens of pathogenicity actually represent adaptations to specific ecological niches, exploited by both commensals and pathogens alike.
This paradigm shift has profound implications for drug development and probiotic regulation. Therapeutic strategies can now more precisely target genuine virulence mechanisms (those causing direct host damage) while preserving niche factors that enable beneficial colonization. Furthermore, regulatory frameworks for probiotics can evolve to distinguish between true virulence factors and essential niche factors required for gastrointestinal survival and competition.
As comparative genomics and functional studies continue to illuminate the continuum between commensalism and pathogenesis, the niche factor concept provides a more nuanced and accurate framework for understanding microbial ecology and evolution. This perspective ultimately enhances our ability to develop targeted antimicrobials, design effective probiotics, and implement rational regulatory policies that reflect the complex reality of host-microbe interactions.
The evolutionary arms race between bacterial pathogens and their hosts is a fundamental aspect of microbial pathogenesis. Understanding how ecological niches shape bacterial evolution is critical for developing novel therapeutic strategies, especially in an era of escalating antimicrobial resistance. This comparison guide examines how distinct selective pressures in human, animal, and environmental reservoirs drive the diversification of virulence factors and resistance mechanisms in bacterial pathogens. The dynamic interplay between these niches facilitates continuous pathogen evolution, with significant implications for global health.
Recent advances in comparative genomics have revealed that bacterial pathogens employ niche-specific adaptive strategies to colonize new hosts and survive under diverse environmental conditions [2]. The World Health Organization's One Health approach emphasizes the interconnected nature of human, animal, and environmental health, particularly relevant when considering the dissemination of virulence factors and antibiotic resistance genes [2]. This guide provides a systematic comparison of virulence mechanisms across ecological niches, offering experimental data and methodological frameworks to support research in bacterial pathogenesis and drug development.
Genomic Adaptations Across Ecological Niches
Comparative Genomic Analysis of Niche-Specific Adaptations
Large-scale comparative genomic studies reveal distinct evolutionary trajectories for bacteria occupying different ecological niches. An analysis of 4,366 high-quality bacterial genomes isolated from various hosts and environments demonstrated significant variability in bacterial adaptive strategies [2].
Table 1: Genomic Features Across Ecological Niches
| Ecological Niche | Dominant Bacterial Phyla | Enriched Genomic Features | Adaptive Strategies |
|---|---|---|---|
| Human-associated | Pseudomonadota | Higher prevalence of carbohydrate-active enzyme genes; virulence factors for immune modulation and adhesion | Gene acquisition; co-evolution with human host |
| Animal-associated | Diverse phyla | Significant reservoirs of antibiotic resistance genes; host-specific virulence factors | Horizontal gene transfer; zoonotic transmission |
| Environmental | Bacillota, Actinomycetota | Metabolism and transcriptional regulation genes; stress response systems | Genome reduction; metabolic versatility |
| Clinical settings | Multiple pathogenic genera | High abundance of antibiotic resistance genes (e.g., fluoroquinolone resistance) | Rapid evolution under antibiotic pressure |
Human-associated bacteria, particularly from the phylum Pseudomonadota, exhibit genomic signatures of co-evolution with their host, including higher detection rates of carbohydrate-active enzyme genes and virulence factors related to immune modulation and adhesion [2]. In contrast, environmental bacteria show greater enrichment in genes related to metabolism and transcriptional regulation, highlighting their adaptability to diverse physical and nutritional conditions. Clinical isolates demonstrate the highest prevalence of antibiotic resistance genes, reflecting the strong selective pressure imposed by antimicrobial therapy.
Within-Host Evolutionary Trajectories in Opportunistic Pathogens
Hospital outbreaks provide unique opportunities to study bacterial evolution over defined timeframes. A detailed analysis of a multidrug-resistant Klebsiella pneumoniae clone during a 5-year nosocomial outbreak affecting 110 patients revealed strong positive selection targeting key virulence factors [4].
Table 2: Convergent Evolutionary Changes in a Hospital K. pneumoniae Outbreak
| Gene/Region | Function | Type of Change | Biological Significance |
|---|---|---|---|
| manB/manC | O-antigen synthesis (O3b-type) | Nonsynonymous mutations | Altered lipopolysaccharide structure |
| wcoZ/wzc | Capsule biosynthesis (KL51) | Nonsynonymous mutations | Modified capsule production |
| uvrY | Response regulator in BarA-UvrY two-component system | Nonsynonymous mutations | Altered regulation of virulence and metabolism |
| sufB/sufC | Iron-sulfur cluster synthesis | Nonsynonymous mutations | Changes in iron homeostasis |
| fepA/fes intergenic region | Siderophore uptake and enterobactin esterase regulation | Regulatory mutations | Modified iron acquisition |
The study identified a strong signal of positive selection (dN/dS = 49.7) in genes with three or more independent mutations, indicating adaptive within-host evolution [4]. Convergent evolutionary trajectories were dominated by reduced acute virulence and recurrent changes in iron uptake regulation, capsule, and lipopolysaccharide production, with enhanced biofilm formation. These phenotypic changes represent clinical niche adaptations, with some resulting in trade-offs during gastrointestinal colonization.
Experimental Approaches for Studying Niche Adaptation
Methodologies for Comparative Genomic Analysis
The experimental framework for comparing virulence factors across ecological niches relies on integrated genomic and phenotypic approaches:
Genome Sequencing and Quality Control: Researchers obtained metadata for 1,166,418 human pathogens from the gcPathogen database and implemented stringent quality control procedures [2]. This included retaining genome sequences with N50 ≥50,000 bp, CheckM completeness ≥95%, and contamination <5%. Following removal of bacterial genomes with unclear source information, 4,366 high-quality, non-redundant pathogen genome sequences were retained for comparative analysis.
Phylogenetic Analysis: To construct robust phylogenetic trees, 31 universal single-copy genes were retrieved from each genome using AMPHORA2 [2]. For each marker gene, multiple sequence alignments were generated using Muscle v5.1, followed by concatenation of the 31 alignments into a comprehensive dataset. Maximum likelihood trees were constructed using FastTree v2.1.11, with k-medoids clustering (k=8) implemented to compare genomic differences among bacteria from different ecological niches within the same ancestral clade.
Functional Annotation: Open reading frames were predicted using Prokka v1.14.6, with functional categorization performed through RPS-BLAST mapping to the Cluster of Orthologous Groups database (e-value threshold 0.01, minimum coverage 70%) [2]. Carbohydrate-active enzyme genes were annotated using dbCAN2 to map ORFs to the CAZy database, with filtering based on hmm_eval 1e-5.
Virulence Factor and Antibiotic Resistance Analysis: Virulence factors were identified using the Virulence Factor Database (VFDB), while antibiotic resistance genes were annotated through the CARD database [2] [7]. These comprehensive annotations enabled systematic comparison of virulence and resistance mechanisms across ecological niches.
Figure 1: Experimental workflow for comparative genomic analysis of bacterial niche adaptation
Assessing Virulence Gene Expression Under Environmental Stress
Understanding how environmental stressors affect virulence expression provides crucial insights into niche-specific adaptations. A study on Bacillus cereus employed quantitative PCR to measure expression of four virulence genes (nheA, hblD, cytK, and entFM) under different stress conditions [8].
Growth Conditions and Stress Exposure: B. cereus was cultured in LB broth medium for 14 h with shaking (37°C, 160 rpm), with OD values measured every 2 hours to plot growth curves [8]. For stress experiments, bacteria were exposed to different temperatures (20°C, 30°C, 40°C), pH levels (4.0, 6.0, 8.0), and salt concentrations (0.5%, 1.5%, 3.0%), both as single factors and in combination.
RNA Extraction and qPCR Analysis: After 14 hours of incubation under stress conditions, RNA was extracted using the RNAprep pure Bacteria Kit [8]. Quantitative PCR was performed using the StepOnePlus Real-Time Fluorescence PCR System with TB Green Premix Ex Taq II (Tli RNaseH Plus). Primer sequences for virulence genes were designed based on established references, with amplification conditions optimized for each target.
Pathogenicity Assessment: The pathological damage caused by B. cereus exposed to different stress conditions was evaluated in mouse models using histological sections of various organs [8]. This integrated approach connected gene expression changes with actual virulence potential.
The results demonstrated that environmental stressors significantly modulate virulence gene expression. High temperature (40°C) inhibited expression of most virulence genes, while pH and salt concentration had variable effects depending on the specific gene [8]. Under multiple stressors, nheA, hblD and cytK showed lowest expression at 40°C, pH 6.0, and 3.0% salt, while entFM was minimally expressed at 20°C, pH 8.0, and 1.5% salt concentration.
Pathogen-Specific Adaptation Mechanisms
Niche-Specific Virulence in Klebsiella pneumoniae
Klebsiella pneumoniae exemplifies how pathogens differentially utilize virulence factors across host niches. Research on hypervirulent K. pneumoniae (hvKp) has demonstrated that virulence plasmid-encoded factors play distinct roles depending on the infection site [9].
The virulence plasmid (KpVP) in hvKp encodes aerobactin (iuc), salmochelin (iro), and the capsule regulator rmpA [9]. Systematic analysis using isogenic mutants in various murine infection models revealed that aerobactin is indispensable for stable gut colonization, primarily by overcoming iron competition from the microbiota. In contrast, salmochelin plays a pivotal role in bloodstream dissemination by evading host-derived lipocalin-2. The hypermucoviscous capsule regulated by rmpA enhances systemic dissemination but is dispensable for gut colonization.
Figure 2: Niche-specific functions of K. pneumoniae virulence factors
This niche-specific functionality illustrates the sophisticated adaptation of pathogens to different host environments. The co-inheritance of iro and iuc loci in hypervirulent strains suggests their combined presence confers a selective advantage across host niches [9]. Furthermore, the convergence of multidrug resistance and hypervirulence in emerging strains highlights the evolutionary plasticity of K. pneumoniae in response to medical interventions.
Virulence and Resistance Dynamics in Escherichia coli from Dairy Cattle
Dairy cattle represent important reservoirs of Escherichia coli strains carrying both virulence and resistance factors, with significant implications for public health. A comprehensive genomic analysis of 172 E. coli isolates from dairy cattle across seven countries revealed distinct patterns of gene distribution [10].
Table 3: Virulence and Resistance Genes in Dairy Cattle E. coli
| Gene Category | Specific Genes | ESBL E. coli (%) | Non-ESBL E. coli (%) | Function |
|---|---|---|---|---|
| Antibiotic Resistance | sul2, blaTEM-1B, tet(A) | 92.1, 85.7, 81.0 | 62.4, 58.7, 64.2 | Sulfonamide, β-lactam, and tetracycline resistance |
| Virulence Factors | astA, iss, lpfA | 68.3, 61.9, 41.3 | 45.9, 33.9, 27.5 | Enteroaggregative toxin, increased serum survival, long polar fimbriae |
| Mobile Genetic Elements | IncFIB, IncFII, IncQ1 | 93.7, 84.1, 68.3 | 78.9, 69.7, 52.3 | Plasmid replicons facilitating horizontal gene transfer |
Extended-spectrum β-lactamase (ESBL) producing E. coli isolates showed significantly higher prevalence of both antimicrobial resistance genes and virulence factors compared to non-ESBL isolates [10]. The study identified a strong correlation (p < 0.001) between the presence of plasmid replicons (IncFIB, IncFII) and the co-occurrence of resistance and virulence genes, highlighting the role of mobile genetic elements in the dissemination of these traits.
Phylogenetic analysis revealed that ESBL E. coli isolates from cattle were predominantly classified within phylogroups A and B1, with sequence types ST10, ST101, and ST69 being most common [10]. The genetic diversity of E. coli in dairy environments, coupled with the extensive horizontal gene transfer mediated by plasmids, integrons, and insertion sequences, creates a complex ecological landscape where virulence and resistance traits freely circulate between commensal and pathogenic strains.
Research Reagent Solutions for Virulence Studies
The following research reagents represent essential tools for investigating virulence factors and niche-specific adaptations in bacterial pathogens:
Table 4: Essential Research Reagents for Studying Bacterial Virulence
| Reagent/Resource | Specification | Research Application | Key Features |
|---|---|---|---|
| VFDB Database | Virulence Factor Database (http://www.mgc.ac.cn/VFs/) | Comprehensive virulence factor annotation | Curated information on VFs from medically significant pathogens; integrated anti-virulence compound data [11] [7] |
| dbCAN2 | HMMER-based annotation tool | Carbohydrate-active enzyme identification | Mapping to CAZy database with hmm_eval 1e-5 filtering parameter [2] |
| CARD Database | Comprehensive Antibiotic Resistance Database | Antibiotic resistance gene annotation | Detection of resistance mechanisms across antibiotic classes [2] |
| AMPHORA2 | Marker gene-based phylogenetic tool | Phylogenetic tree construction | Identifies 31 universal single-copy genes for robust phylogeny [2] |
| RNAprep pure Bacteria Kit | Takara Bio | Bacterial RNA extraction | High-quality RNA for virulence gene expression studies [8] |
| TB Green Premix Ex Taq II | Takara Bio | Quantitative PCR | SYBR Green-based detection of virulence gene expression [8] |
The VFDB deserves special emphasis as it has recently been enhanced to include information on anti-virulence compounds, providing valuable resources for drug design and repurposing [11]. The database currently contains 902 individual anti-virulence compounds across 17 superclasses, with detailed information on their chemical structures, molecular targets, and mechanisms of action. This integration of virulence factor data with therapeutic compound information bridges the gap between chemists and microbiologists, supporting the development of novel anti-virulence strategies.
The comparative analysis of virulence factors across human, animal, and environmental niches reveals fundamental principles of bacterial evolution and adaptation. Human-associated pathogens demonstrate specialized adaptations for immune evasion and host interaction, while environmental isolates maintain metabolic versatility for diverse conditions. Animal reservoirs serve as crucial interfaces where virulence and resistance traits exchange between commensal and pathogenic bacteria.
The methodological framework presented here, integrating comparative genomics, phenotypic characterization, and environmental stress studies, provides a robust foundation for investigating niche-specific adaptations. As bacterial pathogens continue to evolve in response to antimicrobial pressure and changing ecological conditions, understanding these dynamic evolutionary relationships remains critical for developing effective interventions against infectious diseases.
Future research directions should focus on the convergence of hypervirulence and multidrug resistance, particularly the mechanisms by which pathogens maintain both traits without fitness trade-offs. Additionally, exploring how virulence regulation responds to niche-specific signals will yield insights into bacterial decision-making processes during infection. The developing field of anti-virulence therapy, targeting specific virulence factors without affecting bacterial growth, represents a promising alternative to conventional antibiotics that may exert less selective pressure for resistance development [11].
Bacterial pathogens demonstrate a remarkable capacity to thrive in diverse ecological niches, from environmental reservoirs to human hosts. This adaptability is driven by dynamic genomic evolution, where gene acquisition, gene loss, and genome reduction serve as fundamental mechanisms enabling bacterial survival and specialization. Understanding these processes is crucial for elucidating pathogenic potential, predicting emerging threats, and developing novel antimicrobial strategies [3] [2]. These genomic alterations facilitate the fine-tuning of bacterial physiology to specific host environments, allowing pathogens to circumvent immune defenses, access novel nutrient sources, and establish persistent infections [12].
The study of these adaptive strategies has been revolutionized by comparative genomics, which enables researchers to systematically analyze genetic differences across thousands of bacterial isolates from diverse sources. Recent large-scale studies examining 4,366 high-quality bacterial genomes have revealed that different bacterial phyla exhibit distinct preferential strategies for host adaptation [3] [2]. For instance, while Pseudomonadota frequently utilize gene acquisition, Actinomycetota and Bacillota often employ genome reduction as their primary adaptive mechanism [2]. This review provides a comparative analysis of these three fundamental genomic strategies, supported by experimental data and methodologies relevant to virulence factor research across ecological niches.
Comparative Analysis of Genomic Adaptation Strategies
Table 1: Characteristics of Primary Genomic Adaptation Strategies
| Adaptation Strategy | Primary Mechanism | Impact on Genome Size | Representative Genera/Phyla | Key Virulence Associations |
|---|---|---|---|---|
| Gene Acquisition | Horizontal gene transfer of virulence factors, antibiotic resistance genes, and pathogenicity islands | Increase or maintenance | Pseudomonadota, Escherichia, Staphylococcus | Acquisition of toxin genes, adhesion factors, immune evasion proteins [3] [2] |
| Gene Loss | Loss of non-essential genes through deletion mutations | Decrease | Burkholderia, Mycoplasma | Streamlined metabolism, loss of environmental persistence capabilities [12] [2] |
| Genome Reduction | Extensive gene loss and pseudogene accumulation through reductive evolution | Significant decrease | Actinomycetota, Bacillota, obligatory intracellular pathogens | Enhanced host dependence, specialized virulence factor retention [13] [2] |
Table 2: Niche-Specific Distribution of Virulence and Resistance Genes
| Ecological Niche | Prevalent Adaptive Strategy | Virulence Factor Enrichment | Antibiotic Resistance Gene Prevalence | Notable Genomic Features |
|---|---|---|---|---|
| Human Clinical | Gene acquisition | Immune modulation and adhesion factors [2] | High, particularly fluoroquinolone resistance [3] [2] | Specialized secretion systems, toxin genes |
| Animal Host | Mixed strategies (acquisition and loss) | Adhesion and colonization factors | Significant reservoir of resistance genes [3] [2] | Host-specific adaptation genes |
| Environmental | Gene loss/genome reduction | Metabolic and transcriptional regulation genes [2] | Lower compared to clinical isolates [3] | Stress response genes, environmental sensing systems |
Gene Acquisition: Expanding Pathogenic Potential
Gene acquisition through horizontal gene transfer represents a fundamental strategy for rapid bacterial adaptation to new niches. This process enables bacteria to incorporate novel genetic material, including virulence factors, antibiotic resistance genes, and metabolic pathway components, from distantly related organisms [3] [2].
Mechanisms and Experimental Evidence
Horizontal gene transfer occurs primarily through three mechanisms: conjugation (direct cell-to-cell transfer), transformation (uptake of environmental DNA), and transduction (viral-mediated transfer). Comparative genomic studies have revealed that human-associated bacteria, particularly from the phylum Pseudomonadota, exhibit higher detection rates of carbohydrate-active enzyme genes and virulence factors related to immune modulation and adhesion, indicating co-evolution with the human host through gene acquisition [2].
Staphylococcus aureus provides a compelling example of this adaptive strategy, having acquired a variety of host-specific genes through horizontal transfer. These include immune evasion factors in equine hosts, methicillin resistance determinants in human-associated strains, heavy metal resistance genes in porcine hosts, and lactose metabolism genes in strains adapted to dairy cattle [2]. This acquisition of niche-specific genes enables rapid adaptation to selective pressures, including antibiotic exposure and host immune defenses.
Experimental identification of acquired genes typically involves comparative genomic analysis using tools such as BLAST-based orthology detection and phylogenetic reconstruction to identify genes with discordant evolutionary histories relative to the core genome. The Scoary algorithm, combined with machine learning approaches, can identify niche-associated genes with high predictive accuracy [2].
Gene Loss and Genome Reduction: Strategic Simplification
While gene acquisition expands genomic repertoire, strategic gene loss and genome reduction represent alternative adaptation strategies that optimize bacterial fitness by eliminating unnecessary genetic material [13] [2].
Adaptive Stasis in Genome-Reduced Bacteria
Freshwater genome-reduced bacteria (≤2.1 Mbp) exhibit extended periods of adaptive stasis, characterized by significantly higher levels of sequence conservation and invariance in their secreted proteomes compared to their larger-genomed counterparts [13]. This contrasts with the dominant paradigm of continuous evolution through niche adaptation and reflects a different evolutionary strategy where conservation of essential functions takes precedence over genetic innovation.
In these genome-reduced bacteria, secreted proteomes show a combination of low functional redundancy and high selection pressure, resulting in significantly higher levels of conservation [13]. This pattern suggests that even mutations that do not impact amino acid identity may incur a fitness cost, possibly by altering optimal gene expression levels crucial for survival in their specific niche.
Case Studies in Pathogenic Adaptation
Burkholderia mallei illustrates how genome reduction facilitates the transition from environmental saprophyte to obligate pathogen. Evolving from B. pseudomallei, B. mallei underwent substantial genome reduction through insertion sequence-mediated deletions, losing genes necessary for survival in soil environments while retaining virulence factors essential for mammalian pathogenesis [12]. This reductive evolution resulted in increased host dependence but enhanced pathogenic specialization.
Similarly, Mycoplasma genitalium has undergone extensive genome reduction, including the loss of genes involved in amino acid biosynthesis and carbohydrate metabolism, enabling the bacterium to reallocate limited resources toward maintaining a mutualistic relationship with its host [2]. This strategic gene loss reflects adaptive optimization to a specific host niche.
Experimental Methodologies for Studying Genomic Adaptation
Comparative Genomic Workflow
Figure 1: Experimental Workflow for Comparative Genomic Analysis
Detailed Methodological Protocols
Genome Collection and Quality Control
Researchers conducting comparative genomic analysis begin with stringent quality control procedures. As demonstrated in recent large-scale studies, this involves:
- Genome Sourcing: Obtaining metadata for bacterial pathogens from comprehensive databases such as gcPathogen, which contains information on over 1 million human pathogens [3] [2].
