Integrating Genomic Sciences with a One Health Approach: From Pathogen Surveillance to Precision Medicine
This article explores the transformative role of genomic sciences within the One Health framework, which recognizes the interconnectedness of human, animal, and environmental health.
Integrating Genomic Sciences with a One Health Approach: From Pathogen Surveillance to Precision Medicine
Abstract
This article explores the transformative role of genomic sciences within the One Health framework, which recognizes the interconnectedness of human, animal, and environmental health. Aimed at researchers, scientists, and drug development professionals, it covers foundational concepts, methodological applications, and optimization strategies for genomic surveillance and analysis. The content delves into how cross-species genomic data is revolutionizing pandemic preparedness, antimicrobial resistance (AMR) tracking, and the management of zoonotic diseases. It also addresses critical challenges in data integration and bioinformatics, evaluates the comparative effectiveness of One Health genomics against traditional siloed approaches, and discusses future directions for implementing these technologies in biomedical research and clinical practice.
The One Health Genomic Paradigm: Connecting Human, Animal, and Ecosystem Health
Defining the One Health Framework and Its Imperative in Modern Genomics
The One Health framework represents a transformative approach to public health that recognizes the inextricable linkages between human, animal, and environmental health. This whitepaper examines the critical imperative of integrating One Health principles with modern genomic sciences to address complex global health challenges. Through advanced genomic technologies including high-throughput sequencing, bioinformatic analyses, and real-time surveillance, researchers can now decode complex biological interactions across species and ecosystems with unprecedented precision. This technical guide explores methodological frameworks, experimental protocols, and practical applications of genomics within the One Health paradigm, providing researchers and drug development professionals with actionable strategies for implementing integrated health solutions.
Conceptual Foundation and Definition
One Health is defined as "an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals, and ecosystems" [1] [2]. This approach recognizes that the health of humans, domestic and wild animals, plants, and the wider environment are closely linked and interdependent [1]. The framework mobilizes multiple sectors, disciplines, and communities at varying levels of society to work together to foster well-being and tackle threats to health and ecosystems while addressing collective needs for healthy food, water, energy, and air [2].
The conceptual foundation of One Health rests on several key principles [3] [2]:
- Equity between sectors and disciplines
- Sociopolitical and multicultural parity and inclusion of marginalized voices
- Socioecological equilibrium seeking harmonious balance in human-animal-environment interactions
- Stewardship and responsibility for sustainable solutions
- Transdisciplinarity and multisectoral collaboration across modern and traditional knowledge systems
Historical Evolution and Contemporary Relevance
While the interconnectedness of human, animal, and environmental health has been recognized for centuries, the formalized One Health concept gained significant traction in the early 2000s in response to emerging zoonotic diseases [4]. The Manhattan Principles established in 2004 by the Wildlife Conservation Society represented a pivotal milestone, explicitly recognizing the critical links between human and animal health and the threats diseases pose to food supplies and economies [3] [4]. This was subsequently refined through the Berlin Principles, which expanded the conceptual framework [3].
The SARS outbreak in 2003 and the subsequent spread of highly pathogenic avian influenza H5N1 demonstrated the necessity of collaborative, cross-disciplinary approaches to emerging infectious diseases [4]. These events catalyzed international cooperation and institutional recognition of One Health, leading to the formation of the One Health High-Level Expert Panel (OHHLEP) in 2020 by the Quadripartite organizations: the Food and Agriculture Organization (FAO), the World Organisation for Animal Health (WOAH), the World Health Organization (WHO), and the United Nations Environment Programme (UNEP) [3] [2].
The COVID-19 pandemic has further underscored the urgent need for strengthened One Health approaches, with greater emphasis on connections to the environment and promoting healthy recovery [1]. The pandemic revealed how deeply human health is intertwined with animal health and ecosystem integrity, highlighting the necessity of genomic tools for understanding pathogen emergence and transmission dynamics [5] [6].
The Integration of Genomics into One Health Applications
Genomic Technologies Enabling One Health Solutions
Modern genomic technologies have revolutionized our ability to operationalize the One Health framework across human, animal, and environmental domains. These technologies provide powerful tools for understanding pathogen evolution, transmission dynamics, and host-pathogen interactions at unprecedented resolution [3].
Table 1: Genomic Technologies in One Health Applications
| Technology | Key Features | One Health Applications | References |
|---|---|---|---|
| Nanopore Sequencing | Portable, real-time sequencing, long reads, direct RNA sequencing | Field-based pathogen detection, outbreak surveillance, antimicrobial resistance monitoring | [5] |
| Whole Genome Sequencing (WGS) | Comprehensive genomic data, high resolution | Pathogen characterization, transmission tracking, antimicrobial resistance research | [6] |
| Metagenomic Next-Generation Sequencing (mNGS) | Culture-independent, unbiased pathogen detection | Novel pathogen discovery, microbiome studies, environmental surveillance | [7] |
| Bioinformatic Pipelines | Data integration, computational analysis, visualization | Genomic epidemiology, phylogenetic analysis, predictive modeling | [6] [3] |
Nanopore sequencing represents a particularly transformative technology for One Health applications due to its portability and real-time capabilities [5]. This technology enables genomic analyses in field settings and local laboratories, making genomic surveillance accessible in resource-limited environments common in tropical regions where many emerging zoonotic diseases originate [5] [7]. The MinION device, for example, has been deployed worldwide to break down barriers and improve the accessibility and versatility of genomic sequencing [5].