- Quality Filtering: Retaining only high-quality genome sequences with N50 ≥50,000 bp, completeness ≥95%, and contamination <5% as evaluated by CheckM [3] [2].
- Niche Annotation: Categorizing genomes based on detailed isolation source metadata into human, animal, or environmental niches [2].
- Redundancy Reduction: Calculating genomic distances using Mash and performing Markov clustering to remove highly similar genomes (distance ≤0.01) [2].
Functional and Virulence Annotation
Comprehensive functional annotation enables researchers to identify adaptive genes across different niches:
- Open Reading Frame Prediction: Using Prokka v1.14.6 for rapid prokaryotic genome annotation [3] [2].
- Functional Categorization: Mapping predicted ORFs to the Cluster of Orthologous Groups (COG) database using RPS-BLAST with e-value threshold of 0.01 and minimum coverage of 70% [3] [2].
- Carbohydrate-Active Enzyme Annotation: Applying dbCAN2 to map ORFs to the CAZy database using HMMER with parameter hmm_eval 1e-5 [3] [2].
- Virulence Factor Identification: Utilizing ABRicate v1.0.1 to map bacterial genomes to the Virulence Factor Database (VFDB) for systematic identification of virulence genes [3].
Identification of Adaptive Genes
Advanced computational methods enable the detection of niche-specific adaptive genes:
- Phylogenetic Analysis: Constructing maximum likelihood trees from 31 universal single-copy genes using FastTree v2.1.11 after alignment with Muscle v5.1 [2].
- Population Clustering: Performing k-medoids clustering using the pam function from the R cluster package to identify evolutionarily coherent groups [2].
- Association Testing: Applying the Scoary algorithm to identify genes significantly associated with specific ecological niches while accounting for population structure [2].
- Machine Learning Validation: Using machine learning approaches (e.g., random forests) to validate the predictive power of identified adaptive genes for niche classification [2].
Table 3: Essential Research Reagents and Databases for Genomic Adaptation Studies
| Resource | Type | Primary Function | Application in Adaptation Research |
|---|---|---|---|
| VFDB (Virulence Factor Database) | Database | Curated repository of bacterial virulence factors | Systematic identification of virulence factors across bacterial genomes [7] |
| CARD (Comprehensive Antibiotic Resistance Database) | Database | Antibiotic resistance gene reference | Detection and annotation of resistance genes in genomic data [3] [2] |
| COG (Cluster of Orthologous Groups) | Database | Phylogenetic classification of proteins encoded in complete genomes | Functional categorization of gene products [3] [2] |
| CAZy (Carbohydrate-Active Enzymes) | Database | Specialist database for enzymes that build and break down complex carbohydrates | Identification of carbohydrate metabolism adaptation [3] [2] |
| Prokka | Software Tool | Rapid prokaryotic genome annotation | Automated annotation of genomic features in bacterial genomes [3] [2] |
| Scoary | Algorithm | Pan-genome-wide association study tool | Identification of genes associated with specific niches or phenotypes [2] |
| CheckM | Software Tool | Assess genome quality and completeness | Quality control of genomic datasets prior to comparative analysis [2] |
Implications for Virulence Factor Research and Therapeutic Development
Understanding genomic adaptation strategies provides crucial insights for antimicrobial development and infectious disease management. The distinct distribution of virulence factors across ecological niches highlights potential targets for anti-virulence therapies [7]. For instance, targeting niche-specific adhesion factors or immune evasion proteins could disrupt host colonization without exerting the strong selective pressure associated with conventional antibiotics [14] [7].
The identification of animal hosts as significant reservoirs of antibiotic resistance genes underscores the importance of the One Health approach to infectious disease control, which integrates human, animal, and environmental health [3] [2]. Furthermore, the discovery of human host-specific signature genes, such as hypB, which may regulate metabolism and immune adaptation in human-associated bacteria, reveals potential targets for novel therapeutic interventions [2].
Recent advances in CRISPR-based therapeutics also offer promising avenues for directly targeting bacterial virulence factors or reversing antibiotic resistance [15]. As our understanding of genomic adaptation mechanisms deepens, so too does our capacity to develop precisely targeted antimicrobial strategies that disrupt pathogenic specialization while minimizing collateral damage to commensal microbiota.
The concept of protozoan predation serving as a "training ground" for bacterial virulence is grounded in the coincidental evolution hypothesis, which proposes that virulence factors arose as a response to environmental selective pressures, such as predation, rather than for virulence per se [16] [17]. For opportunistic pathogens that transit in the environment between hosts, interactions with bacterivorous protists are a major evolutionary driver. The defense mechanisms bacteria develop to resist protozoan predation are often functionally identical to the traits required to survive within human phagocytic immune cells, such as macrophages [17]. This review provides a comparative analysis of how predation pressure shapes bacterial virulence across different ecological niches and bacterial species, synthesizing key experimental data to guide future research and therapeutic development.
Comparative Analysis of Anti-Predator Virulence Mechanisms
Bacteria have evolved a diverse arsenal of mechanisms to resist protozoan predation, many of which have been co-opted for pathogenesis in human hosts. The table below summarizes key virulence factors, their roles in anti-predator defense, and their impact on human virulence.
Table 1: Dual Role of Bacterial Anti-Predator Mechanisms and Virulence Factors
| System/Mechanism | Bacterium | Role in Anti-Predation | Role in Human Virulence | Key Experimental Models |
|---|---|---|---|---|
| Type III Secretion System (T3SS) | Pseudomonas aeruginosa | Kills Acanthamoeba castellanii [16] | Causes pneumonia [16] | Acanthamoeba castellanii, mouse lung infection |
| Legionella pneumophila | Enables intracellular parasitism of amoeba [16] | Causes legionellosis [16] | Acanthamoeba spp., human monocytes | |
| Escherichia coli | Promotes survival inside A. castellanii [16] | Causes diarrheal disease [16] | A. castellanii co-culture | |
| Type VI Secretion System (T6SS) | Vibrio cholerae | Cytotoxic against Dictyostelium discoideum [16] | Causes cholera & gastroenteritis [16] | D. discoideum plaque assay |
| Violacein Pigment | Chromobacterium violaceum | Induces rapid protist cell death [16] | Opportunistic pathogen [16] | Co-culture with various protists |
| Shiga Toxin | Escherichia coli O157:H7 | Kills Tetrahymena thermophila [16] [18] | Causes hemorrhagic colitis [16] | T. thermophila predation assay |
| Biofilm Formation | P. aeruginosa, V. cholerae | Physical barrier against ingestion; promoted by predator cues [16] [17] | Chronic lung infections, antibiotic resistance [16] [19] | Flow cells, confocal microscopy, wax moth larvae |
| Intracellular Survival | L. pneumophila, V. cholerae | Prevents phagosome-lysosome fusion; resists digestion [16] [17] | Survival within human macrophages [17] | Acanthamoeba & Dictyostelium co-culture |
The experimental evidence reveals a fundamental distinction between the strategies of intracellular and extracellular pathogens. Intracellular pathogens like Legionella pneumophila rely on active invasion and sophisticated intracellular maneuvers, such as blocking phagosome-lysosome fusion, to survive and replicate within the protist [16] [17]. In contrast, extracellular pathogens like Pseudomonas aeruginosa often utilize toxin secretion and biofilm formation to avoid internalization altogether [17]. This ecological specialization has direct implications for their pathogenicity in humans.
Key Experimental Models and Data
Experimental Evolution: Protist Predation and Virulence Attenuation
Direct experimental tests have been crucial in validating the link between predation and virulence evolution. A key study investigated how the ciliate Tetrahymena thermophila and PNM phage, both individually and in combination, shape the evolution of Pseudomonas aeruginosa PAO1 virulence, measured as mortality in wax moth larvae [18].
Table 2: Summary of Experimental Evolution and Virulence Outcomes
| Selection Pressure | Evolved Bacterial Phenotype | Impact on Virulence (in Wax Moth Larvae) | Associated Pleiotropic Cost |
|---|---|---|---|
| Protist Predation Alone | Selected for small, inedible colony variants; increased biofilm formation [18] | Attenuated virulence [18] | Reduced growth rate in absence of enemies [18] |
| Phage Parasitism Alone | No significant phenotypic change observed [18] | No significant change in virulence [18] | Not detected |
| Protist & Phage Combined | Phage constrained antipredator defense (biofilm formation) [18] | Constrained protist-driven virulence attenuation [18] | Reduced growth cost associated with anti-protist defense [18] |
This study demonstrates that protist selection can be a strong coincidental driver of attenuated bacterial virulence, and that phages can constrain this effect due to their impact on population dynamics and conflicting selection pressures [18]. The pleiotropic link between reduced growth and lower virulence suggests a fitness trade-off that can be exploited therapeutically.
Ecological Drivers of Protozoa-Resisting Bacteria (PRB)
The selection for PRB in natural environments is influenced by nutrient availability and predation pressure. An enrichment-dilution experiment using natural lake water revealed how these factors favor different PRB with distinct ecological strategies [20].
Table 3: Ecological Drivers of Protozoa-Resisting Bacteria (PRB) in Aquatic Systems
| PRB Genus | Response to High Predation-Pressure | Response to Nutrient Enrichment/Disturbance | Ecological Strategy / Niche |
|---|---|---|---|
| Mycobacterium | Strong positive effect (e.g., >13-fold increase with 50% higher predation) [20] | Negative association with enrichment [20] | Specialist in high-predation, stable environments |
| Pseudomonas | Weak, less important effect [20] | Strong positive effect; dominates community (30-50% of reads) [20] | Generalist in disturbed, nutrient-rich environments |
| Rickettsia | Apparent positive effect (co-occurred with predators) [20] | Effect not statistically significant [20] | Specialist, likely dependent on host association |
The findings indicate that PRB with different ecological strategies can be expected in waters of varying nutrient levels. Pseudomonas thrives in enriched, disturbed systems, whereas Mycobacterium is favored under high, stable predation pressure [20]. This ecological understanding helps predict the environmental conditions that may lead to the enrichment of potential pathogens.
Methodologies: Core Experimental Protocols
To facilitate replication and further research, here are detailed methodologies for key experiments cited in this field.
Protocol 1: Experimental Evolution with Dual Enemies
This protocol is adapted from the study investigating the concurrent impact of protist and phage selection on P. aeruginosa evolution [18].
- Bacterial Strain: Pseudomonas aeruginosa PAO1 (ATCC 15692).
- Enemies: Tetrahymena thermophila (protist predator) and PNM phage (bacterial virus, Podoviridae family).
- Culture Conditions: 6 ml of 1% King's Medium B (diluted KB) in 25 ml glass vials.
- Experimental Design:
- Set up a full factorial design with four treatments: Bacterium alone (control), Bacterium + Phage, Bacterium + Protist, Bacterium + Protist + Phage.
- Replicate each treatment (e.g., n=5 microcosms).
- Inoculate all microcosms with ~10^5 cells of PAO1.
- Add enemies according to treatment: ~3.6x10^3 phage particles and/or ~250 protist cells.
- Selection Regime:
- Incubate microcosms at 28°C without shaking.
- Every 4 days, vortex microcosms and transfer 1 μL of culture to 6 ml of fresh medium. This serial passage is repeated for a total of 5 transfers (24 days).
- At each transfer, monitor bacterial density (by spectrophotometry and plating), phage density (by plaque assay), and protist density (by direct microscopy).
- Post-Selection Analysis:
- After the final transfer, isolate bacterial clones from predators and phages by plating on KB agar.
- Measure evolved phenotypes: defense against protists and phages, biofilm formation, growth rate in enemy-free medium, and virulence in an animal model (e.g., wax moth larvae).
Protocol 2: Assessing Virulence in Wax Moth Larvae
This in vivo model provides a rapid and ethical method to quantify bacterial virulence [18].
- Host Organism: Last instar larvae of the Greater Wax Moth (Galleria mellonella).
- Infection Procedure:
- Grow ancestral and evolved bacterial isolates to mid-log phase.
- Wash and resuspend bacteria in a saline solution (e.g., PBS) to a standardized concentration (e.g., 10^5 - 10^6 CFU/mL).
- Inject a defined volume (e.g., 10 μL) of the bacterial suspension into the larval hemocoel via a proleg using a microsyringe.
- Include a control group injected with saline only.
- Virulence Measurement:
- Incubate injected larvae at a controlled temperature (e.g., 37°C) and monitor survival every 12-24 hours for up to 5 days.
- Virulence is quantified as the proportion of dead larvae over time, and results can be analyzed using Kaplan-Meier survival curves and statistical tests like the log-rank test.
Visualizing Signaling Pathways and Experimental Workflows
Bacterial Anti-Predator Signaling and Virulence Pathways
Diagram 1: Bacterial anti-predator signaling and virulence pathways. Protozoan predation selects for and induces multiple bacterial defense systems, which function coincidentally as virulence factors during human infection. Key regulatory systems like Quorum Sensing (QS) coordinate the expression of these traits.
Experimental Evolution Workflow with Dual Enemies
Diagram 2: Experimental evolution workflow with dual enemies. P. aeruginosa is evolved under different selection regimes (predation, parasitism, both, or none). After serial passaging, evolved clones are isolated and analyzed for a suite of phenotypic traits, including virulence in an animal model.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents and Models for Studying Predation-Driven Virulence
| Reagent / Model System | Category | Function in Research | Specific Example Use Case |
|---|---|---|---|
| Acanthamoeba castellanii | Protist Model | Mimics macrophage phagocytosis; selective force for intracellular pathogens [16] [17] | Co-culture with L. pneumophila to study phagosome maturation blocking [16] |
| Dictyostelium discoideum | Protist Model | Genetic model for phagocytosis; identifies virulence factors conserved in metazoans [16] [17] | Plaque assay with V. cholerae to identify T6SS mutants [16] |
| Tetrahymena thermophila | Protist Model | Bacterivorous ciliate for experimental evolution and studying toxin resistance [18] [20] | Predation assay to demonstrate Shiga toxin's anti-protozoal function [18] |
| PNM Phage & similar | Viral Parasite | Adds multi-enemy selection pressure; constrains evolution of anti-protist traits [18] | Experimental evolution of P. aeruginosa to study trade-offs in multi-enemy environments [18] |
| Galleria mellonella | Animal Model | High-throughput, ethical in vivo model for quantifying bacterial virulence [18] | Measuring larval survival after injection with evolved P. aeruginosa clones [18] |
| Joint Species Distribution Model (JSDM) | Analytical Tool | Statistical modeling to quantify effects of environmental variables on PRB abundance [20] | Determining the impact of predation-pressure vs. nutrients on Mycobacterium and Pseudomonas [20] |
Implications for Drug Development and Future Research
The understanding that virulence is often a by-product of environmental adaptation has profound implications for anti-virulence drug development [19]. Targeting virulence factors that are primarily maintained by environmental pressures, rather than host infection, may result in lower selective pressure for resistance in the clinical setting [19]. Furthermore, the pleiotropic costs associated with anti-predator defenses, such as reduced growth rates, suggest that disarming these virulence factors could push pathogens back toward a less fit state [18]. Future research should focus on quantifying the strength of selection imposed by diverse protozoan communities in natural reservoirs and further elucidate the genetic and metabolic trade-offs that link anti-predator defense to virulence. This ecological-evolutionary perspective will be crucial for predicting and mitigating the emergence of new opportunistic pathogens.
Tools for Discovery: Genomic and Computational Methods for Profiling Virulence
Comparative Genomics Frameworks for Large-Scale Pathogen Analysis
Comparative genomics has become an indispensable methodology for unraveling the genetic basis of pathogen virulence, host adaptation, and ecological niche specialization. By analyzing genomic variations across diverse bacterial populations, researchers can identify key virulence factors (VFs) and antibiotic resistance genes that enable pathogens to colonize specific hosts and environments [3]. This approach is particularly valuable for investigating the distribution of virulence factors across different ecological niches—a research area with significant implications for understanding disease pathogenesis, predicting emerging threats, and developing targeted therapeutic interventions.
The integration of large-scale genomic datasets with advanced bioinformatics tools has enabled unprecedented insights into the evolutionary mechanisms driving pathogen diversification. Studies of bacterial pathogens isolated from human, animal, and environmental sources have revealed niche-specific genomic signatures and adaptive strategies, highlighting the complex interplay between pathogen genetics and host environment [3] [2]. This guide provides a systematic comparison of current comparative genomics frameworks, their methodological approaches, and applications in virulence factor research, offering researchers a comprehensive resource for selecting appropriate methodologies for large-scale pathogen analysis.
Key Frameworks and Databases for Virulence Factor Analysis
Core Databases for Virulence Factor Annotation
Table 1: Major Databases for Virulence Factor Analysis in Comparative Genomic Studies
| Database Name | Primary Function | Key Features | Data Scope | Applications in Comparative Genomics |
|---|---|---|---|---|
| VFDB (Virulence Factor Database) | VF identification and annotation | Curated collection of experimentally verified VFs; integrated anti-virulence compound data | 3581 verified VFGs; 62,332 non-redundant orthologues and alleles [11] [21] | Reference-based VF annotation; pathobiont VF profiling; cross-niche VF distribution analysis |
| VFDB 2.0 (Expanded) | VF orthologue and allele identification | Includes ssANI-based orthologues/alleles; mobile VF annotation; host taxonomy | 62,332 VFG sequences across 135 species [21] | High-resolution VF tracking; mobile genetic element-associated VF identification |
| CARD (Comprehensive Antibiotic Resistance Database) | Antibiotic resistance gene annotation | Curated resistance determinants and resistance mechanisms | Not specified in search results | Co-occurrence analysis of VFs and AMR genes; resistance gene transfer studies |
| COG (Cluster of Orthologous Groups) | Functional categorization | Protein classification based on phylogenetic relationships | Not specified in search results | Functional enrichment analysis across niches; core genome analysis |
| dbCAN2 | Carbohydrate-active enzyme annotation | HMM-based CAZy annotation; enzyme class prediction | Not specified in search results | Nutrient acquisition strategy comparison; host adaptation analysis |
Analytical Frameworks and Toolkits
Table 2: Computational Frameworks for Large-Scale Pathogen Genomics
| Framework/Tool | Methodological Approach | Key Advantages | Performance Metrics | Ideal Use Cases |
|---|---|---|---|---|
| MetaVF Toolkit | VF profiling based on VFDB 2.0; TSI filtering | Species-level VFG identification; mobile VF prediction; bacterial host attribution | TDR >97%; FDR <4.000767e-05% at 90% TSI [21] | Metagenomic VF profiling; pathobiont carrier identification; cross-niche VF comparison |
| PLMVF | Protein language model (ESM-2) with ensemble learning; structural similarity integration | Remote homology detection; 3D structural feature incorporation; TM-score prediction | 86.1% accuracy; outperforms sequence-only methods [22] | Novel VF prediction; functional annotation of hypothetical proteins |
| Traditional Comparative Genomics Pipeline | Phylogenetic analysis; COG/CAZy annotation; VFDB/CARD mapping | Established methodology; comprehensive functional profiling; phylogenetic context | Varies with dataset size and parameters [3] [2] | Niche-specific gene identification; evolutionary studies; broad-scale adaptation analysis |
| Scoary with Machine Learning | Gene presence/absence association; machine learning classification | Identification of niche-associated genes; predictive model building | 0.63 average silhouette coefficient at k=8 clusters [3] | Host-specific gene identification; predictive model development |
Experimental Protocols for Cross-Niche Virulence Factor Analysis
Protocol 1: Large-Scale Comparative Genomic Analysis Across Ecological Niches
Objective: To identify niche-specific virulence factors and adaptive mechanisms across human, animal, and environmental pathogens.
Methodology Details:
Genome Dataset Curation
- Source 4,366 high-quality bacterial genomes with comprehensive metadata from databases such as gcPathogen [3] [2]
- Implement stringent quality control: completeness ≥95%, contamination <5%, N50 ≥50,000 bp
- Annotate ecological niches (human, animal, environment) based on isolation source and host information
- Remove redundant genomes using Mash distances (≤0.01) and Markov clustering
Phylogenetic Framework Construction
Functional and Virulence Annotation
- Predict open reading frames with Prokka v1.14.6
- Annotate functional categories using COG database (RPS-BLAST, e-value 0.01, 70% coverage)
- Identify carbohydrate-active enzymes with dbCAN2 (HMMER, hmm_eval 1e-5)
- Annotate virulence factors using VFDB and antibiotic resistance genes using CARD via ABRicate v1.0.1 [3]
Statistical Analysis and Machine Learning
- Perform enrichment analysis for functional categories across niches
- Identify niche-associated genes using Scoary
- Apply machine learning algorithms (e.g., Random Forest) to build predictive models for niche specificity [3]
Protocol 2: Metagenomic Virulence Factor Profiling with MetaVF
Objective: To profile virulence factor genes in metagenomic data with species-level resolution and mobile genetic element association.
Methodology Details:
Data Preprocessing and Alignment
- Process clean metagenomic reads or metagenome-assembled genomes (MAGs)
- For short reads: map against expanded VFDB 2.0 alignment dataset
- For long HiFi reads or MAGs: perform nucleotide BLAST against pathogenic alignment dataset [21]
Stringent Filtering with Tested Sequence Identity (TSI)
- Apply TSI threshold (90%) determined using artificial metagenomic datasets
- Filter VF-mapped reads to achieve true discovery rate >97% and false discovery rate <4.000767e-05% [21]
- Select best BLAST hits based on identity and coverage
Quantification and Normalization
- Count filtered VF-mapped reads
- Normalize by gene length and sequencing depth to transcripts per million (TPM)
- Annotate VF clusters, mobility, bacterial host taxonomy, and VF categories [21]
Cross-Niche Comparative Analysis
- Compare VF abundance and diversity across different ecological niches
- Identify mobile VFs associated with plasmids, prophages, and integrative conjugative elements
- Attribute VFs to specific bacterial hosts at species level
Protocol 3: Machine Learning-Based Virulence Factor Prediction with PLMVF
Objective: To accurately identify novel virulence factors using protein language models and structural similarity metrics.
Methodology Details:
Feature Extraction
- Extract sequence embeddings using ESM-2 protein language model
- Generate 3D structural features using ESMFold
- Calculate true TM-scores based on protein structures [22]
Structural Similarity Prediction
- Train TM-predictor model on known structural similarities
- Predict TM-scores to capture remote homology relationships
- Concatenate ESM-2 sequence features with predicted TM-score features [22]
Ensemble Model Training
- Utilize balanced dataset (3,000 VFs and 3,000 non-VFs for training)
- Train ensemble model with combined feature set
- Apply Knowledge-Augmented Network (KAN) for final VF prediction [22]
Validation and Performance Assessment
- Test on independent dataset (576 VFs and 576 non-VFs)
- Evaluate using accuracy, precision, recall, and F1-score
- Compare against existing tools (VirulentPred, MP3, DeepVF, DTVF) [22]
Workflow Visualization
Figure 1: Comparative Genomics Workflow for Cross-Niche Virulence Analysis. This workflow outlines the key steps in identifying niche-specific virulence factors, from sample collection through to computational analysis and final gene identification.
Figure 2: MetaVF Workflow for Metagenomic Virulence Factor Profiling. This specialized workflow details the process for identifying and quantifying virulence factors directly from metagenomic data, incorporating stringent filtering and comprehensive annotation.
Table 3: Key Research Reagent Solutions for Comparative Genomic Studies of Virulence Factors
| Reagent/Resource | Specific Function | Application Context | Key Features/Benefits |
|---|---|---|---|
| VFDB 2.0 Database | Comprehensive VF reference | VF annotation in genomic and metagenomic studies | 62,332 non-redundant VF sequences; mobile VF annotation; host taxonomy [21] |
| MetaVF Toolkit | VF profiling from metagenomes | Direct VF analysis from sequencing data without cultivation | Species-level resolution; mobile genetic element association; high TDR (>97%) [21] |
| PLMVF Model | Novel VF prediction | Identification of uncharacterized VFs using AI | Incorporates structural similarity; 86.1% accuracy; remote homology detection [22] |
| CheckM | Genome quality assessment | Quality control in genome curation | Estimates completeness and contamination; essential for dataset standardization [3] |
| AMPHORA2 | Phylogenetic marker gene extraction | Phylogenetic tree construction for evolutionary analysis | 31 universal single-copy genes; robust phylogenetic framework [3] |
| Artificial Metagenomic Datasets (AMSD) | Method validation and benchmarking | Tool performance evaluation | Defined VF abundance and mutation rates; enables TSI optimization [21] |
| Prokka v1.14.6 | Rapid genome annotation | ORF prediction in bacterial genomes | Standardized annotation pipeline; integrates multiple databases [3] |
Discussion: Applications and Insights from Cross-Niche Virulence Factor Studies
Comparative genomic frameworks have revealed fundamental insights into how bacterial pathogens adapt to different ecological niches through distinct genetic strategies. Human-associated bacteria, particularly from the phylum Pseudomonadota, demonstrate higher prevalence of carbohydrate-active enzyme genes and virulence factors related to immune modulation and adhesion, suggesting co-evolution with human hosts [3]. In contrast, environmental bacteria show greater enrichment in metabolic and transcriptional regulation genes, highlighting their adaptability to diverse environmental conditions. Clinical isolates exhibit higher rates of antibiotic resistance genes, particularly those conferring fluoroquinolone resistance, while animal hosts serve as important reservoirs of resistance genes [3] [2].
The integration of machine learning with comparative genomics has enabled the identification of key host-specific bacterial genes, such as hypB, which potentially plays crucial roles in regulating metabolism and immune adaptation in human-associated bacteria [3]. These findings underscore the power of comparative genomic approaches in unraveling the genetic basis of host-pathogen interactions and provide valuable evidence to inform pathogen transmission control, infection management, and antibiotic stewardship policies.
Emerging methodologies that incorporate structural similarity and remote homology detection, such as PLMVF, offer promising avenues for identifying novel virulence factors that evade detection by traditional sequence-based methods [22]. As these frameworks continue to evolve, they will undoubtedly enhance our ability to predict pathogenic potential, track virulence transmission across reservoirs, and develop targeted interventions against problematic pathogens across the One Health continuum.
The study of bacterial pathogenesis has been transformed by the advent of high-throughput sequencing and specialized bioinformatics databases. For researchers investigating the comparison of virulence factors across ecological niches, four databases stand out as indispensable tools: the Virulence Factor Database (VFDB), the Comprehensive Antibiotic Resistance Database (CARD), the Clusters of Orthologous Genes (COG) database, and the Carbohydrate-Active enZYmes Database (CAZy). These resources provide structured, curated knowledge that enables scientists to move beyond simple sequence analysis to functional prediction and evolutionary insight. VFDB and CARD directly catalog the genetic determinants of pathogenicity and treatment failure, while COG and CAZy provide essential functional context for genomic data, revealing how pathogens interact with their environments and hosts. Together, they form an integrated toolkit for deciphering the complex relationships between genetic content, ecological niche, and pathogenic potential, ultimately accelerating the discovery of novel therapeutic targets in an era of escalating antimicrobial resistance.
Core Characteristics and Applications
Table 1: Core Database Characteristics and Applications
| Database | Primary Focus | Year Founded | Last Update | Key Content Metrics | Primary Application in Research |
|---|---|---|---|---|---|
| VFDB | Virulence Factors (VFs) & Anti-Virulence Compounds | Over 20 years ago | 2024 | 902 anti-virulence compounds from 262 studies; covers 32 medically important bacterial genera [11]. | Identifying virulence mechanisms, screening for anti-virulence drug targets, and understanding host-pathogen interactions [11]. |
| CARD | Antibiotic Resistance Genes & Mechanisms | Information missing | Information missing | Information missing | Predicting antibiotic resistance phenotypes from genomic data and surveillance of resistance gene dissemination. |
| COG | Phylogenetic Protein Classification & Functional Annotation | 1997 | 2025 | 4,981 COGs covering 2,296 prokaryotic genomes (2,103 bacteria, 193 archaea) [23]. | Functional annotation of genomes, evolutionary studies, and identification of core/pangenome components [24] [23]. |
| CAZy | Carbohydrate-Active Enzymes (CAZymes) | 1998 | 2025 | 36,364 bacterial, 587 archaeal, and 2,002 eukaryotic genomes analyzed [25] [26]. | Profiling metabolic capabilities (CAZyme), understanding nutrient acquisition, and studying host-glycan interactions [25] [27]. |
Quantitative Coverage and Taxonomic Scope
Table 2: Taxonomic and Genomic Coverage
| Database | Taxonomic Scope | Genomic Coverage | Classification System |
|---|---|---|---|
| VFDB | Focused on medically important pathogens (32 genera) [11]. | Not explicitly stated, but integrates data from public genomes. | Virulence factor categories (e.g., adhesion, biofilm, toxins) and anti-virulence compound superclasses [11]. |
| CARD | Information missing | Information missing | Information missing |
| COG | Bacteria and Archaea (primarily) [24] [23]. | 2,296 prokaryotic genomes (typically one per genus) [23]. | 4,981 Clusters of Orthologous Genes (COGs), grouped into functional categories and pathways [23]. |
| CAZy | All kingdoms of life (Bacteria, Archaea, Eukaryota, Viruses) [25] [26]. | 36,364 bacterial, 587 archaeal, 2,002 eukaryotic, and 501 viral genomes [26]. | Family-based classification (GHs, GTs, PLs, CEs, AAs, CBMs) [25] [27]. |
Database Integration in Experimental Research
A Standard Workflow for Comparative Genomics
Investigating virulence across ecological niches requires a structured bioinformatics workflow that integrates these databases. The following diagram outlines a generalized experimental protocol for a comparative genomic study.
Detailed Experimental Protocol
The workflow above is implemented through the following detailed steps, which can be adapted for studying niche-specific adaptations:
Genome Dataset Curation: Collect high-quality genome sequences with clear metadata on isolation source (e.g., human, animal, environment). Apply stringent quality control: exclude contig-level assemblies, require high N50 (e.g., ≥50,000 bp), and ensure high completeness (≥95%) and low contamination (<5%) using tools like CheckM. Remove redundant genomes by calculating genomic distances with Mash and applying clustering (e.g., genomic distance ≤0.01) to obtain a non-redundant set [2].
Open Reading Frame (ORF) Prediction: Annotate all curated genomes using a standardized tool like Prokka to consistently identify protein-coding sequences [2].
Functional and Specialized Annotation:
- COG Annotation: Map predicted ORFs to the COG database using RPS-BLAST (e-value threshold: 0.01, minimum coverage: 70%) to assign functional categories [2].
- CAZy Annotation: Identify carbohydrate-active enzymes using dbCAN2 (or HMMER against CAZy HMM profiles with parameter
hmm_eval 1e-5) to assign ORFs to Glycoside Hydrolase (GH), GlycosylTransferase (GT), and other CAZy families [2]. - VFDB & CARD Annotation: Screen ORFs against VFDB and CARD using appropriate tools (e.g., BLAST, RPS-BLAST) with defined identity/coverage thresholds to identify virulence and antibiotic resistance genes.
Data Integration and Statistical Analysis: Merge the annotation results into a unified table. Conduct comparative analyses (e.g., ANOVA, Chi-square tests) to identify genes and functions significantly enriched in specific niches (human, animal, environment). Use machine learning algorithms (e.g., random forest) with functional profiles as features to build predictive models of niche adaptation and identify key genetic determinants [2].
Phylogenetic Contextualization: For evolutionary insight, construct a robust phylogenetic tree. Extract universal single-copy genes (e.g., using AMPHORA2), align them (e.g., with Muscle), concatenate the alignments, and infer a maximum-likelihood tree (e.g., with FastTree). This tree controls for phylogenetic relatedness when comparing genetic traits across niches [2].
Table 3: Key Bioinformatics Tools and Resources for Database Analysis
| Resource Name | Type | Primary Function in Analysis |
|---|---|---|
| Prokka | Software Tool | Rapid prokaryotic genome annotation; generates the standardized ORF calls required for downstream database searches [2]. |
| BLAST/RPS-BLAST | Algorithm/Suite | Fundamental tool for sequence similarity searching; used for mapping ORFs to COG, VFDB, and CARD [24] [2]. |
| HMMER | Software Tool | Profile Hidden Markov Model searches; provides a more sensitive method for detecting remote homologs, essential for CAZy and other family-based annotations [2] [27]. |
| dbCAN2 | Web Server/Pipeline | Automated pipeline for CAZyme annotation; integrates multiple tools including HMMER for robust assignment of sequences to CAZy families [2]. |
| CheckM | Software Tool | Assesses genome quality (completeness and contamination) which is a critical prerequisite for meaningful comparative genomics [2]. |
| Mash | Software Tool | Estimates genomic distance and performs fast genome clustering to reduce dataset redundancy and avoid phylogenetic bias [2]. |
Research Insights: Linking Database Queries to Biological Understanding
Key Findings from Integrated Database Studies
The application of these integrated databases has yielded critical insights into microbial adaptation. A large-scale comparative genomics study of 4,366 pathogen genomes, which employed COG, VFDB, and CAZy, revealed distinct niche-specific strategies [2]. Human-associated bacteria, particularly Pseudomonadota, were enriched in VFDB-derived virulence factors for immune modulation and adhesion, and CAZy-derived genes for carbohydrate-active enzymes, indicating co-evolution with the human host. In contrast, environmental bacteria showed COG enrichment in general metabolic and transcriptional regulation functions. Furthermore, the study identified specific adaptive genes like hypB in human-associated strains using this database-integrated approach [2].
VFDB's curation of anti-virulence compounds reveals the translational potential of this research. The database has cataloged 902 such compounds, with a significant focus on targeting virulence factors like biofilms, effector delivery systems, and exoenzymes [11]. This information is crucial for developing drugs that disarm pathogens without imposing the strong selective pressure that drives antibiotic resistance [19] [11].
Conceptual Framework of Anti-Virulence Targeting
The following diagram illustrates key virulence mechanisms and their corresponding inhibitors, as cataloged in VFDB, highlighting potential therapeutic strategies.
The integrated use of VFDB, CARD, COG, and CAZy databases provides a powerful, multi-dimensional framework for deciphering the genetic basis of bacterial pathogenicity and niche adaptation. While each database excels in its specialized domain—VFDB in virulence, CARD in resistance, COG in core function, and CAZy in carbohydrate metabolism—their collective strength lies in the holistic functional portrait they create when used together. Standardized experimental protocols, as outlined, enable researchers to systematically identify niche-specific genetic signatures, from virulence factors and resistance genes to metabolic adaptations. As these databases continue to grow and incorporate new features like VFDB's anti-virulence compound repository [11] and COG's expanded pathway groupings [23], their value for comparative genomics and drug discovery will only increase. This database-driven approach is fundamental for advancing our understanding of host-pathogen interactions and developing novel strategies to combat infectious diseases.
Machine Learning and GWAS for Identifying Niche-Associated Signature Genes
Understanding the genetic determinants that enable bacterial pathogens to adapt to specific hosts and environments is a cornerstone of modern infectious disease research. The interplay between microbial genomes and their ecological niches not only influences host health but also drives bacterial genome diversification, enhancing pathogen survival across varied environments [3]. Within this context, the identification of niche-associated signature genes—genetic elements linked to survival in specific habitats like humans, animals, or environmental settings—has become a critical research focus. The convergence of genome-wide association studies (GWAS) and machine learning (ML) has revolutionized this field, enabling researchers to move beyond correlation to establish causal relationships between genetic variants and niche-specific adaptations. This guide provides a comparative analysis of experimental methodologies, benchmarking data, and reagent solutions for identifying these signature genes, with particular emphasis on applications within virulence factors research across ecological niches.
Experimental Approaches: A Comparative Framework
Core Methodologies and Their Applications
Table 1: Comparative Analysis of Genomic Approaches for Identifying Niche-Associated Genes
| Method | Core Principle | Best Use Cases | Strengths | Limitations |
|---|---|---|---|---|
| Traditional GWAS (e.g., Pyseer) | Identifies statistical associations between genetic variants and phenotypes across genomes [28]. | Antimicrobial resistance traits under low selection pressure; diverse datasets with high recombination rates [29]. | High interpretability; established statistical frameworks; effective for variants with minimal phylogenetic influence. | Struggles with variants concordant with phylogeny; requires careful population structure correction [29]. |
| pan-GWAS | Extends GWAS to include accessory genome (genes not shared by all strains) [30]. | Assessing zoonotic potential in closely related pathogens; host specificity studies. | Captures broader genetic diversity; identifies gene presence/absence associations. | Complex interpretation with thousands of genes; requires high-quality pangenome annotation. |
| Machine Learning Integration (e.g., aurora) | Uses ML algorithms to identify patterns in genomic data while accounting for population structure [29]. | Habitat adaptation traits; datasets with metadata errors or allochthonous strains; lineage-associated variants [29]. | Robust to mislabeled samples; identifies both lineage and locus effects simultaneously; handles phylogenetic correlations. | "Black box" interpretation challenges; computationally intensive; requires careful parameter tuning. |
| Comparative Genomics | Compiles genomic features across isolates from different niches using functional databases [3]. | Broad characterization of niche-specific enrichment in virulence factors, carbohydrate-active enzymes, and antibiotic resistance genes. | Holistic view of genomic adaptations; integrates multiple functional annotation systems. | Primarily identifies correlations; limited causal inference without experimental validation. |
Experimental Workflows and Protocols
Large-Scale Comparative Genomic Analysis
Table 2: Key Experimental Steps for Large-Scale Genomic Comparisons
| Step | Protocol Details | Tools/Databases | Critical Parameters |
|---|---|---|---|
| Genome Collection & Quality Control | Obtain metadata and genomes from repositories; filter based on assembly quality and source information [3]. | gcPathogen database; CheckM; Mash | Completeness ≥95%; contamination <5%; N50 ≥50,000 bp; genomic distance ≤0.01 for redundancy removal [3]. |
| Niche Annotation | Categorize isolates based on isolation source and host information [3]. | Custom metadata curation | Human (clinical samples); Animal (livestock, wildlife); Environment (water, soil, surfaces). |
| Functional Annotation | Predict open reading frames; map to functional databases [3]. | Prokka; COG database; dbCAN2; VFDB; CARD | e-value threshold 0.01; minimum coverage 70%; hmm_eval 1e-5 for CAZy annotation [3]. |
| Statistical Analysis & ML | Identify niche-enriched genes; build predictive models [3]. | Scoary; SVM; Random Forest | Correction for multiple testing; phylogenetic confounding adjustment; cross-validation. |
Figure 1: Workflow for identifying niche-associated signature genes using GWAS and machine learning, showing the progression from data preparation through analysis to validation.
Integrated GWAS-ML Workflow for Habitat Adaptation
The aurora algorithm represents a significant methodological advancement by specifically addressing key limitations in microbial GWAS [29]. Its unique two-phase approach includes:
Phenotype Validation (aurora_pheno()): This initial phase identifies mislabeled or allochthonous strains through iterative machine learning model training (Random Forest, AdaBoost, logistic regression, and CART) with intentional random mislabeling to establish classification probability thresholds [29].
Association Testing (aurora_GWAS()): After removing mislabeled strains, this function calculates genotype-phenotype association scores using bootstrapped datasets adjusted for strain non-independence, effectively handling both lineage and locus effects without priori assumptions [29].
Performance Benchmarking: Quantitative Comparisons
Method Performance Across Simulation Scenarios
Table 3: Benchmarking Results of GWAS Methods Across Simulated Datasets
| Method | Causal Variant Detection Power | False Positive Control | Performance with Mislabeled Strains | Lineage Effect Detection |
|---|---|---|---|---|
| aurora | 92% (MuSSE1 simulation); 88% (MuSSE2 simulation) [29] | Excellent (controlled FPR <5%) [29] | Robust (maintains >85% power with 15% mislabeling) [29] | Excellent (specifically designed for lineage effects) [29] |
| Pyseer | 45% (MuSSE1); 52% (MuSSE2) [29] | Moderate (FPR ~10-15%) [29] | Poor (power drops to <30% with 15% mislabeling) [29] | Limited (removes lineage-associated variants) [29] |
| Scoary | 65% (single causal gene scenario) [29] | Good (FPR ~5-8%) [29] | Moderate (power drops to ~45% with mislabeling) [29] | Limited (phylogenetic correction removes lineage signals) [29] |
| Hogwash | 38% (MuSSE1); 41% (MuSSE2) [29] | Excellent (FPR <5%) [29] | Poor (requires accurate strain labeling) [29] | Moderate (identifies convergent evolution) [29] |
Case Study Performance Metrics
Brucella Zoonotic Potential Assessment
In a study evaluating the zoonotic potential of Brucella species, researchers integrated pan-GWAS with machine learning, identifying 268 genes associated with zoonotic potential [30]. When these genes were used as features in ML models:
- Support Vector Machine (SVM) achieved the highest accuracy (94.2%) in predicting zoonotic potential [30]
- Random Forest performed slightly lower (91.5% accuracy) but offered better feature interpretability [30]
- The model revealed host-origin influences, showing Brucella melitensis strains from humans had higher zoonotic potential than those from cattle, goats, and sheep [30]
Large-Scale Genomic Analysis Across Ecological Niches
A comprehensive analysis of 4,366 bacterial genomes across human, animal, and environmental niches revealed distinct genomic adaptation patterns [3]:
- Human-associated bacteria (particularly Pseudomonadota) showed enrichment in carbohydrate-active enzyme genes and virulence factors related to immune modulation and adhesion [3]
- Environmental bacteria (Bacillota and Actinomycetota) exhibited greater enrichment in metabolism and transcriptional regulation genes [3]
- Clinical settings isolates had higher prevalence of antibiotic resistance genes, particularly fluoroquinolone resistance [3]
- Machine learning algorithms identified hypB as a key host-specific bacterial gene potentially regulating metabolism and immune adaptation in human-associated bacteria [3]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Niche-Associated Gene Studies
| Reagent/Resource | Function | Application Examples | Implementation Considerations |
|---|---|---|---|
| gcPathogen Database | Repository for pathogen genomic data and metadata [3]. | Source of 1,166,418 human pathogen genomes for comparative analysis [3]. | Requires stringent quality control; filtering for completeness ≥95%, contamination <5% recommended [3]. |
| COG Database | Cluster of Orthologous Groups for functional categorization of genes [3]. | Annotation of core, accessory, and unique genes in pangenome studies [30]. | Use RPS-BLAST with e-value threshold 0.01, minimum coverage 70% [3]. |
| VFDB | Virulence Factor Database for identifying pathogenicity determinants [3]. | Annotation of virulence factors across niches; identification of niche-specific virulence enrichment [3]. | ABRicate tool with default parameters effectively maps genomes to VFDB [3]. |
| dbCAN2 | Database for carbohydrate-active enzyme annotation [3]. | Identifying CAZy gene enrichment in human-associated bacteria [3]. | HMMER tool with hmm_eval 1e-5 provides reliable annotations [3]. |
| CARD | Comprehensive Antibiotic Resistance Database [3]. | Profiling antibiotic resistance genes across clinical, animal, and environmental niches [3]. | Critical for One Health studies connecting resistance across reservoirs [31]. |
| Aurora R Package | Machine learning GWAS tool for microbial habitat adaptation [29]. | Identifying causal variants despite mislabeled strains or phylogenetic correlations [29]. | Implements both phenotype validation (aurorapheno) and association testing (auroraGWAS) [29]. |
Figure 2: Ecosystem of research reagents and their relationships in identifying niche-associated signature genes, showing the flow from data sources through annotation and analysis to discovery.
The integration of GWAS with machine learning represents a paradigm shift in identifying niche-associated signature genes, moving beyond correlation to establish causal relationships while accounting for complex microbial population structures. For virulence factor research across ecological niches, method selection should be guided by specific research questions: traditional GWAS suits traits with minimal phylogenetic influence, pan-GWAS excels in accessory genome analysis, while ML-integrated approaches like aurora offer robust solutions for complex habitat adaptation traits with lineage effects and metadata quality issues. The benchmarking data presented enables researchers to make evidence-based decisions, optimizing their experimental designs for identifying the genetic basis of pathogen niche specialization.
The genomic era has revolutionized our understanding of bacterial pathogenesis, revealing that virulence is not an intrinsic property but an ecological adaptation. Contemporary research demonstrates that bacterial pathogens employ niche-specific genomic strategies to colonize diverse hosts and environments [3]. Understanding these adaptive mechanisms requires a sophisticated integration of comparative genomics and functional analysis, moving beyond mere genetic identification to uncover profound mechanistic insights into host-pathogen interactions.
The "One Health" approach underscores the complex interdependencies within ecosystems, integrating human, animal, and environmental health [3]. Genomic diversity plays crucial roles in pathogen adaptability, with DNA mutation, repair, and horizontal gene transfer serving as key evolutionary mechanisms [3]. Bacteria adapt to host environments primarily through gene acquisition and loss, with horizontal gene transfer being particularly common among host-associated microbiota [3]. Staphylococcus aureus, for instance, has acquired a variety of host-specific genes through this process, including immune evasion factors in equine hosts and methicillin resistance determinants in human-associated strains [3].
This guide provides a comprehensive comparison of methodological frameworks for identifying and functionally characterizing virulence factors across ecological niches, equipping researchers with the tools to bridge genetic identification with mechanistic understanding in pathogen research.
Methodological Comparison: Databases and Analytical Frameworks
Comparative Genomic Workflows for Virulence Discovery
Large-Scale Genomic Analysis: Advanced comparative genomics enables the identification of niche-specific adaptive mechanisms across thousands of bacterial genomes. A 2025 study analyzing 4,366 high-quality bacterial genomes isolated from various hosts and environments revealed significant variability in bacterial adaptive strategies [3]. Human-associated bacteria, particularly from the phylum Pseudomonadota, exhibited higher detection rates of carbohydrate-active enzyme genes and virulence factors related to immune modulation and adhesion, indicating co-evolution with human hosts [3]. In contrast, environmental bacteria showed greater enrichment in genes related to metabolism and transcriptional regulation, while clinical isolates had higher detection rates of antibiotic resistance genes [3].
Specialized Pathogen Analysis: Targeted genomic studies provide detailed virulence characterization of emerging pathogens. Research on novel Aliarcobacter faecis and Aliarcobacter lanthieri species identified virulence-related factors through comprehensive genome analysis [32]. This approach revealed that both species possess flagella genes as motility and export apparatus, along with genes encoding Twin-arginine translocation and type II/III secretory pathways [32]. Invasion and immune evasion genes (ciaB, iamA, mviN, pldA, irgA, and fur2) were found in both species, while adherence genes (cadF and cj1349) were specific to A. lanthieri [32].
Table 1: Comparative Genomic Approaches for Virulence Factor Discovery
| Approach | Scope | Key Databases Used | Identified Virulence Elements | Niche-Specific Insights |
|---|---|---|---|---|
| Large-Scale Cross-Niche Analysis [3] | 4,366 bacterial genomes from human, animal, environmental sources | COG, dbCAN (CAZy), VFDB, CARD | Carbohydrate-active enzymes, immune modulation factors, adhesion proteins, antibiotic resistance genes | Human-associated: immune modulation genes; Environmental: metabolic genes; Clinical: fluoroquinolone resistance |
| Emerging Pathogen Characterization [32] | Reference strains of novel Aliarcobacter species | VFDB, custom virulence gene databases | Flagellar genes, secretory pathways (tatABC, pulEF, fliFN), invasion genes (ciaB, pldA), adherence factors | Species-specific adherence gene distribution; Stress resistance mechanisms adaptation |
| Gut Microbiome Virulence Profiling [21] | 5,452 commensal isolates from healthy individuals; 9 chronic diseases | Expanded VFDB 2.0 (62,332 nonredundant VFGs) | Adhesins, iron uptake systems, toxins (colibactin, FadA, B. fragilis toxin) | Disease-specific VFG features; E. coli and K. pneumoniae pathobiont roles in T2D |
Computational Frameworks for Virulence Prediction
Integrated Bioinformatics Pipelines: The MetaVF toolkit represents a significant advancement in virulence gene profiling, utilizing an expanded VFDB 2.0 database consisting of 62,332 nonredundant orthologues and alleles of virulence factor genes (VFGs) [21]. This toolkit employs a three-stage process: alignment of metagenomic sequences against the expanded database, filtering with tested sequence identity thresholds (90% TSI achieving TDR >97% and FDR <0.000767%), and annotation of VFG clusters, mobility, bacterial host taxonomy, and virulence categories [21]. Benchmarking demonstrates that MetaVF outperforms existing tools (PathoFact, ShortBRED, VFDB direct mapping) in both sensitivity and precision across various mutation rates [21].
Fungal Pathogen Applications: Computational approaches for fungal virulence factor discovery employ a systematic four-stage workflow [33]. This begins with data acquisition from public repositories (UniProt, FungiDB, MycoCosm), followed by careful tool selection based on biological objectives and prediction quality [33]. Subsequent filtering based on confidence metrics reduces false positives, with final outputs guiding experimental validation [33]. For respiratory dimorphic fungi like Coccidioides, these approaches can predict adhesins, transporters, secreted effectors, carbohydrate-active enzymes (CAZymes), and secondary metabolites, clarifying pathogenic mechanisms and guiding experimental design [33].
Table 2: Computational Tools for Virulence Factor Identification and Analysis
| Tool/Database | Primary Function | Data Input | Key Features | Performance Metrics |
|---|---|---|---|---|
| MetaVF Toolkit [21] | VFG profiling from metagenomes | Metagenomic reads, MAGs, HiFi reads | VFDB 2.0 database (62,332 VFGs), mobile VFG identification, bacterial host attribution | TDR >97%, FDR <0.000767% at 90% TSI; superior to PathoFact, ShortBRED |
| VFDB 2.0 [21] | Expanded virulence factor reference | Genome sequences, gene sequences | 62,332 nonredundant VFGs from 135 species; orthologues/alleles; mobility annotation | Species-specific (70%) and genus-specific (94%) VFG identification |
| Fungal Virulence Prediction Pipeline [33] | Multi-stage virulence factor discovery | Fungal proteomes, genomic sequences | Adhesin, transporter, effector, CAZyme prediction; therapeutic target prioritization | Framework for target classification (high/moderate/low priority) |
Experimental Protocols: From In Silico to In Vitro Validation
Genomic DNA Extraction and Sequencing Protocols
Bacterial Culture and DNA Extraction: For virulence factor characterization in emerging pathogens, proven methodologies include culturing on specialized media under appropriate conditions. For Aliarcobacter species, successful protocols involve using modified Agarose Medium (m-AAM) with selective antibiotic supplements (cefoperazone, amphotericin-B, and teicoplanin), incubated at 30°C under microaerophilic conditions (85% N₂, 10% CO₂, and 5% O₂) for 3-6 days [32]. Genomic DNA can then be extracted and purified using commercial kits (e.g., Wizard Genomic DNA purification kit, Promega), with concentration determination via fluorometry (Qubit 2.0 Fluorometer) [32].
Library Preparation and Sequencing: For comprehensive genome analysis, Illumina TruSeq DNA library preparation kits effectively generate libraries with median insert sizes of 300 bp [32]. After PCR enrichment, libraries are quantified and sequenced on Illumina platforms (e.g., HiSeq 2500) generating 2×101 bp paired-end reads [32]. Mate-pair sequencing using Nextera Mate Pair kits with size selection (1.8-3.5 Kb, 4.0-7.0 Kb, and 8.0-12.0 Kb fragments) provides additional scaffolding information [32].
Virulence Gene Validation Protocols
PCR Verification of Virulence Factors: Following genomic identification, specific virulence factors require experimental validation. For Aliarcobacter species, researchers have successfully validated 11 virulence-associated genes using PCR assays, including six virulence genes (cadF, ciaB, irgA, mviN, pldA, and tlyA), two antibiotic resistance genes [tet(O) and tet(W)], and three cytolethal distending toxin genes (cdtA, cdtB, and cdtC) [32]. This approach confirmed that A. lanthieri tested positive for all 11 virulence-associated genes, while A. faecis showed positive for ten genes (with cdtB unavailable for testing) [32].
Functional Assessment of Virulence Mechanisms: Beyond genetic presence, functional assays are crucial for mechanistic insights. For Coccidioides adhesins like spherule outer wall glycoprotein (SOWgp), functional validation includes binding assays to host extracellular matrix components (laminin, fibronectin, collagen) and murine infection models demonstrating decreased virulence in SOWgp-depleted strains [33]. These functional assays confirm the essential role of specific virulence factors in pathogenesis and provide mechanistic insights into host-pathogen interactions.
Integrated Workflow: From Genetic Identification to Mechanistic Insight
The following workflow illustrates the comprehensive pipeline for virulence factor discovery and validation, integrating computational and experimental approaches:
Integrated Workflow for Virulence Factor Discovery
This integrated workflow demonstrates the systematic progression from genomic data acquisition to mechanistic understanding, highlighting critical decision points for target prioritization and validation.
The Scientist's Toolkit: Essential Research Reagents and Databases
Table 3: Essential Research Reagents and Databases for Virulence Factor Analysis
| Category | Specific Tool/Reagent | Function/Application | Key Features/Benefits |
|---|---|---|---|
| Bioinformatics Databases | VFDB 2.0 [21] | Virulence factor gene annotation | 62,332 nonredundant VFGs from 135 species; mobile element annotation |
| dbCAN2 [3] | Carbohydrate-active enzyme annotation | HMMER-based mapping to CAZy database; hmm_eval 1e-5 threshold | |
| CARD [3] | Antibiotic resistance gene identification | Comprehensive resistance gene database; functional annotation | |
| Experimental Reagents | Modified Agarose Medium (m-AAM) [32] | Aliarcobacter culture | Selective antibiotics (cefoperazone, amphotericin-B, teicoplanin) |
| Wizard Genomic DNA Purification Kit [32] | High-quality DNA extraction | Sufficient yield for Illumina/PacBio sequencing | |
| Analytical Tools | MetaVF Toolkit [21] | VFG profiling from metagenomes | Species-level VFG attribution; TPM normalization; mobility prediction |
| AMPHORA2 [3] | Phylogenetic tree construction | 31 universal single-copy genes; maximum likelihood trees | |
| Specialized Assays | Virulence Factor PCR Arrays [32] | Target gene validation | 11 VAT gene verification; species-specific confirmation |
The functional analysis of virulence factors has evolved from simple genetic identification to sophisticated mechanistic insights that account for ecological context and niche-specific adaptations. The integration of large-scale comparative genomics with specialized computational tools and rigorous experimental validation creates a powerful framework for understanding bacterial pathogenesis.
Current research reveals that virulence is not a binary property but a spectrum of adaptations to specific ecological niches. Human-associated bacteria exhibit distinct genomic profiles compared to environmental isolates, with enrichment in immune modulation and adhesion factors reflecting co-evolution with human hosts [3]. The identification of niche-specific signature genes, such as hypB in human-associated bacteria, provides crucial targets for therapeutic intervention and transmission control [3].
As computational methods continue to advance, with tools like MetaVF offering unprecedented sensitivity and precision in virulence gene identification [21], and experimental approaches provide functional validation, the field moves closer to comprehensive understanding of host-pathogen interactions. This progress enables more targeted antimicrobial strategies, informed antibiotic stewardship, and novel therapeutic development based on the fundamental mechanisms of bacterial virulence across diverse ecological contexts.
Challenges and Solutions in Virulence Factor Research and Application
The development of probiotics and live biotherapeutic products (LBPs) presents a unique regulatory challenge: balancing their potential health benefits with a rigorous safety assessment, primarily focused on virulence factors. Virulence factors are bacterial traits that enable invasion, colonization, damage to the host, and immune evasion. For pathogenic strains, these factors are well-documented drivers of disease. However, the distinction between a pathogen and a therapeutic can sometimes hinge on the precise combination and genomic context of these very genes. Strains used as therapeutics must be devoid of functional virulence factors that could confer pathogenic potential, making their identification and characterization a critical regulatory hurdle [34] [35].
This guide compares the landscape of virulence factor assessment, providing researchers and drug development professionals with a framework for navigating the complex regulatory requirements. By integrating comparative genomics, functional assays, and evolutionary safety considerations, we outline a pathway for translating promising bacterial strains into approved therapeutics.
Comparative Genomics of Virulence Across Ecological Niches
Genomic Insights into Niche Adaptation
Comparative genomic analyses reveal that bacterial pathogens employ distinct genetic strategies to adapt to different hosts and environments. Understanding these niche-specific adaptations is crucial for evaluating the potential risks associated with bacterial strains intended for therapeutic use.
Table 1: Niche-Specific Genomic Features in Bacterial Pathogens
| Ecological Niche | Phylum Examples | Enriched Virulence Factors | Adaptive Mechanisms | Key Genomic Features |
|---|---|---|---|---|
| Human-Associated | Pseudomonadota | Immune modulation, adhesion factors [2] | Gene acquisition, co-evolution with host [2] | Higher detection rates of carbohydrate-active enzyme genes [2] |
| Clinical Settings | Various | Antibiotic resistance genes (e.g., fluoroquinolone) [2] | Horizontal gene transfer, selection pressure [2] | Enrichment of resistance determinants on mobile genetic elements [2] |
| Animal Hosts | Various | Diverse virulence & resistance genes [2] | Host switching, reservoir formation [2] | Significant reservoirs of antibiotic resistance genes [2] |
| Environmental | Bacillota, Actinomycetota | Metabolic versatility, transcriptional regulation [2] | Genome reduction, resource reallocation [2] | Enrichment in genes for metabolism and transcriptional regulation [2] |
The Pathogen-Probiotic Spectrum: A Case Study ofEnterococcus faecium
The species Enterococcus faecium exemplifies the fine line between pathogen and probiotic, a distinction determined by the presence or absence of specific virulence and resistance genes [34].
- Probiotic Strains: Strains like E. faecium T110 and 17OM39 are marketed as probiotics. Genomic analyses confirm the absence of known functional virulence genes (such as cylA, esp, agg, and gelE) and vancomycin resistance genes. Their genomes are notably stable, lacking frequently found transposable elements, and they harbor genes beneficial for persistence in the gastrointestinal tract [34] [36].
- Pathogenic Strains: In contrast, pathogenic strains like E. faecium Aus0004 and DO are isolated from human blood and possess acquired virulence factors, including those for immune evasion and cytolysin production, along with antibiotic resistance genes like vancomycin and tetracycline resistance determinants [34].
- Non-Pathogenic Non-Probiotic (NPNP) Strains: Strains such as E. faecium NRRL B-2354 occupy a middle ground, used as surrogates in food safety testing without causing disease. Their genomes lack the virulent markers of pathogenic strains but may not possess the full suite of beneficial traits found in dedicated probiotics [34].
Methodologies for Virulence Assessment in Probiotic Development
A robust assessment of virulence potential requires a multi-faceted approach, combining in silico genomics with in vitro functional assays.
1In SilicoGenomic Analysis
The first and most critical step is a comprehensive genomic screening.
- Whole Genome Sequencing (WGS): WGS provides the complete genetic blueprint of a candidate strain. Platforms like PacBio Sequel II facilitate high-quality, contiguous assemblies, which are essential for accurate gene annotation [37].
- Virulence Factor Databases: Tools like VirulenceFinder (from the Center for Genomic Epidemiology) and the Virulence Factor Database (VFDB) are used to systematically screen the genome against curated databases of known virulence genes [32] [37].
- Antimicrobial Resistance Gene (ARG) Detection: The Comprehensive Antibiotic Resistance Database (CARD) and tools like ResFinder are employed to identify acquired antibiotic resistance genes. The absence of transferable ARGs is a key safety requirement [38] [37].
- Mobile Genetic Element (MGE) Analysis: Tools like MobileElementFinder are used to identify plasmids, prophages, and insertion sequences. Since virulence and resistance genes are often located on MGEs, their absence is a strong indicator of genomic stability and safety [37].
2In VitroFunctional Assays
Genomic predictions must be validated with phenotypic tests.
- Adhesion and Invasion Assays: The adhesive potential of a strain to intestinal epithelial cells (e.g., Caco-2, HT-29) is measured. A high adhesion capacity is desirable for probiotic persistence but must be distinguished from pathogenic invasion. For example, E. faecium CM33 showed strong adhesion to Caco-2 cells while also reducing the adhesion of pathogens like E. coli and Listeria monocytogenes by more than 50% [36].
- Cytotoxicity Screening: Cell lines are exposed to bacterial supernatants or cells to check for cytotoxic effects. The absence of hemolytic activity on blood agar and gelatinase activity are standard, basic safety screens [37].
- Antibiotic Susceptibility Profiling: Phenotypic tests determine the strain's intrinsic resistance profile against a panel of clinically relevant antibiotics, ensuring it aligns with genomic predictions and established safety guidelines [36] [37].
Figure 1: A comprehensive workflow for assessing virulence factors in probiotic candidates, integrating in silico genomics with in vitro functional validation.
The Researcher's Toolkit: Essential Reagents and Databases
Table 2: Key Research Reagent Solutions for Virulence Assessment
| Category | Item/Reagent | Function in Assessment | Example/Reference |
|---|---|---|---|
| Bioinformatics Tools | VirulenceFinder, VFDB | Identifies known virulence factors from genomic data [32] [37] | E. faecium CM33 screened for cylA, esp, agg [36] |
| Bioinformatics Tools | CARD, ResFinder | Detects acquired antimicrobial resistance genes [38] [37] | B. breve JKL2022 confirmed free of acquired ARGs [37] |
| Bioinformatics Tools | MobileElementFinder | Identifies plasmids, prophages, and other mobile elements [37] | Used to confirm genomic stability of B. breve JKL2022 [37] |
| Cell Culture Models | Caco-2, HT-29 cells | In vitro model for assessing bacterial adhesion and invasion potential [36] [38] | E. faecium CM33 showed 241 ± 1 adhesion per 100 Caco-2 cells [38] |
| Culture Media | Simulated Gastric/Intestinal Fluid | Tests survival through gastrointestinal transit [38] | C. butyricum MCC0233 retained 87.9% viability after 6h [38] |
| Biochemical Assays | Hemolysis, Gelatinase tests | Basic phenotypic screens for toxin production [37] | B. breve JKL2022 tested negative for hemolysis [37] |
Regulatory Frameworks and the Challenge of Evolutionary Safety
A primary regulatory hurdle is the dynamic nature of bacterial genomes. Even a strain proven safe at the time of administration has the potential to evolve in vivo. Bacteria possess high mutation rates, large population sizes, and mechanisms for horizontal gene transfer (HGT), all of which can lead to the acquisition of undesirable traits post-administration [35].
- Hypermutator Phenotypes: Some probiotic strains, including Lactiplantibacillus plantarum and Bifidobacterium animalis, have been observed to develop hypermutator phenotypes within the mouse gut, accelerating adaptation but also increasing the risk of deleterious or dangerous mutations [35].
- Horizontal Gene Transfer: The risk of HGT is a major focus of regulatory scrutiny. Safety assessments must evaluate not only the intrinsic resistance of a strain but also its potential to acquire and transfer resistance genes from commensal gut microbiota [35].
- Mitigation Strategies: To address these evolutionary risks, developers can:
- Select for Genomic Stability: Prioritize strains with fewer mobile genetic elements and a history of stability, as seen with E. faecium 17OM39 [34].
- Utilize Directed Evolution: Harness evolutionary principles in a controlled laboratory setting (Adaptive Laboratory Evolution) to pre-adapt strains to the gut environment and stabilize beneficial traits, potentially reducing unpredictable evolution in vivo [35].
- Implement Post-Marketing Surveillance: Monitor circulating strains in the population to detect any long-term evolutionary shifts that could impact safety [35].
Figure 2: A logical decision matrix for regulatory assessment of probiotic candidates, highlighting key genomic and phenotypic safety gates.
Successfully navigating the regulatory hurdles for probiotics and LBPs requires a sophisticated, multi-layered strategy for virulence factor assessment. As demonstrated by comparative genomics, safety is not defined by a single gene but by the entire genetic context of a strain—the absence of virulence and transferable resistance genes, the stability of its genome, and its evolutionary trajectory. The path forward integrates advanced bioinformatics with classical microbiology, all viewed through the lens of evolutionary biology. By adopting this comprehensive framework, researchers can robustly demonstrate the safety of their therapeutic bacterial products, paving the way for their approval and successful application in improving human health.
Addressing Contamination and Persistence in Complex Environments
Bacterial pathogens exhibit a remarkable capacity to survive in complex environments, from natural ecosystems to clinical settings. This adaptability is driven by genomic plasticity, enabling both persistence under stress and the potential for environmental contamination with resistant strains [2]. A critical challenge in microbial ecology and infectious disease management lies in understanding the genetic mechanisms governing survival strategies across different ecological niches. This guide systematically compares the genomic features, virulence factors, and persistence mechanisms of bacterial pathogens from human, animal, and environmental sources, providing a framework for researchers investigating host-pathogen interactions and antimicrobial development.
The persistence of bacterial cells in stressful conditions, including antibiotic exposure, fundamentally differs from genetic resistance. While resistant cells genetically inherit their tolerance, persister cells represent a transient, non-growing or slow-growing phenotypic state within a susceptible population that survives antibiotic treatment without possessing resistance genes [39] [40]. These persisters can regrow after stress removal and are now recognized as primary contributors to chronic and relapsing infections, biofilm-associated diseases, and treatment failures [39]. Understanding the interplay between persistence mechanisms and niche-specific genomic adaptations is essential for developing novel therapeutic strategies.
Comparative Genomic Analysis Across Ecological Niches
Genomic Adaptation Strategies
Comparative genomic analyses of 4,366 high-quality bacterial genomes reveal distinct adaptive strategies employed by pathogens from different sources. Human-associated bacteria, particularly from the phylum Pseudomonadota, demonstrate extensive co-evolution with their host, characterized by higher frequencies of carbohydrate-active enzyme (CAZyme) genes and specific virulence factors related to immune modulation and adhesion [2]. This suggests an evolutionary trajectory fine-tuned for host colonization and nutrient acquisition.
In contrast, environmental bacteria (e.g., from phyla Bacillota and Actinomycetota) show greater enrichment in genes related to metabolic diversity and transcriptional regulation, reflecting the need for versatility in fluctuating environments [2]. Some lineages, such as Mycoplasma genitalium, have undergone extensive genome reduction as an adaptive strategy, reallocating resources toward maintaining mutualistic relationships [2]. Meanwhile, clinical isolates exhibit marked enrichment of antibiotic resistance genes, particularly those conferring fluoroquinolone resistance, while animal hosts serve as significant reservoirs for both virulence and resistance genes, highlighting their role in the One Health continuum [2].
Key Genomic Features by Niche
Table 1: Comparative Genomic Features Across Ecological Niches
| Ecological Niche | Key Adaptive Strategy | Enriched Functional Categories | Notable Virulence/Resistance Factors |
|---|---|---|---|
| Human-Associated | Gene acquisition & co-evolution | Carbohydrate-active enzymes (CAZymes), immune modulation factors | Adhesion proteins, immune evasion factors [2] |
| Clinical Settings | Resistance gene acquisition | Antibiotic resistance mechanisms | Fluoroquinolone resistance genes [2] |
| Animal-Associated | Reservoir maintenance | Diverse metabolic pathways | Virulence factors, antibiotic resistance genes [2] |
| Environmental | Metabolic versatility & genome reduction | Transcriptional regulation, diverse metabolism | Stress response systems, reduced virulence repertoire [2] |
Experimental Protocols for Comparative Analysis
Genome Sequencing and Quality Control
Protocol 1: Genome Dataset Construction High-quality, non-redundant genome collections are constructed through stringent quality control. Genome sequences should be filtered based on assembly quality (N50 ≥50,000 bp) and completeness (CheckM evaluation with ≥95% completeness and <5% contamination) [2]. Taxonomic annotation accuracy must be verified through phylogenetic placement. Genomic distances are calculated using Mash, with clustering via Markov clustering to remove redundant genomes (genomic distances ≤0.01) [2].
Protocol 2: Phylogenetic Analysis For phylogenetic tree construction, identify 31 universal single-copy genes from each genome using AMPHORA2 [2]. Generate multiple sequence alignments for each marker gene using Muscle v5.1, then concatenate alignments into a comprehensive dataset [2]. Construct maximum likelihood trees using FastTree v2.1.11, with visualization through iTOL. Convert phylogenetic trees to evolutionary distance matrices using the R package ape, then perform k-medoids clustering (e.g., using the pam function in the R cluster package) to define populations for comparative analysis [2].
Functional Annotation and Comparative Genomics
Protocol 3: Functional Categorization Predict open reading frames (ORFs) using Prokka v1.14.6 [2]. Map predicted ORFs to functional databases using RPS-BLAST (for COG database with e-value threshold of 0.01 and minimum coverage of 70%) and HMMER (for CAZy database via dbCAN2 with hmm_eval 1e-5) [2]. For virulence factor annotation, perform Diamond blast searches against the Virulence Factor Database (VFDB) with e-value cutoff of 1e-5 [2].
Protocol 4: Diversity and Enrichment Analysis Calculate alpha diversity indices (Observed species and Shannon indices) for CAZymes and virulence factors using the 'vegan' package in R [41]. Conduct differential abundance analysis of species and metabolic pathways using the 'ALDEx2' and 'DESeq2' packages in R [41]. Correct for batch effects in relative abundance tables (species, pathways, CAZymes, virulence factors) using the 'MMUPHin' R package [41].
Table 2: Key Bioinformatics Tools for Genomic Analysis
| Tool Name | Version/Reference | Primary Function | Key Parameters |
|---|---|---|---|
| Prokka | v1.14.6 [2] | Rapid annotation of prokaryotic genomes | Default parameters for ORF prediction |
| dbCAN2 | (Zhang et al., 2018) [2] | CAZyme annotation | HMMER with hmm_eval 1e-5 |
| Diamond | v2.0.15 [41] | BLAST searches against VFDB | e-value cutoff 1e-5 |
| CD-HIT | v4.8.1 [41] | Construction of non-redundant gene catalog | ≥95% similarity, 90% coverage |
| FastTree | v2.1.11 [2] | Maximum likelihood phylogenetic trees | Default parameters for concatenated alignments |
Visualization of Key Pathways and Workflows
Bacterial Persistence Formation Pathways
Diagram 1: Bacterial persistence formation pathways.
Comparative Genomics Workflow
Diagram 2: Comparative genomics workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Databases
| Reagent/Database | Category | Function | Application Example |
|---|---|---|---|
| CAZy Database | Functional Database | Annotates carbohydrate-active enzymes | Identifying niche-specific nutrient acquisition capabilities [2] [41] |
| Virulence Factor Database (VFDB) | Specialized Database | Catalogs bacterial virulence factors | Comparing pathogenic potential across isolates [2] [41] |
| CARD (Comprehensive Antibiotic Resistance Database) | Resistance Database | Annotates antibiotic resistance genes | Profiling resistome across ecological niches [2] |
| EggNOG Database | Functional Database | Provides functional annotation and KEGG pathway mapping | Metabolic pathway comparison across bacterial populations [41] |
| CheckM | Quality Control Tool | Assesses genome completeness and contamination | Quality control in genome dataset construction [2] |
| Salmon | Quantification Tool | Quantifies ORF abundance from metagenomic data | Gene expression and functional potential analysis [41] |
Discussion and Research Implications
The comparative analysis of virulence factors and persistence mechanisms across ecological niches reveals fundamental principles of bacterial adaptation. Human-associated pathogens demonstrate specialized adaptations for host interaction, while environmental isolates maintain broader metabolic capabilities. Critically, animal hosts serve as important reservoirs for resistance genes, and captive environments can reshape virulence factor profiles in gut microbiomes, increasing pathogenic potential [2] [41]. These findings highlight the interconnected nature of microbial ecosystems under the One Health framework.
From a therapeutic perspective, understanding persistence mechanisms provides crucial insights for addressing chronic infections. Unlike genetic resistance, persistence involves transient phenotypic switching to dormant states, making these populations refractory to conventional antibiotics that target active cellular processes [39]. Future therapeutic strategies should consider combination approaches that target both growing populations and persistent subpopulations, potentially through compounds that disrupt toxin-antitoxin systems, stringent response pathways, or metabolic quiescence [39]. The continued identification of niche-specific signature genes, such as hypB in human-associated bacteria, offers promising targets for novel antimicrobial development [2].
Overcoming Limitations in Cultivation and Functional Characterization
Understanding the genetic basis of bacterial pathogen adaptation is crucial for developing targeted treatments and prevention strategies [3]. However, a significant challenge persists: many pathogens are difficult or impossible to cultivate in laboratory settings, and directly linking genes to functions, especially virulence, remains complex [3] [42]. This is particularly true when comparing virulence factors across different ecological niches (human, animal, environmental) [3]. The inability to culture an organism precludes classic genetic manipulation and phenotypic screening, creating a major bottleneck in functional characterization. This guide objectively compares modern genomic solutions to these traditional limitations, providing researchers with a framework for advancing pathogen research without relying solely on cultivation.
Solution Comparison: Genomic Approaches vs. Traditional Cultivation
The table below summarizes the limitations of traditional methods and how contemporary genomic solutions overcome them.
| Traditional Challenge | Genomic Solution | Key Advantage | Supporting Experimental Data |
|---|---|---|---|
| Inability to Culture Organisms | Culture-independent whole-genome sequencing from direct samples [3]. | Enables genetic characterization of unculturable pathogens, expanding the known pathogen repertoire. | Identification of novel Aliarcobacter faecis and A. lanthieri from human and livestock feces without prior isolation [32]. |
| Linking Genotype to Phenotype | Comparative genomic analysis across ecological niches using bioinformatics databases (COG, VFDB, CARD) [3]. | Identifies niche-specific genetic signatures (e.g., virulence, antibiotic resistance genes) directly from sequence data. | Human-associated bacteria showed higher virulence factors for immune modulation; clinical isolates had more fluoroquinolone resistance genes [3]. |
| Functional Validation in Non-Model Organisms | Machine learning (e.g., Scoary) to predict host-specific genes, followed by targeted experimental validation [3]. | Prioritizes key genes from vast genomic datasets for downstream functional studies, saving time and resources. | The gene hypB was identified as a potential key regulator of metabolism and immune adaptation in human-associated bacteria [3]. |
| Characterizing Genes in Polyploid Crops | Use of high-quality reference sequences (e.g., RefSeq v1.0 for wheat) and sequenced mutant populations (TILLING) [42]. | Allows functional genetic studies directly in agronomically important but genetically complex species. | In wheat, over half of high-confidence genes exist as three homoeologous copies, which can now be studied individually [42]. |
Detailed Experimental Protocols for Genomic Workflows
Protocol 1: Genome-Wide Comparison of Virulence Factors
This methodology is adapted from a large-scale comparative genomics study of bacterial pathogens [3].
1. Genome Dataset Curation:
- Source: Obtain metadata and genome sequences from public databases like gcPathogen.
- Quality Control: Implement stringent filters. Retain only genomes with:
- N50 ≥ 50,000 bp.
- CheckM completeness ≥ 95%.
- CheckM contamination < 5%.
- Clear isolation source information (human, animal, environment).
- Redundancy Reduction: Calculate genomic distances using Mash and perform clustering (e.g., Markov clustering) to remove near-identical genomes (distance ≤ 0.01).
2. Phylogenetic Analysis:
- Marker Gene Extraction: Identify 31 universal single-copy genes from each genome using a tool like AMPHORA2.
- Alignment and Tree Building: Perform multiple sequence alignments for each gene (e.g., with Muscle). Concatenate alignments and construct a maximum likelihood phylogenetic tree using FastTree.
3. Functional and Virulence Annotation:
- Gene Prediction: Predict Open Reading Frames (ORFs) using Prokka.
- Functional Categorization: Map ORFs to the Cluster of Orthologous Groups (COG) database using RPS-BLAST (e-value threshold 0.01, minimum coverage 70%).
- Virulence Factor Identification: Use ABRicate to map genomes to the Virulence Factor Database (VFDB) for identifying virulence genes.
- Antibiotic Resistance Gene Screening: Similarly, use ABRicate with the CARD database to identify resistance genes.
4. Data Integration and Analysis:
- Enrichment Analysis: Statistically determine which COG categories, virulence factors, or resistance genes are over-represented in specific ecological niches (human, animal, environment).
- Machine Learning: Apply tools like Scoary to identify genes highly associated with a particular niche. Validate predictive models on held-out genome sets.
Protocol 2: Functional Characterization of a Target Gene
This protocol outlines a general roadmap for moving from a gene candidate to functional insight, integrating principles from crop and bacterial genomics [42] [32].
1. Target Gene Identification:
- Input: Use results from comparative genomics (e.g., a niche-specific gene like hypB [3]) or homology-based searches (e.g., finding wheat orthologs of known Arabidopsis genes via Ensembl Plants [42]).
2. In silico Characterisation:
- Gene Model Inspection: Use a genome browser (e.g., Ensembl Plants, VFDB) to examine gene structure, homoeologs (in polyploids), and existing variant data [42].
- Expression Analysis: Consult expression atlases (e.g., expVIP for wheat) to see if the gene is expressed in relevant tissues or conditions [42].
3. Functional Validation:
- Mutant Screening: Screen available sequenced mutant populations (e.g., TILLING mutants in wheat) for lesions in the target gene [42].
- Genetic Transformation: Where possible, use improved transformation protocols to generate knock-out mutants or overexpressing lines for the target gene [42].
- Phenotyping: Conduct targeted phenotypic assays relevant to the hypothesized function (e.g., adhesion/invasion assays for virulence factors, stress tolerance assays, etc.) [32].
- PCR Confirmation: As used in Aliarcobacter studies, design specific PCR assays to confirm the physical presence of the candidate gene in the studied organism [32].
Visualizing the Research Workflow
The following diagram illustrates the integrated computational and experimental pathway for characterizing virulence factors, from genome to function.
The Scientist's Toolkit: Research Reagent Solutions
The table below details key reagents, databases, and tools essential for conducting the experiments described in this guide.
| Reagent / Resource | Function / Application | Specific Example |
|---|---|---|
| gcPathogen Database | Provides a centralized repository of metadata and genome sequences for human pathogens for comparative analysis [3]. | Source for 1,166,418 pathogen metadata records and genomes [3]. |
| CheckM | A tool for assessing the quality (completeness and contamination) of microbial genomes derived from isolates, single cells, or metagenomes [3]. | Used to filter genomes for completeness ≥95% and contamination <5% [3]. |
| VFDB (Virulence Factor Database) | A comprehensive resource for curating virulence factors of bacterial pathogens, used to annotate virulence genes in genomic sequences [3] [32]. | Identified adherence (cadF), invasion (ciaB), and toxin (cdtA, cdtB, cdtC) genes in Aliarcobacter [32]. |
| CARD (Comprehensive Antibiotic Resistance Database) | A bioinformatics resource containing data on resistance genes, mechanisms, and associated antibiotics, used for in silico resistance screening [3]. | Detected higher rates of fluoroquinolone resistance genes in clinical isolates [3]. |
| Ensembl Plants | A genome browser that integrates wheat genome assemblies, annotations, variation data, and gene trees, facilitating ortholog identification and genomic exploration [42]. | Used to access RefSeq v1.0 hexaploid wheat assembly and homoeolog information [42]. |
| TILLING (Targeting Induced Local Lesions IN Genomes) Populations | A reverse genetics method that uses chemical mutagenesis to create and identify point mutations in genes of interest, enabling functional studies in non-model crops [42]. | A resource for identifying mutants in specific wheat genes to study their function [42]. |
| Modified Agarose Medium (m-AAM) | A selective culture medium used for the isolation and cultivation of fastidious bacteria like Aliarcobacter under microaerophilic conditions [32]. | Used to culture A. faecis and A. lanthieri from fecal sources prior to DNA extraction and sequencing [32]. |
Optimizing Hygiene and Stewardship to Counter Niche-Driven Resistance
The escalating challenge of antimicrobial resistance (AMR) necessitates a paradigm shift from reactive treatment to proactive, niche-informed prevention and control. The ecological niche of a pathogen—whether human clinical settings, animal hosts, or environmental reservoirs—exerts distinct selective pressures that shape its repertoire of virulence factors and antibiotic resistance genes [3]. Understanding these niche-specific adaptations is critical for developing targeted hygiene and antimicrobial stewardship programs. This guide compares the virulence and resistance profiles of pathogens across different ecological niches, providing a data-driven framework for optimizing interventions to disrupt the transmission of resistant strains and preserve the efficacy of existing antimicrobials.
Comparative Genomic Analysis of Niche-Specific Adaptations
Large-scale comparative genomic studies reveal that bacterial pathogens employ distinct genetic strategies to survive and thrive in different habitats.
Key Genomic Features Across Ecological Niches
Table 1: Comparative genomic features of bacterial pathogens from different ecological niches, based on analysis of 4,366 high-quality genomes [3].
| Ecological Niche | Enriched Virulence Factors | Enriched Resistance Genes | Predominant Adaptive Strategies | Example Pathogens |
|---|---|---|---|---|
| Human Clinical | Immune modulation, adhesion (e.g., FimH in UPEC) [43] | Fluoroquinolone, β-lactam (e.g., blaTEM) [3] [43] | Gene acquisition (e.g., horizontally acquired pathogenicity islands) [3] [44] | Uropathogenic E. coli (UPEC), Candida albicans [43] [45] |
| Animal Hosts | Diverse adhesins and toxins (e.g., CadF) [32] | Sulfonamide (sul1, sul2), tetracycline [3] | Acting as reservoirs for resistance and virulence genes [3] | Aliarcobacter lanthieri, Staphylococcus aureus from livestock [3] [32] |
| Environment | Metabolic versatility, transcriptional regulation | Heavy metal resistance, biodegradation enzymes | Genome reduction, stress resistance (osmotic, heat) [3] [32] | Pseudomonas aeruginosa, Aliarcobacter faecis [3] [32] |
Insights from Niche Comparisons
- Human-Associated Pathogens: Bacteria from the phylum Pseudomonadota isolated from human hosts show a higher prevalence of genes encoding carbohydrate-active enzymes and virulence factors related to immune evasion and host cell adhesion, indicating a co-evolutionary arms race with the human immune system [3].
- Animal Hosts as Reservoirs: Animal-derived pathogens are significant reservoirs of resistance genes. They often carry a diverse set of virulence factors, such as the full complement of cytolethal distending toxin (CDT) genes (cdtA, cdtB, cdtC) observed in Aliarcobacter lanthieri, highlighting their potential for zoonotic transmission [32].
- Environmental Adaptability: Environmental isolates, particularly from the phyla Bacillota and Actinomycetota, are enriched in genes related to metabolic versatility and transcriptional regulation, allowing them to survive in fluctuating conditions. Some employ genome reduction as an adaptive strategy to streamline their genomes for survival in nutrient-limited environments [3].
Experimental Methodologies for Profiling Virulence and Resistance
To generate the comparative data essential for guiding stewardship, standardized experimental protocols are required to characterize pathogenic potential.
Genomic and Bioinformatic Workflow
Diagram 1: A workflow for the comparative genomic analysis of virulence and resistance factors.
Detailed Protocol for Comparative Genomics [3]:
- Genome Collection and Quality Control: Obtain high-quality, non-redundant bacterial genomes from public repositories (e.g., gcPathogen). Apply stringent quality filters: assembly N50 ≥ 50,000 bp, CheckM completeness ≥ 95%, and contamination < 5%. Classify genomes into ecological niches (human, animal, environment) based on isolation source metadata.
- Phylogenetic Tree Construction: Identify 31 universal single-copy genes from each genome using AMPHORA2. Perform multiple sequence alignment for each gene with Muscle v5.1. Concatenate alignments and construct a maximum likelihood phylogenetic tree using FastTree v2.1.11.
- Functional and Pathogenic Annotation:
- Predict Open Reading Frames (ORFs) using Prokka v1.14.6.
- Map ORFs to functional databases using RPS-BLAST (COG for functional categories) and HMMER (dbCAN2 for carbohydrate-active enzymes).
- Identify virulence factors by mapping to the Virulence Factor Database (VFDB) using ABRicate.
- Identify antibiotic resistance genes by mapping to the Comprehensive Antibiotic Resistance Database (CARD).
- Data Analysis: Perform enrichment analysis to identify genes significantly associated with specific niches. Use machine learning algorithms (e.g., Scoary) to identify signature genes predictive of a given ecological niche.
Phenotypic Assay Workflow
Diagram 2: A workflow for the phenotypic characterization of biofilm formation and antifungal resistance.
Detailed Protocol for Fungal Virulence and Resistance Profiling [45]:
Biofilm Formation Assay:
- Adjust fungal suspension to 1 McFarland standard in RPMI-1640 medium.
- Add 100 µL to polystyrene microtiter plates and incubate at 35°C for 2 hours.
- Discard medium, wash wells with phosphate buffer (pH 7.2), and add fresh medium.
- Replace medium every 24 hours after washing.
- After biofilm formation, fix with methanol for 15 minutes, then stain with 0.5% crystal violet for 15 minutes.
- Wash, solubilize with 33% acetic acid, and measure the optical density (OD) at 600 nm.
Antifungal Susceptibility Testing:
- Use the broth microdilution method according to CLSI guidelines (M59, M60).
- Determine the Minimum Inhibitory Concentration (MIC) for antifungal drugs (e.g., fluconazole, voriconazole, amphotericin B).
- Include quality control strains (C. albicans ATCC 90028 and C. parapsilosis ATCC 22019).
Virulence Gene Expression:
- Extract total RNA using a commercial kit.
- Synthesize cDNA using a reverse transcription kit.
- Perform quantitative real-time PCR (qRT-PCR) to quantify expression of virulence genes (e.g., secreted aspartyl proteinases SAP, adhesins ALS1, ALS3, HWP1).
- Normalize data to a housekeeping gene and analyze using the comparative Ct method.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key research reagent solutions for studying virulence and antimicrobial resistance.
| Reagent / Solution | Primary Function | Example Application | Reference |
|---|---|---|---|
| CHROMagar Candida Plates | Selective isolation and preliminary identification of Candida species. | Differentiation of C. albicans (emerald green colonies) from other species. | [45] |
| ATB Fungus 3 / Broth Microdilution Panels | Standardized antifungal susceptibility testing. | Determination of Minimum Inhibitory Concentrations (MICs) for common antifungals. | [45] |
| Crystal Violet Stain | Quantitative assessment of biofilm biomass. | Staining of mature biofilms formed on abiotic surfaces (e.g., microtiter plates). | [45] [43] |
| VITEK 2 Compact System | Automated microbial identification and antibiotic susceptibility testing. | Rapid identification of bacterial species and their resistance profiles in clinical settings. | [45] |
| dbCAN2 & VFDB Databases | In silico prediction of carbohydrate-active enzymes and virulence factors. | Functional annotation of bacterial genomes to predict ecological adaptations. | [3] |
| Tenebrio molitor Larvae | In vivo model for assessing pathogen virulence. | Evaluation of dose-dependent lethality of bacterial pathogens like UPEC. | [43] |
Implications for Hygiene and Antimicrobial Stewardship
The niche-specific profiles of virulence and resistance directly inform targeted interventions.
- Clinical Settings: The high prevalence of fluoroquinolone and β-lactam resistance in clinical isolates underscores the need for robust stewardship around these drug classes [3] [43]. The link between biofilm formation and antifungal treatment failure in C. albicans suggests that infection control protocols should prioritize disrupting biofilm formation on medical devices [45].
- Animal Agriculture: The role of animals as reservoirs for sulphonamide and tetracycline resistance genes calls for enhanced hygiene and stewardship in livestock farming. Reducing the non-therapeutic use of antibiotics in animal feed is critical to minimize the selection pressure for resistant strains that can transfer to humans [3] [46].
- One Health Surveillance: A holistic "One Health" approach that integrates surveillance across human, animal, and environmental niches is essential. Monitoring the emergence of pathogens like Aliarcobacter species, which carry an arsenal of virulence and toxin genes, in livestock manure can provide early warnings for potential public health threats [3] [32].
The battle against antimicrobial resistance must be fought on multiple fronts, guided by a deep understanding of pathogen ecology. Comparative genomic and phenotypic analyses, as detailed in this guide, provide the evidence base to tailor hygiene practices and stewardship programs to the specific threats present in each ecological niche. By moving beyond a one-size-fits-all approach and implementing niche-informed strategies, researchers, clinicians, and public health professionals can more effectively counter the evolution and spread of resistant pathogens.
Cross-Niche Validation: Comparative Virulence and Resistance Profiles
The evolutionary arms race between pathogens and their hosts drives the continuous refinement of microbial virulence mechanisms. For human-associated bacterial pathogens, successful colonization and persistence necessitate specific adaptations to overcome human host defenses. Recent comparative genomic analyses reveal that pathogens isolated from human hosts are significantly enriched in virulence factors related to two key functional categories: adhesion to host tissues and evasion of the immune system [2]. This enrichment pattern distinguishes human-associated pathogens from those isolated from animal hosts or environmental sources, highlighting specialized adaptation strategies to the human ecological niche.
The selective pressure of the human host environment shapes pathogen genomes through distinct evolutionary strategies. Human-associated Pseudomonadota (Proteobacteria) frequently acquire new genes through horizontal gene transfer that enhance host interaction capabilities [2]. In contrast, Actinomycetota and certain Bacillota undergo genome reduction, streamlining their genetic content to retain only essential virulence determinants [2]. This review systematically compares the molecular mechanisms, experimental evidence, and therapeutic implications of these critical virulence factors across major human bacterial pathogens.
Comparative Virulence Factor Distribution Across Ecological Niches
Large-scale genomic analyses of 4,366 bacterial pathogens isolated from different ecological niches reveal distinct enrichment patterns for specific virulence mechanisms. Human-associated pathogens demonstrate significantly higher detection rates for adhesion and immune evasion factors compared to isolates from animal or environmental sources [2].
Table 1: Virulence Factor Enrichment Across Ecological Niches
| Virulence Factor Category | Human-Associated Pathogens | Animal-Associated Pathogens | Environmental Pathogens |
|---|---|---|---|
| Immune Modulation Factors | Significantly enriched | Moderate | Low |
| Adhesion Factors | Significantly enriched | Variable | Low |
| Carbohydrate-Active Enzymes | High | Moderate | Variable |
| Antibiotic Resistance Genes | Clinical isolates highly enriched | Moderate (potential reservoirs) | Low |
| Metabolic Adaptation Genes | Moderate | Moderate | Highly enriched |
This niche-specific distribution reflects the selective pressures unique to the human host environment, where effective adhesion to human tissues and evasion of human immune responses provide critical survival advantages [2]. Animal hosts serve as important reservoirs for virulence and resistance genes, while environmental isolates prioritize metabolic versatility over specialized host interaction tools [2].
Molecular Mechanisms of Adhesion in Human-Associated Pathogens
Structural Diversity of Bacterial Adhesins
Bacterial adhesins represent a diverse array of surface-exposed molecules that facilitate attachment to host cells and tissues. These virulence factors can be broadly categorized into:
- Fimbrial adhesins: Filamentous protein structures that extend from the bacterial surface, such as the type 1 pili of uropathogenic Escherichia coli (UPEC) where the FimH tip adhesin binds specifically to mannose receptors on urinary epithelial cells [47].
- Afimbrial adhesins: Non-pilus adhesins including surface proteins covalently anchored to cell wall peptidoglycan, such as the microbial surface component recognizing adhesive matrix molecules (MSCRAMMs) in Staphylococcus aureus [48].
- Polysaccharide adhesins: Surface carbohydrates that mediate attachment, particularly in Gram-positive pathogens [49].
Table 2: Major Adhesin Families in Human Bacterial Pathogens
| Adhesin Family | Pathogen Examples | Host Receptor | Biological Function |
|---|---|---|---|
| MSCRAMMs | Staphylococcus aureus | Fibrinogen, fibronectin, collagen | Adhesion to extracellular matrix components [48] |
| Pili/Fimbriae | Uropathogenic Escherichia coli | Mannosylated receptors | Bladder and urinary tract colonization [47] |
| Terminal Organelle | Mycoplasma pneumoniae | Sialylated oligosaccharides | Respiratory epithelium attachment [50] |
| Serine-Rich Repeat | Streptococcus pneumoniae | Sialylated glycoconjugates | Mucosal colonization, biofilm formation [49] |
Specialized Adhesion Structures: The Mycoplasma pneumoniae Terminal Organelle
Mycoplasma pneumoniae employs a sophisticated attachment organelle representing a highly specialized adhesion machinery. This polar membrane protrusion features a bipartite architecture with surface-exposed nap-like proteins for host-pathogen interactions and an intricate internal structure that generates mechanical force for gliding motility [50].
The adhesion complex comprises four evolutionarily conserved surface proteins: P1 (MPN141), P90/P40 (MPN142 proteolytic cleavage products), and P30 (MPN453) [50]. Spatial organization places the P1 adhesin complex at the apical tip, forming a rigid membrane anchor, while P30 dynamically associates with the complex periphery to regulate force transduction during gliding [50]. This specialized structure enables M. pneumoniae to establish firm attachment to respiratory epithelium through recognition of sialylated oligosaccharides (SOS), particularly α-2,3-sialyllactose and α-2,6-sialyllactose, in a "lock-and-key" binding pattern [50].
Diagram 1: Molecular architecture of the M. pneumoniae terminal organelle showing surface adhesins and internal core structure that mediate host cell attachment.
Adhesion-Immune System Crosstalk
Beyond their canonical role in attachment, adhesins actively modulate host immune responses. The E. coli Afa/Dr adhesin family binds to decay-accelerating factor (DAF or CD55), a regulator of the complement cascade, and this interaction not only mediates bacterial adhesion but also interferes with the complement regulatory function of DAF by sterically hindering C3 convertase formation [49]. Furthermore, AfaE binding to the SCR-3 domain of DAF triggers pro-inflammatory signaling and increases expression of major histocompatibility complex class-I related molecule MICA, linking bacterial adhesion to innate immune activation [49].
Immune Evasion Mechanisms in Human-Associated Pathogens
Molecular Mimicry and Immune Deception
Pathogens employ molecular mimicry to evade detection by the host immune system. This strategy involves expressing proteins that structurally resemble host molecules, thereby reducing the number of recognizable foreign epitopes [51]. Comprehensive analysis of 134 human-infecting viruses revealed that chronic pathogens, particularly Herpesviridae and Poxviridae, exhibit significantly elevated rates of short linear amino acid mimicry compared to acute pathogens [51]. This mimicry preferentially targets host proteins involved in cellular replication, inflammatory responses, and specific chromosomal regions including autosomes and the X chromosome [51].
The "molecular mimicry trade-off hypothesis" posits that viruses must balance the immune evasion benefits of mimicry against potential constraints on protein function and replication efficiency [51]. Short linear epitope mimicry may represent an optimal solution, providing substantial immune evasion while minimizing detrimental effects on viral protein function [51]. This adaptation is particularly advantageous for chronic pathogens that establish long-term infections and require sustained evasion of host immunity.
Staphylococcal Immune Evasion Strategies
Staphylococcus aureus exemplifies the sophisticated immune evasion capabilities of human-adapted pathogens. Its extensive arsenal of virulence factors includes:
- Complement evasion: SdrE binds complement factor H to accelerate C3b degradation, while clumping factor A (ClfA) binds fibrinogen to mask bacterial surfaces from opsonization [48].
- Antibody interference: Protein A captures IgG Fc regions, positioning antibodies upside down and preventing effective opsonophagocytosis [48].
- Neutrophil resistance: IsdA confers resistance to bactericidal lipids and antimicrobial peptides, enhancing survival within neutrophils [48].
- Biofilm-mediated protection: The icaABCD operon promotes biofilm formation under neutrophil attack, creating physical barriers against phagocytic clearance [47].
Diagram 2: S. aureus immune evasion mechanisms targeting complement, antibodies, neutrophils, and phagocytic clearance.
Adhesion-Immune Evasion Coordination
The functional integration of adhesion and immune evasion is exemplified by Mycoplasma pneumoniae, whose terminal organelle mediates both attachment to respiratory epithelium and strategic positioning to avoid immune surveillance [50]. Adhesion triggers the release of hydrogen peroxide and CARDS toxin, simultaneously causing cytotoxic damage and modulating local immune responses [50]. This coordinated action enables M. pneumoniae to establish persistent infections despite the host's immune defenses.
Experimental Approaches and Methodologies
Comparative Genomic Analysis Protocols
The identification of niche-specific virulence factors relies on robust comparative genomic methodologies:
- Genome Collection and Curation: High-quality, non-redundant bacterial genome sequences are obtained from databases such as gcPathogen. Stringent quality control includes assembly quality assessment (N50 ≥50,000 bp), CheckM evaluation (completeness ≥95%, contamination <5%), and removal of genomes with unclear source information [2].
- Ecological Niche Annotation: Genomes are categorized based on detailed metadata of isolation sources and host information into human, animal, or environmental niches [2].
- Phylogenetic Analysis: Phylogenetic trees are constructed using 31 universal single-copy genes identified by AMPHORA2. Multiple sequence alignments are generated with Muscle v5.1, and maximum likelihood trees are built using FastTree v2.1.11 [2].
- Functional Annotation: Open reading frames are predicted using Prokka v1.14.6, with subsequent annotation against COG, CAZy (via dbCAN2), virulence factor (VFDB), and antibiotic resistance (CARD) databases [2].
Whole-Blood Infection Assays for Immune Evasion Assessment
Experimental quantification of immune evasion mechanisms employs standardized whole-blood infection assays:
- Experimental Setup: Fresh human whole blood is inoculated with bacterial pathogens at defined multiplicities of infection. Samples are incubated with rotation at 37°C for up to 24 hours [52].
- Kinetic Monitoring: Bacterial survival is quantified by plating serial dilutions at specific timepoints (0, 1, 2, 4, 8, 24 hours). Host immune cell populations and inflammatory mediators are simultaneously measured using flow cytometry and cytokine ELISA [52].
- Mathematical Modeling: Theoretical predictions are implemented through virtual infection models that simulate pathogen-immune interactions. The least-square error and Akaike information criterion are applied to compare different immune evasion hypotheses [52].
- Imaging Validation: Model predictions are experimentally validated using fluorescence microscopy and live-cell imaging to visualize pathogen interactions with immune cells [52].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Adhesion and Immune Evasion Factors
| Reagent/Category | Specific Examples | Research Application | Experimental Function |
|---|---|---|---|
| Genome Annotation Tools | Prokka v1.14.6, dbCAN2, VFDB | Comparative genomics | Functional categorization of virulence factors [2] |
| Phylogenetic Analysis Software | AMPHORA2, Muscle v5.1, FastTree v2.1.11 | Evolutionary analysis | Phylogenetic reconstruction and niche adaptation tracking [2] |
| Whole-Blood Infection Assay Components | Fresh human whole blood, flow cytometry antibodies, cytokine ELISA kits | Immune evasion quantification | Experimental measurement of bacterial survival in human blood [52] |
| Mathematical Modeling Platforms | Custom MATLAB/Python scripts for virtual infection modeling | Hypothesis testing | Computational assessment of immune evasion mechanisms [52] |
| Adhesion Inhibitors | Mannose derivatives, anti-FimH antibodies, receptor analogs | Therapeutic targeting | Blockade of specific pathogen-host adhesion interactions [53] [47] |
Therapeutic Implications and Future Directions
The targeted disruption of adhesion and immune evasion mechanisms represents a promising therapeutic strategy against antibiotic-resistant pathogens. Anti-adhesin antibodies against FimH in uropathogenic E. coli have demonstrated significant efficacy in animal models, reducing colonization through blockade of the critical initial attachment step [53]. Similarly, the Bordetella pertussis adhesins FHA and pertactin are key components in three of the four acellular pertussis vaccines licensed in the United States [53].
Future research directions include the development of multi-valent adhesion inhibitors that target redundant adhesion systems in pathogens like S. aureus, which expresses numerous functionally overlapping MSCRAMMs [48]. For immune evasion countermeasures, therapies targeting conserved aspects of molecular mimicry may provide broad-spectrum protection against viral pathogens [51]. Additionally, the co-evolution of virulence and antibiotic resistance genes on mobile genetic elements necessitates integrated therapeutic approaches that simultaneously target both pathogenicity and resistance mechanisms [47].
The continuing advancement of multi-omics integration, artificial intelligence, and CRISPR-based genome editing technologies will enable more precise dissection of adhesion and immune evasion pathways, accelerating the development of novel anti-infective strategies against human-adapted pathogens [47].
Animal Hosts as Key Reservoirs for Antimicrobial Resistance Genes
The emergence and spread of antimicrobial resistance (AMR) represent one of the most pressing global health challenges of our time. While often viewed primarily through the lens of human medicine, the AMR crisis is fundamentally intertwined with animal health and environmental ecosystems. The One Health framework recognizes that the health of humans, domestic and wild animals, plants, and the wider environment are closely linked and interdependent [54]. Within this framework, animal hosts—including livestock, companion animals, and wildlife—are increasingly identified as critical reservoirs for antimicrobial resistance genes (ARGs), playing an essential role in the evolution, maintenance, and dissemination of resistance elements across ecological niches.
The significance of animal reservoirs in the AMR landscape extends beyond their role as passive carriers. Intensive agricultural practices, particularly in food animal production, have created environments where selective pressures from antimicrobial use drive the evolution of resistant bacteria [55]. Meanwhile, wildlife species serve as bioindicators of environmental pollution by ARGs and as potential vectors for long-distance dissemination across geographic boundaries [56] [54]. The genetic connectivity between bacterial populations in human, animal, and environmental compartments facilitates a continuous exchange of resistance determinants, with mobile genetic elements acting as the primary vehicles for this horizontal gene transfer [57] [58].
This review synthesizes contemporary evidence on the role of animal hosts as reservoirs for ARGs, with a specific focus on comparative analysis across ecological niches. By examining the distribution of resistance genes and virulence factors in diverse animal species and their environments, we aim to elucidate the complex dynamics of AMR dissemination at the human-animal-environment interface and identify critical control points for intervention strategies.
ARG Distribution Across Animal Hosts and Ecological Niches
Reservoirs in Food Animal Production Systems
Food animal production systems represent significant hotspots for the emergence and dissemination of antimicrobial resistance. The extensive use of antibiotics in livestock farming—projected to exceed 107,472 tons globally by 2030—creates sustained selective pressure that enriches for resistant bacteria and mobile genetic elements carrying ARGs [55]. Quantitative metagenomic analyses reveal distinct patterns of ARG abundance and diversity across different agricultural sectors.
Table 1: Prevalence of Key Antibiotic Resistance Classes in Food Animal Production Systems
| Animal Sector | Dominant ARG Classes | Relative Abundance | Key Resistance Genes | Primary Reservoirs |
|---|---|---|---|---|
| Poultry | Tetracyclines, Macrolide-Lincosamide-Streptogramin (MLS), Aminoglycosides | 62.2% in droppings [57] | tetM, tetX, ermB, aadA | Droppings, litter, feed |
| Cattle | β-lactams, Aminoglycosides, Tetracyclines | 22.11 mg/PCU consumption [55] | blaTEM-1, tet(A), aph(3')-Ia | Manure, runoff water, soil |
| Swine | Tetracyclines, Macrolides, β-lactams | High in gut and waste products [55] | tet(O), ermF, cfxA | Manure, lagoon sediments |
| Aquaculture | Tetracyclines, Sulfonamides, Fluoroquinolones | 0.1% in fish intestine [57] | tetA, sul1, qnrS | Sediment, water column |
Integrated farming systems, where different animal species are raised in close proximity, create particularly conducive environments for ARG exchange. Metagenomic analysis of integrated chicken-fish farming systems in Bangladesh identified 384 distinct ARGs, with tetracycline resistance genes (tetM, tetX) being most abundant [57]. In these systems, animal droppings contained the highest proportion of ARGs (62.2%), followed by sediment (31.5%), highlighting the role of waste products as primary reservoirs. The close interaction between terrestrial and aquatic environments in such integrated systems facilitates the transfer of resistance determinants across microbial communities, with water serving as both habitat and vector for dissemination [57].
Beyond the immediate farm environment, ARGs from animal production systems enter surrounding ecosystems through multiple pathways, including agricultural runoff, wastewater discharge, and aerosolization. A study of water reservoirs near animal farms in Central China identified a high abundance of vancomycin resistance genes (vanT, vanY) and sulfonamide resistance genes (sul1, sul4) in both farm wastewater and connected drinking water sources, demonstrating the potential for environmental contamination and human exposure through water resources [59].
Companion Animals and Veterinary Settings
Companion animals, particularly dogs and cats, represent an important interface for antimicrobial resistance transmission due to their close contact with humans. A comprehensive study of Staphylococcus aureus isolates from veterinary clinics across five provinces in Thailand revealed substantial variations in AMR profiles between different host categories [60]. Veterinarians and veterinary assistants exhibited higher resistance rates compared to pet owners, highlighting the occupational risk associated with working in veterinary settings.
Table 2: Distribution of Antimicrobial Resistance Genes in Veterinary Clinic Isolates
| Host Category | β-lactam Resistance | Methicillin Resistance | Aminoglycoside Resistance | Quinolone Resistance | Macrolide/Lincosamide Resistance |
|---|---|---|---|---|---|
| Veterinarians | blaZ (86%) | mecA (24%) | aacA-aphD (15%) | gyrA, grlA (18%) | msrA, ermA (22%) |
| Veterinary Assistants | blaZ (82%) | mecA (18%) | aacA-aphD (12%) | gyrA, grlA (14%) | msrA, ermA (19%) |
| Pet Owners | blaZ (79%) | mecA (9%) | aacA-aphD (8%) | gyrA, grlA (7%) | msrA, ermA (11%) |
| Dogs | blaZ (81%) | mecA (21%) | aacA-aphD (16%) | gyrA, grlA (17%) | msrA, ermA (20%) |
| Cats | blaZ (77%) | mecA (11%) | aacA-aphD (23%) | gyrA, grlA (9%) | msrA, ermA (15%) |
The study further identified host-specific patterns in the distribution of resistance genes. The aminoglycoside resistance gene aacA-aphD was particularly common in cats (23%), while quinolone resistance genes (gyrA, grlA) were predominantly identified in veterinarians (18%) and dogs (17%) [60]. Agr typing of S. aureus isolates revealed diverse group distributions, with agr group I predominant in human samples and associated with the highest AMR gene expression, while agr group III was most prevalent in animal samples. These findings emphasize the potential for bidirectional transmission of resistant pathogens between companion animals and humans, with veterinary clinics serving as important interfaces for this exchange.
Wildlife as Sentinels and Vectors
Wildlife species serve as valuable bioindicators of environmental contamination with antimicrobial resistance genes while simultaneously acting as potential vectors for long-distance ARG dissemination. A study of wild birds in Tianjin, China, which examined the gut contents of 72 birds across 30 species, detected 10 high-risk ARGs and 4 mobile genetic elements (MGEs) [56]. The abundance of these resistance elements varied significantly with the birds' ecological traits, particularly their dietary habits and residency status.
The research revealed that carnivorous birds exhibited a higher abundance of certain high-risk ARGs compared to omnivores and herbivores, suggesting potential bioaccumulation through the food chain [56]. This finding aligns with the trophic dissemination hypothesis, which posits that ARGs and associated pathogens can transfer through food webs, with potential implications for human exposure through consumption of wild game or contaminated agricultural products.
Beyond local transmission, migratory birds pose a unique concern for the global dissemination of antimicrobial resistance. These species can acquire resistant bacteria in one geographic location and transport them over vast distances during seasonal migrations. As noted in a review on wildlife and antibiotic resistance, "migrating animals, such as gulls, fishes or turtles may participate in the dissemination of antibiotic resistance across different geographic areas, even between different continents, which constitutes a Global Health issue" [54]. This capacity for long-range dispersal distinguishes wildlife from domestic animal reservoirs and complicates containment efforts.
The role of wildlife in the AMR landscape is complex, as these species typically do not receive direct antibiotic exposure. Instead, the presence of clinically relevant ARGs in wildlife is largely interpreted as a marker of environmental pollution from human and agricultural sources [54]. Supporting this concept, studies of great apes have found that captive individuals harbor microbiomes enriched with human-associated bacterial species and higher abundances of ARGs compared to their wild counterparts, reflecting the interchange of bacteria between humans and animals through direct contact or shared environments [54].
Comparative Analysis of Virulence Factors Across Niches
Distribution of Virulence-Associated Genes
The co-occurrence of antimicrobial resistance genes and virulence factors in bacterial pathogens represents a particularly concerning combination, as it can lead to infections that are both difficult to treat and highly pathogenic. Comparative analyses across ecological niches reveal distinct patterns in the distribution of virulence-associated genes (VAGs) between human, animal, and environmental isolates.
A large-scale comparative genomic study analyzing 4,366 high-quality bacterial genomes found that human-associated bacteria, particularly from the phylum Pseudomonadota, exhibited higher detection rates of virulence factors related to immune modulation and adhesion, indicating co-evolution with the human host [2]. In contrast, bacteria from environmental sources showed greater enrichment in genes related to metabolism and transcriptional regulation, highlighting their adaptation to diverse environmental conditions rather than host colonization.
Research in integrated chicken-fish farming systems identified 445 types of virulence factor-associated genes belonging to 12 different mechanism classes [57]. The distribution of these virulence mechanisms varied significantly across sample types:
- Immune modulation factors were most abundant in fish intestine (67.01%) and sediment (3.07%)
- Effector delivery systems were highest in chicken gut (33.77%) and sediment (34.82%)
- Biofilm formation genes showed the greatest abundance in feed (27.52%), followed by chicken gut (11.4%)
These findings suggest that different ecological niches select for distinct virulence strategies, with bacterial pathogens adapting their pathogenic mechanisms to specific host environments and transmission routes.
Interplay Between Resistance and Virulence
The relationship between antimicrobial resistance and virulence is complex, with evidence supporting both trade-offs and synergistic interactions depending on the bacterial species and genetic context. Some studies suggest that the acquisition of resistance determinants may impose fitness costs that reduce virulence, while others indicate that certain resistance mutations can enhance pathogenic potential.
The co-localization of ARGs and VAGs on mobile genetic elements creates particularly concerning scenarios. A study of Escherichia coli populations in Hong Kong aquatic ecosystems identified 2647 circular plasmids, with 195 plasmids shared across human-associated, animal-associated, and environmental sectors [58]. Functional conjugation assays confirmed that several of these plasmids were transmissible across ecological boundaries, demonstrating the potential for co-transfer of resistance and virulence traits.
The convergence of multidrug resistance and enhanced virulence in successful bacterial clones poses significant challenges for clinical management. For instance, the extraintestinal pathogenic E. coli (ExPEC) lineage ST131, a globally disseminated and multidrug-resistant clone, was recovered from human, animal, and environmental sources in Hong Kong, underscoring its ecological adaptability and potential for cross-sectoral dissemination [58].
Molecular Mechanisms and Horizontal Gene Transfer
Mobile Genetic Elements as Key Dissemination Vehicles
The horizontal transfer of antimicrobial resistance genes between bacterial species is primarily mediated by mobile genetic elements (MGEs), including plasmids, transposons, integrons, and bacteriophages. These elements facilitate the movement of ARGs not only within bacterial populations in specific animal hosts but also across ecological boundaries between different compartments.
Metagenomic analysis of integrated chicken-fish farming systems revealed that plasmids and transposons like Tn6072 and Tn4001 were the most abundant MGEs, playing a critical role in horizontal gene transfer [57]. Bacterial genera including Bacteroides, Clostridium, and Escherichia showed strong associations with MGEs, indicating their importance as vectors for the dissemination of resistance and virulence traits.
A comprehensive genomic study of E. coli in Hong Kong aquatic ecosystems provided detailed insights into the plasmid-mediated dissemination of ARGs [58]. The researchers generated 1016 near-complete genomes using Nanopore long-read sequencing, which enabled high-resolution characterization of mobile genetic elements. This analysis identified 141 ARG subtypes across 15 antibiotic classes, many of which were plasmid-encoded. The study further documented 142 clonal strain-sharing events between human-associated and environmental water samples, highlighting the role of MGEs in facilitating the cross-sectoral transmission of resistance determinants.
Ecological Connectivity and Gene Exchange
The concept of ecological connectivity is central to understanding the dissemination of antimicrobial resistance in a One Health context. Genomic studies have developed frameworks to quantify this connectivity based on sequence type similarity, genetic relatedness, and clonal sharing between bacterial populations from different sources.
Research on E. coli in urban aquatic ecosystems of Hong Kong established that E. coli populations from human, animal, and environmental sources exhibited close genetic relatedness, with extensive sharing of strains and plasmids across these compartments [58]. To quantify these patterns, the researchers developed a genomic framework integrating sequence type similarity, genetic relatedness, and clonal sharing to assess ecological connectivity. Their results indicated that ecological connectivity facilitates AMR dissemination, highlighting the importance of integrated strategies to monitor and manage resistance risks across sectors.
The transfer of ARGs between wildlife and livestock, while potentially less frequent than other pathways, represents another important connectivity route. A study of microbial exchange at the wildlife-livestock interface found that ARG profiles differed among hosts (cattle, sheep, and common voles), suggesting that environmental acquisition rather than direct transmission between hosts was the primary mechanism [61]. Common voles harbored diverse ARGs, including resistance to tetracycline and vancomycin, which were likely acquired from the environment rather than through direct contact with livestock. These findings highlight the significant role of environmental reservoirs in shaping microbial communities and the spread of resistance, even in the absence of direct host-to-host transmission.
ARG Transmission from Animal Hosts to Human Health
Methodologies for ARG Detection and Surveillance
Culture-Based Approaches and Antimicrobial Susceptibility Testing
Traditional culture-based methods remain foundational for antimicrobial resistance surveillance in animal hosts. The standard protocol for antimicrobial susceptibility testing (AST) involves isolating bacterial strains from animal samples and determining their minimum inhibitory concentration (MIC) values against a panel of antibiotics.
In a study of Staphylococcus aureus from veterinary clinics, all isolates were examined for susceptibility to multiple antimicrobial classes using commercial Sensititre Companion Animal Gram Positive COMPGP1F Vet AST Plates [60]. The tested classes included β-lactams (ampicillin, penicillin, oxacillin + 2% NaCl), fluoroquinolones (enrofloxacin, marbofloxacin), glycopeptides (vancomycin), aminoglycosides (amikacin, gentamicin), macrolides (erythromycin), tetracyclines (doxycycline, minocycline), lincosamides (clindamycin), and others. The MIC values were interpreted according to Clinical and Laboratory Standards Institute (CLSI) guidelines, specifically using M100 for human isolates and VET01S for animal isolates [60].
The Multiple Antibiotic Resistance (MAR) index is frequently calculated to quantify an isolate's resistance profile, providing a measure of the extent of antibiotic resistance in microbial populations from animal hosts. The MAR index is calculated as a/b, where a represents the number of antibiotics to which an isolate is resistant, and b is the total number of antibiotics tested [60].
Molecular Detection of Resistance Genes
Polymerase chain reaction (PCR)-based methods enable the direct detection of specific antimicrobial resistance genes in bacterial isolates from animal hosts. The standard protocol involves DNA extraction from bacterial cultures followed by amplification with primers specific to target ARGs.
In the investigation of S. aureus from veterinary settings, bacterial genomic DNA was extracted using a commercial DNA extraction kit [60]. The PCR mixture with a total volume of 25 µL contained 1 µM of each AMR gene primer, 2 µM agr primer, 2.5 µL of 10 U Taq PCR buffer, 0.2 mM dNTP, 2 mM MgCl2, and 1 U Taq DNA polymerase. The thermal cycling conditions consisted of an initial denaturation at 95°C for 5 minutes, followed by 30 cycles of amplification at 95°C for 30 seconds, annealing at temperatures specific for each gene for 30 seconds, and extension at 72°C for 60 seconds, with a final extension step [60].
This approach allowed for the detection of various AMR genes, including blaZ (β-lactam resistance), mecA (methicillin resistance), aacA-aphD (aminoglycoside resistance), msrA (macrolide resistance), tetK (tetracycline resistance), and quinolone resistance genes (gyrA, grlA) [60].
Metagenomic Approaches for Resistome Analysis
Metagenomic sequencing has revolutionized the study of antimicrobial resistance in animal hosts by enabling comprehensive profiling of resistomes without the need for bacterial cultivation. This culture-independent approach allows for the detection of both known and novel ARGs across diverse microbial communities.
The standard workflow for metagenomic resistome analysis includes:
- DNA extraction from complex samples (feces, soil, water) using commercial kits or CTAB-based methods
- Library preparation through random fragmentation of genomic DNA followed by adapter ligation and PCR amplification
- High-throughput sequencing using platforms such as Illumina PE150
- Bioinformatic analysis including quality control, assembly, gene prediction, and annotation against ARG databases
In a study of water reservoirs and wastewater from animal farms, DNA was extracted using a commercial kit and the CTAB method [59]. After quality control, sequencing libraries were constructed and quantified via qPCR before sequencing on the Illumina platform. Bioinformatic analysis involved preprocessing raw data with Readfq, assembly using MEGAHIT software, prediction of open reading frames with MetaGeneMark, and redundancy removal with CD-HIT [59]. Taxon annotation was performed using DIAMOND software aligned against the NCBI Non-Redundant Protein Sequence database.
Metagenomic approaches have been particularly valuable for tracking the dissemination of ARGs through integrated farming systems. Research on integrated chicken-fish farming employed these methods to identify the abundance and transmission patterns of 384 distinct ARGs across environmental samples, revealing droppings as the primary reservoir (62.2% of total ARGs) and sediment as a hotspot for multi-metal resistance genes [57].
Metagenomic Workflow for ARG Detection
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for ARG Studies in Animal Hosts
| Category | Specific Products/Techniques | Application in ARG Research | Key Considerations |
|---|---|---|---|
| DNA Extraction Kits | Commercial kits (e.g., Geneaid, TianGen), CTAB method | Isolation of high-quality DNA from diverse sample matrices | Optimization needed for different sample types (feces, tissue, soil) |
| PCR Reagents | Taq DNA polymerase, dNTPs, specific primer sets, buffer systems | Amplification of target ARGs and mobile genetic elements | Primer design critical for specificity; optimization of annealing temperatures |
| AST Platforms | Sensititre COMPGP1F Vet AST Plates, MIC strips | Phenotypic confirmation of resistance patterns | Standardization according to CLSI (VET01S) or EUCAST guidelines |
| Sequencing Technologies | Illumina platforms, Nanopore R10.4.1 | Whole-genome sequencing, metagenomic resistome profiling | Long-read technologies better for mobile genetic element characterization |
| Bioinformatic Tools | MEGAHIT, MetaGeneMark, DIAMOND, CD-HIT | Data processing, assembly, gene prediction, and annotation | Pipeline validation essential for reproducible results |
| Reference Databases | CARD, NR database, VFDB | Annotation of ARGs, virulence factors, and taxonomic assignment | Regular updates needed to capture newly discovered genes |
The selection of appropriate research reagents and methodologies is critical for generating reliable and comparable data on antimicrobial resistance in animal hosts. The combination of culture-based, molecular, and metagenomic approaches provides complementary insights into the prevalence, diversity, and transmission dynamics of ARGs across different animal species and production systems.
Advanced sequencing technologies, particularly long-read platforms such as Nanopore R10.4.1, have significantly enhanced the ability to characterize mobile genetic elements involved in horizontal gene transfer [58]. These technologies enable the reconstruction of complete plasmids and other MGEs, providing insights into the genetic context of ARGs and their potential for cross-species transmission.
Bioinformatic tools and reference databases continue to evolve, supporting more comprehensive and accurate analysis of resistome data. The integration of these computational resources with experimental data is essential for understanding the complex epidemiology of antimicrobial resistance at the human-animal-environment interface.
Animal hosts constitute critical reservoirs for antimicrobial resistance genes, contributing significantly to the global AMR burden through complex transmission networks that span agricultural, companion animal, wildlife, and environmental compartments. The evidence synthesized in this review demonstrates that resistance genes are not uniformly distributed across these ecosystems but rather exhibit distinct patterns shaped by host species, management practices, and ecological factors.
The interconnectedness of human, animal, and environmental health underscores the necessity of a One Health approach to AMR surveillance and control. Integrated strategies that address antimicrobial use across all sectors, improve waste management practices, and enhance environmental protection are essential for mitigating the spread of resistance. Furthermore, the development of harmonized surveillance systems that track both resistance genes and their associated mobile genetic elements will provide crucial insights into transmission dynamics and enable more targeted interventions.
As research in this field advances, the application of cutting-edge genomic technologies and computational methods will continue to refine our understanding of the ecological and evolutionary drivers of AMR emergence and dissemination in animal hosts. This knowledge is fundamental to preserving the efficacy of antimicrobial agents for future generations and safeguarding global public health against the threat of untreatable infections.
The adaptive strategies of bacterial isolates are profoundly shaped by their ecological niches. Environmental isolates, originating from non-clinical settings such as soil and water, exhibit distinct genetic and phenotypic profiles compared to their clinical counterparts, particularly in their metabolic versatility and the regulation of virulence factors. These differences are critical for understanding bacterial evolution and have significant implications for drug development, as they can reveal potential targets for disrupting pathogenicity or enhancing biocontrol applications. This guide objectively compares the performance of environmental and clinical isolates across key genomic and phenotypic metrics, framing the analysis within the broader thesis of comparing virulence factors across ecological niches.
Comparative Genomics of Niche Adaptation
Comparative genomic analyses reveal that bacteria evolve niche-specific signatures. Environmental isolates often display a broader metabolic capacity for utilizing diverse energy sources and degrading complex compounds, whereas clinical isolates may show enrichment in genes facilitating host interaction and immune evasion.
Genomic Features of Enterobacter xiangfangensis
A study of Enterobacter xiangfangensis MDMC82, isolated from the Merzouga desert, provides a prime example of environmental adaptation [62]. Genomic analysis predicted a robust apparatus involved in:
- Stress Tolerance: Heat/cold shock response, drought and salinity tolerance.
- Metabolic Versatility: A variety of industrial enzymes (e.g., amylases, proteases, cellulases), aromatic compound degradation, and carbon storage/starvation response.
- Survival Mechanisms: Biofilm formation, motility, heavy metal resistance, and DNA repair systems [62]. Pan-genome analysis further highlighted pronounced metabolic and transcriptional versatility among environmental E. xiangfangensis isolates, suggesting remarkable genome plasticity driven by environmental pressures [62].
Large-Scale Genomic Comparison Across Niches
A large-scale comparative genomic analysis of 4,366 bacterial genomes isolated from various hosts and environments quantified niche-specific differences [3].
- Human-associated bacteria, particularly from the phylum Pseudomonadota, exhibited higher detection rates of carbohydrate-active enzyme (CAZy) genes and virulence factors related to immune modulation and adhesion [3].
- Bacteria from environmental sources, particularly from the phyla Bacillota and Actinomycetota, showed greater enrichment in genes related to metabolism and transcriptional regulation, highlighting their high adaptability to diverse environments [3].
- Clinical settings were characterized by a higher prevalence of antibiotic resistance genes, especially those related to fluoroquinolone resistance [3].
Table 1: Comparative Genomic and Phenotypic Features Across Ecological Niches
| Feature | Environmental Isolates | Clinical Isolates |
|---|---|---|
| Core Genome Size (E. xiangfangensis) | Larger, more plastic [62] | Smaller, more conserved [62] |
| Enrichment of Genes For | Metabolism, transcriptional regulation, stress response, aromatic compound degradation [62] [3] | Immune evasion, adhesion, antibiotic resistance [3] |
| Virulence Factor Detection Rate | Lower [3] | Higher [3] |
| Antibiotic Resistance Gene Detection Rate | Lower [3] | Higher (especially in clinical settings) [3] |
| Biotechnological Potential | High (e.g., industrial enzymes, bioremediation) [62] | Low |
| Key Adaptive Mechanism | Gene acquisition for metabolic versatility [62] | Genome reduction & specialized virulence factor acquisition [3] |
Experimental Data and Methodologies
Supporting experimental data and standardized protocols are essential for validating genomic predictions and enabling comparative research.
Key Experimental Protocols
The following table summarizes the core methodologies used in the cited studies to generate the comparative data.
Table 2: Key Experimental Protocols for Comparative Analysis
| Methodology | Description | Application in Featured Studies |
|---|---|---|
| Whole-Genome Sequencing & Assembly | High-quality DNA sequencing and reconstruction of genomic sequences, typically using Illumina platforms and assemblers like SPAdes [62]. | Used for all isolates in the compared studies to establish a foundational genomic dataset [62] [4]. |
| Pan-Genome Analysis | Analysis of the full complement of genes in a bacterial species, partitioning genes into core and accessory genomes using tools like Roary [62]. | Used to assess genomic diversity and identify niche-specific genes in E. xiangfangensis and A. alcaligenes [62] [63]. |
| Functional Annotation | Prediction of gene function by mapping to databases such as COG (Clusters of Orthologous Groups), VFDB (Virulence Factor Database), and CARD (Comprehensive Antibiotic Resistance Database) [62] [3]. | Identified genes involved in stress tolerance, metabolism, virulence, and antibiotic resistance across isolates from different niches [62] [3]. |
| Phenotypic Characterization | Laboratory assays to test traits like mucoviscosity, serum survival, biofilm formation, and infection potential in model organisms [4]. | Used to validate genomic predictions and demonstrate convergent evolution of reduced acute virulence and enhanced biofilm in K. pneumoniae [4]. |
Within-Host Evolution of a Pathogen
A study tracking the within-host evolution of a multidrug-resistant Klebsiella pneumoniae clone during a 5-year hospital outbreak provides a powerful example of niche-specific adaptation [4]. Genomic analysis revealed strong positive selection for mutations in key virulence factors like capsule synthesis (wzc, wcoZ), lipopolysaccharide (manB, manC), and iron utilization (sufB, sufC, fepA/fes) [4]. Phenotypic characterization showed that these mutations led to reduced acute virulence and enhanced biofilm formation, representing adaptations to the host environment that traded off transmission potential [4]. This underscores the dynamic nature of virulence regulation even on short time scales.
Diagram 1: Convergent evolutionary pathways in K. pneumoniae during a hospital outbreak. Within-host pressures select for mutations in specific virulence factors, leading to an adapted phenotype characterized by reduced acute virulence and enhanced biofilm formation [4].
The Scientist's Toolkit: Research Reagent Solutions
This table details key bioinformatics tools and databases essential for conducting the types of comparative genomic analyses described in this guide.
Table 3: Essential Research Reagents and Resources for Comparative Genomic Studies
| Reagent/Resource | Function | Application Example |
|---|---|---|
| SPAdes | Genome assembly from sequencing reads [62]. | De novo assembly of the E. xiangfangensis MDMC82 genome [62]. |
| Roary | Pan-genome analysis pipeline [62]. | Identification of core and accessory genes across 37 environmental E. xiangfangensis strains [62]. |
| NCBI PGAP | Automated annotation of prokaryotic genomes [62]. | Functional annotation of the E. xiangfangensis MDMC82 genome [62]. |
| VFDB (Virulence Factor Database) | Repository for virulence factors and associated genes [3] [63]. | Screening for virulence-associated genes in A. alcaligenes and other pathogens [3] [63]. |
| CARD (Comprehensive Antibiotic Resistance Database) | Database of antibiotic resistance genes and variants [3] [63]. | Annotation of antibiotic resistance determinants in A. alcaligenes and large-scale genomic comparisons [3] [63]. |
| COG (Clusters of Orthologous Groups) | Database for phylogenetic classification of proteins [3]. | Functional categorization of genes from bacterial genomes in comparative studies [3]. |
| IQ-TREE | Software for maximum likelihood phylogenetic inference [62]. | Construction of core-based phylogenetic trees for Enterobacter species [62]. |
Metabolic Niche Differentiation and Transcriptional Regulation
The interplay between metabolic capability and transcriptional regulation is a cornerstone of bacterial adaptation. Environmental isolates often maintain a broad transcriptional repertoire to sense and respond to diverse environmental cues.
Metabolic Specialization in Woeseiaceae
A comparative metagenomics study of Woeseiaceae from benthic (sediment) and planktonic (water column) marine environments revealed clear metabolic niche differentiation [64].
- Benthic Woeseiaceae MAGs possessed polysaccharide utilization loci (PULs) for degrading algal polysaccharides like laminarin and alginate, and genes for dissimilatory nitrate/nitrite and iron reduction [64].
- Particle-attached Planktonic Woeseiaceae MAGs lacked these PULs but encoded significantly more sulfatases and peptidases, suggesting specialization in degrading protein-rich and sulfated organic matter [64]. This demonstrates how taxonomically related groups can transcriptionally specialize for distinct ecological roles based on available substrates and redox conditions.
Transcriptional Regulation of Metabolic Fluxes
The relationship between transcriptional regulation and metabolic activity is complex. While transcription is crucial for producing metabolic enzymes, its direct control over metabolic fluxes is not always straightforward. Many metabolic enzymes are expressed at levels that are overabundant under steady-state conditions, creating a buffer that makes metabolic fluxes relatively insensitive to moderate changes in enzyme abundance [65]. This suggests that transcriptional regulation is essential for drastic metabolic reprogramming (e.g., switching carbon sources), but not for fine-tuning fluxes under stable conditions, where allosteric regulation may play a more immediate role [65]. This principle is likely a key differentiator between the "generalist" strategy of many environmental isolates and the "specialist" strategy of host-adapted pathogens.
Antimicrobial resistance (AMR) presents a distinct and pressing challenge across different ecological niches. The profiles of antibiotic resistance genes (ARGs), their associated virulence factors, and the genetic platforms that carry them differ markedly between clinical settings and community or environmental reservoirs. Understanding these contrasts is not merely an academic exercise; it is fundamental to designing effective surveillance and control strategies for multidrug-resistant pathogens. This guide synthesizes experimental data and genomic findings to objectively compare the resistance gene profiles, their genetic contexts, and functional implications in clinical versus community environments, providing a crucial resource for researchers and drug development professionals.
Comparative Analysis of Resistance Gene Prevalence
The distribution of clinically relevant ARGs varies significantly between human-associated microbiomes and environmental reservoirs. Table 1 summarizes the key contrasts in ARG profiles based on large-scale metagenomic and isolate genome analyses [66].
Table 1: Prevalence of Clinically Relevant Antibiotic Resistance Genes in Different Settings
| Resistance Gene | Resistance Mechanism | Prevalence in Human Gut Metagenomes | Prevalence in Hospital Effluent | Primary Taxonomic Restriction |
|---|---|---|---|---|
| cfiA | Carbapenemase | High | Not Specified | Bacteroides |
| CTX-M | Cephalosporinase | Low | Enriched | Proteobacteria |
| KPC | Carbapenemase | Very Low (<8/14,229 samples) | Enriched | Proteobacteria |
| NDM | Carbapenemase | Very Low (3/14,229 samples) | Enriched | Proteobacteria |
| VIM | Carbapenemase | Very Low | Enriched | Proteobacteria |
| IMP | Carbapenemase | Very Low | Enriched | Proteobacteria |
| OXA-48 | Carbapenemase | Very Low (5/14,229 samples) | Enriched | Proteobacteria |
| cfxA, cblA | Cephalosporinase | High | Not Specified | Bacteroides |
Data reveals that despite high global consumption of beta-lactam antibiotics, the most concerning carbapenemase genes (KPC, NDM, VIM, IMP) remain rare in the general human gut microbiome but are significantly enriched in hospital effluent [66]. Conversely, certain genes like cfiA and cfxA are highly prevalent in gut microbiomes but are taxonomically restricted to Bacteroides.
Virulence and Resistance Interplay Across Niches
The relationship between antimicrobial resistance and bacterial virulence is complex and context-dependent. Table 2 compares the resistance and virulence profiles of key pathogens isolated from clinical and informal community water sources, highlighting niche-specific adaptations [67].
Table 2: Comparison of Clinical and Environmental Isolates from Informal Settlements
| Characteristic | Enterococcus faecium | Klebsiella pneumoniae | Pseudomonas aeruginosa |
|---|---|---|---|
| Genetic Relatedness (Clinical vs. Environmental) | Low genetic relatedness for most isolates | Low genetic relatedness for most isolates | One clinical isolate (PAO1) showed high similarity to environmental strains |
| Predominant Resistance Profile | XDR (Extensively Drug-Resistant) in one clinical strain; MDR in others | MDR (Multidrug-Resistant) in all but one isolate | Higher antimicrobial susceptibility |
| Key Resistance Genes Detected | tetM (47.4%), blaKPC (52.6%) | blaKPC (15.4%) | Not Specified |
| Biofilm Formation | Poor biofilm formers | Moderate biofilm formers | Strong biofilm formers |
| Key Virulence Factors | Gamma-haemolytic, non-gelatinase producing | Gamma-haemolytic, non-hypermucoviscous, fimH+, ugE+ | Beta-haemolytic, gelatinase producing, phzM+, algD+ |
The study demonstrates that while clinical and environmental isolates can be genetically distinct, they can harbor similar antibiograms and virulence genes, indicating a flow of resistance and virulence traits between niches [67]. This is particularly evident in the detection of the carbapenemase gene blaKPC in environmental E. faecium and K. pneumoniae from water sources.
Molecular Mechanisms and Genetic Exchange
Regulation of Resistance Expression
Bacteria fine-tune the expression of resistance genes to balance the biological cost of resistance with the need to survive antibiotic challenge. A key regulatory mechanism is the two-component system (TCS), exemplified by the VanS/VanR system regulating glycopeptide resistance in enterococci [68].
Diagram: Two-component system regulating antibiotic resistance gene expression. The membrane-bound sensor kinase (VanS) detects an antibiotic, autophosphorylates, and transfers the phosphate to the response regulator (VanR), which then activates transcription of resistance genes.
In inducible resistance, the antibiotic itself acts as the signal, leading to its own detoxification. This sophisticated regulation allows bacteria to express resistance mechanisms efficiently while minimizing the fitness cost in the absence of antibiotic pressure [68].
Horizontal Gene Transfer and Mobile Genetic Elements
Horizontal gene transfer (HGT) is a primary driver of ARG dissemination between bacteria in different environments. The human gut, with its high bacterial density and diversity, is a hotspot for HGT [69]. Key mechanisms include:
- Conjugation: Transfer of plasmids or integrative conjugative elements (ICEs) through a conjugation pilus. The gut's mucus layer and high cell density create an environment favorable for this contact-dependent process [69].
- Transduction: Transfer of ARGs via bacteriophages. Antibiotic treatment can increase the number of ARG-carrying phages in the human gut [69].
- Transformation: Uptake of free environmental DNA.
- Membrane Vesicles: Membrane-derived vesicles that can transfer ARGs, such as beta-lactamases, between cells [69].
Plasmids are particularly crucial as they often carry multiple ARGs alongside virulence genes and bacteriocins, creating a multi-functional advantage for the host bacterium. For example, in E. coli, bacteriocin plasmids are strongly associated with extra-intestinal pathogenic (ExPEC) strains and are frequently co-located with virulence factors and AMR genes on large plasmids [70].
Experimental Protocols for Profiling Resistance and Virulence
Antimicrobial Susceptibility Testing (AST)
Protocol: The disk-diffusion method is a fundamental technique for phenotypically characterizing resistance profiles [71].
- Preparation: Prepare a standardized inoculum of the bacterial isolate in a saline or broth medium, adjusted to a 0.5 McFarland standard.
- Inoculation: Evenly spread the inoculum onto the surface of a Mueller-Hinton agar plate.
- Application: Aseptically place antibiotic-impregnated disks onto the inoculated agar surface.
- Incubation: Incubate the plates at 35°C for 16-18 hours.
- Analysis: Measure the diameter of the zone of inhibition around each disk. Interpret the results as Susceptible, Intermediate, or Resistant based on guidelines provided by the Clinical and Laboratory Standards Institute (CLSI) [71].
Virulence Gene Profiling via PCR
Protocol: Singleplex and multiplex PCR assays are used to detect virulence genes [71].
- DNA Extraction: Extract genomic DNA from overnight bacterial cultures using a commercial kit or standard thermal lysis method (e.g., incubation at 80°C for 30 minutes) [71].
- PCR Setup: Prepare a PCR reaction mix containing:
- GoTaq Green Master Mix (includes dNTPs, MgCl₂, and Taq polymerase)
- Forward and reverse primers specific to the target virulence genes (e.g., enterotoxins, adhesins, toxins)
- Template DNA
- Amplification: Perform PCR in a thermal cycler under conditions optimized for the primer sets. A typical program includes: initial denaturation at 94°C for 4 minutes; 30 cycles of denaturation (94°C for 30s), annealing (primer-specific temperature, e.g., 53°C for 30s), and extension (72°C for 1min); final extension at 72°C for 4 minutes [71].
- Visualization: Resolve PCR products by electrophoresis on an ethidium bromide-stained agarose gel and visualize under UV light.
Genetic Relatedness Analysis
Protocol: REP-PCR (Repetitive Extragenic Palindromic Sequence-Based Polymerase Chain Reaction) is used to fingerprint bacterial strains and assess outbreak relatedness [67].
- DNA Extraction: As in step 5.2.1.
- PCR Amplification: Perform PCR using primers targeting the repetitive REP sequences scattered throughout the bacterial genome.
- Fragment Separation: Separate the amplified DNA fragments using high-resolution gel electrophoresis (e.g., agarose).
- Pattern Analysis: Analyze the resulting banding patterns. Isolates with highly similar or identical patterns are considered closely related, potentially part of the same transmission chain.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for Resistance and Virulence Profiling
| Research Reagent / Kit | Primary Function | Example Application in Research |
|---|---|---|
| Wizard Genomic DNA Purification Kit (Promega) | High-quality genomic DNA extraction from bacterial cultures. | Template preparation for PCR-based virulence gene detection and SCCmec typing [71]. |
| GoTaq Green Master Mix (Promega) | Ready-to-use mix for standard PCR, containing Taq polymerase, dNTPs, MgCl₂, and loading dyes. | Amplification of virulence genes and molecular typing targets in singleplex and multiplex PCR assays [71]. |
| CLSI-Approved Antibiotic Disks | Standardized discs for antimicrobial susceptibility testing by disk diffusion. | Phenotypic profiling of resistance to anti-staphylococcal antibiotics (e.g., oxacillin, clindamycin, tetracycline) [71]. |
| Mueller-Hinton Agar | Standardized medium for antibiotic susceptibility testing. | Lawn culture for disk diffusion assays to ensure reproducible and interpretable results [71]. |
| Specific Primer Pairs | Oligonucleotides designed to bind and amplify specific target genes. | Detection of mecA, SCCmec types, virulence genes (e.g., sea, sei, lukE-lukD), and plasmid replicons [71]. |
The contrast between clinical and community ARG profiles is stark. Clinical settings are characterized by a higher prevalence of transferable, high-risk resistance genes (e.g., KPC, NDM) in classic pathogens, often linked with a full complement of virulence factors. In contrast, community and gut environments harbor a vast reservoir of diverse ARGs, but many of the most clinically worrying genes remain taxonomically restricted, despite being found on mobile elements. This suggests that barriers to gene exchange and expression between phyla are more significant than previously assumed. Future research and diagnostic efforts must therefore adopt a dual focus: continue rigorous surveillance of known high-risk clones in clinical settings while also investigating the ecological and genetic barriers that currently constrain the spread of the most dangerous resistance genes from environmental reservoirs into broad populations of human commensals.
Conclusion
The comparative analysis of virulence factors across ecological niches reveals that pathogenicity is often a byproduct of adaptation to specific environmental challenges, from protozoan predation to nutrient scarcity. Key takeaways include the critical role of horizontal gene transfer in spreading adaptive traits, the importance of animal and environmental reservoirs in the One Health framework, and the potential for niche-specific genes to serve as novel therapeutic targets. Future research must integrate multi-omics data with experimental models to functionally validate these adaptations. For biomedical and clinical research, this perspective is imperative for anticipating emerging pathogens, developing next-generation antimicrobials that disrupt niche-specific adaptations, and refining antibiotic stewardship programs to mitigate the spread of resistance from non-human reservoirs.
References
- 1. Virulence or Niche Factors: What's in a Name? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3486107/]
- 2. Comparative genomics reveals key adaptive mechanisms ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1543610/full]
- 3. Comparative genomics reveals key adaptive mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180303/]
- 4. Parallel within-host evolution alters virulence factors in an ... [https://www.nature.com/articles/s41467-025-64521-9]
- 5. Adaptative Divergence of Cryptococcus neoformans: Phenetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943092/]
- 6. Virulence factor activity relationships (VFARs) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5897045/]
- 7. VFDB: Virulence Factors of Bacterial Pathogens [https://www.mgc.ac.cn/VFs/main.htm]
- 8. Effect of environmental stress factors on the expression of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11865045/]
- 9. Context-dependent virulence in Klebsiella pneumoniae [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019290/]
- 10. Genetic comparison of virulence and resistance factors in ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969725021795]
- 11. VFDB 2025: an integrated resource for exploring anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11701737/]
- 12. Bacterial genome adaptation to niches: Divergence of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1343551/]
- 13. Freshwater genome-reduced bacteria exhibit pervasive ... [https://www.nature.com/articles/s41467-024-47767-7]
- 14. Detection of virulence factors in opportunistic bacteria [https://pmc.ncbi.nlm.nih.gov/articles/PMC12484208/]
- 15. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 16. The Rise of Pathogens: Predation as a Factor Driving the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3637895/]
- 17. Dual Role of Mechanisms Involved in Resistance to ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.01017/full]
- 18. Phages can constrain protist predation-driven attenuation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4139730/]
- 19. Considerations and caveats in anti-virulence drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5069136/]
- 20. Predators and nutrient availability favor protozoa-resisting ... [https://www.nature.com/articles/s41598-018-26422-4]
- 21. An expanded database and analytical toolkit for identifying ... [https://www.nature.com/articles/s41467-024-51864-y]
- 22. Accurate prediction of virulence factors using pre-train protein ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11694-8]
- 23. COG - Database Commons [https://ngdc.cncb.ac.cn/databasecommons/database/id/37]
- 24. The COG database: a tool for genome-scale analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC102395/]
- 25. CAZy - Home [https://www.cazy.org/]
- 26. Genomes [https://www.cazy.org/Genomes.html]
- 27. The Carbohydrate-Active EnZymes database (CAZy) [https://pmc.ncbi.nlm.nih.gov/articles/PMC2686590/]
- 28. Exploring Bacterial Virulence with Genome-wide ... [https://www.sciencedirect.com/science/article/abs/pii/S0966842X20303176]
- 29. aurora: a machine learning gwas tool for analyzing microbial ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03524-7]
- 30. Machine learning based on pangenome-wide association ... [https://www.nature.com/articles/s42003-025-08650-3]
- 31. A genome-wide One Health study of Klebsiella pneumoniae in ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01466-0]
- 32. Comparative genomics analysis and virulence-related factors ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-022-08663-w]
- 33. Computational Approaches for Discovering Virulence ... [https://www.mdpi.com/2309-608X/11/10/754]
- 34. Comparative genome analysis reveals key genetic factors ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-018-5043-9]
- 35. Evolutionary adaptation of probiotics in the gut [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145451/]
- 36. Antimicrobial activity and the presence of virulence factors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4518196/]
- 37. Genomic characterization and probiotic assessment of ... [https://www.nature.com/articles/s41598-025-98770-x]
- 38. Probiotic Features and Safety Assessment [https://pubmed.ncbi.nlm.nih.gov/41240266/]
- 39. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 40. An overview of the antimicrobial resistance mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604941/]
- 41. Captive environments reshape the compositions of carbohydrate active... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-03863-2]
- 42. A roadmap for gene functional characterisation in crops with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7093151/]
- 43. Assessment of Antimicrobial Resistance and Virulence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466447/]
- 44. Detection of virulence factors in opportunistic bacteria [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1638925/full]
- 45. Virulence factors, biofilm formation and antifungal ... [https://www.nature.com/articles/s41598-025-21846-1]
- 46. Antimicrobial Resistance: A Growing Serious Threat for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10340576/]
- 47. International Journal of Molecular Medicine [https://www.spandidos-publications.com/10.3892/ijmm.2025.5614]
- 48. Adhesion, invasion and evasion: the many functions of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5708296/]
- 49. Adhesin - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/adhesin]
- 50. Advances in adhesion-related pathogenesis in Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325244/]
- 51. Molecular mimicry as a mechanism of viral immune ... [https://www.nature.com/articles/s41467-024-53658-8]
- 52. Comparative assessment of immune evasion mechanisms ... [https://pubmed.ncbi.nlm.nih.gov/33793643/]
- 53. 14.1D: Adherence [https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_(Boundless)/14%3A_Pathogenicity/14.01%3A_Entry_into_the_Host/14.1D%3A_Adherence]
- 54. Wildlife and Antibiotic Resistance [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.873989/full]
- 55. Antibiotic Resistance Genes in Food Animal Production [https://www.mdpi.com/2076-3298/12/11/427]
- 56. Intestinal microbiota and high-risk antibiotic resistance ... [https://www.sciencedirect.com/science/article/abs/pii/S0013935124019479]
- 57. Abundance and transmission of antibiotic resistance ... [https://www.nature.com/articles/s41598-025-92921-w]
- 58. Ecological connectivity of genomic markers of antimicrobial ... [https://www.nature.com/articles/s41467-025-62455-w]
- 59. Analysis of Antibiotic Resistance Genes in Water ... [https://www.mdpi.com/2076-2607/12/2/396]
- 60. A Comparative Analysis of Antimicrobial Resistance Patterns ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12303630/]
- 61. Microbial exchange at the wildlife-livestock interface [https://pmc.ncbi.nlm.nih.gov/articles/PMC12330063/]
- 62. Comparative genomics uncovers adaptive and ... [https://www.nature.com/articles/s41598-025-25044-x]
- 63. Pangenome analysis of Aquipseudomonas alcaligenes 67P [https://www.sciencedirect.com/science/article/pii/S3050641725000102]
- 64. Comparative metagenomics indicates metabolic niche ... [https://environmentalmicrobiome.biomedcentral.com/articles/10.1186/s40793-025-00732-3]
- 65. the role of transcription in regulating microbial metabolic ... [https://www.sciencedirect.com/science/article/abs/pii/S0958166913000712]
- 66. Clinically relevant antibiotic resistance genes are linked to ... [https://www.nature.com/articles/s41467-023-42998-6]
- 67. Comparing antibiotic resistance and virulence profiles of ... [https://www.sciencedirect.com/science/article/pii/S2405844024062467]
- 68. Modes and Modulations of Antibiotic Resistance Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1797629/]
- 69. Exploring the role of gut microbiota in antibiotic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11915737/]
- 70. Bacterial warfare is associated with virulence and ... [https://www.nature.com/articles/s41467-025-64363-5]
- 71. Comparison of antibiotic resistance, virulence gene profiles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4216751/]