The declining costs of DNA sequencing have further accelerated the adoption of genomic technologies in One Health contexts. However, this has created new challenges in data management, with annual acquisition of raw genomic data worldwide expected to exceed one zettabyte (one trillion GB) by 2025 [6]. This massive data generation necessitates robust bioinformatic infrastructure and scalable computational workflows to transform raw sequence data into actionable insights [6].
Methodological Framework for Genomic One Health Implementation
Implementing genomic technologies within a One Health framework requires systematic approaches that coordinate activities across human, animal, and environmental sectors. The Generalizable One Health Framework (GOHF) provides a structured five-step process for developing capacity to coordinate zoonotic disease programming across sectors [8]:
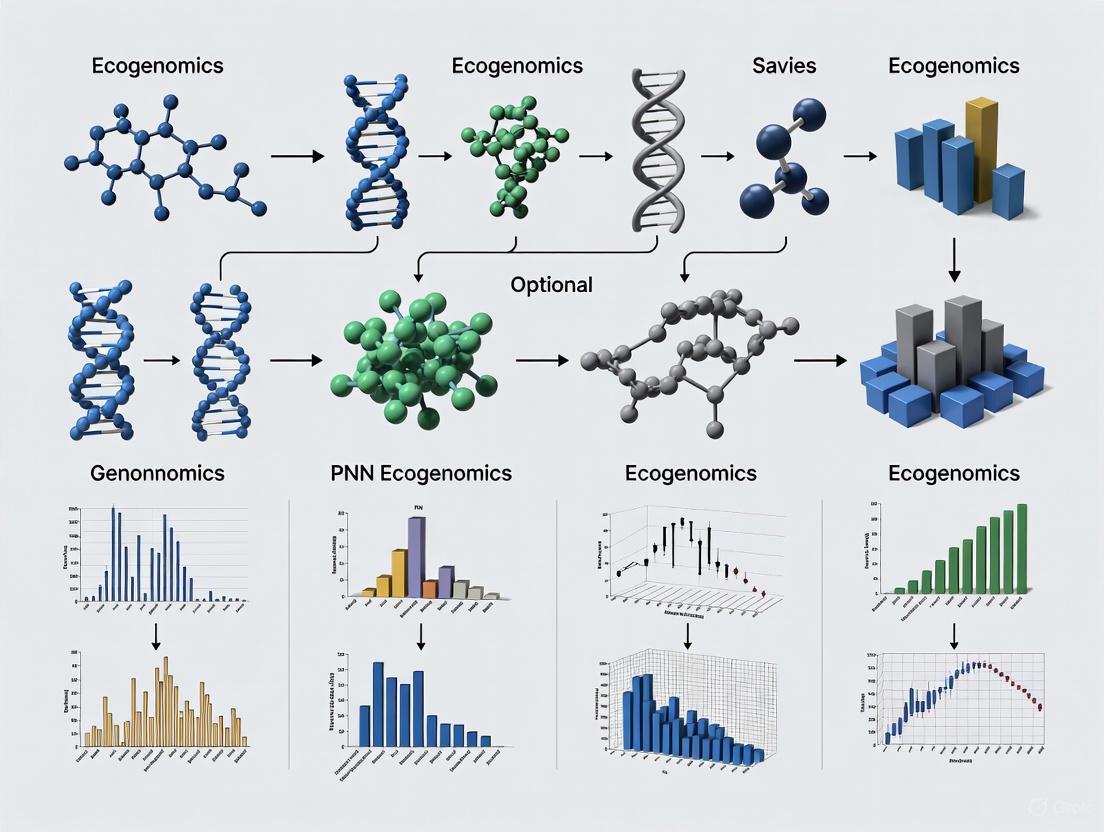
Figure 1: Generalizable One Health Framework (GOHF) for implementing genomic surveillance systems
Step 1: Engagement involves establishing One Health interest by identifying and engaging stakeholders across relevant sectors. This includes prioritizing zoonotic diseases through formalized processes like the One Health Zoonotic Disease Prioritization (OHZDP) and establishing sustained government support [8].
Step 2: Assessment focuses on mapping existing infrastructure and establishing baseline information on current activities, disease burden, and epidemiologic situations. Infrastructure mapping visualizes mechanisms of communication, collaboration, and coordination between sectors [8].
Step 3: Planning develops strategic roadmaps that define specific objectives, interventions, and resource requirements for genomic One Health implementation. This includes developing integrated surveillance plans that incorporate genomic data from human, animal, and environmental sources [8].
Step 4: Implementation executes the planned activities through coordinated action across sectors. This includes establishing laboratory networks, data sharing platforms, and joint response protocols that leverage genomic technologies [8].
Step 5: Evaluation assesses the effectiveness of implemented activities and systems, using monitoring data to refine approaches and improve outcomes in an iterative process [8].
Technical Approaches and Experimental Protocols
Genomic Surveillance Methodologies
Implementing genomic surveillance within a One Health framework requires standardized methodologies that enable comparable data generation across human, animal, and environmental samples. The following protocols outline key approaches for integrated genomic surveillance:
Protocol 1: Cross-Species Pathogen Genomic Surveillance
- Sample Collection: Coordinate synchronized collection of specimens from human cases, domestic animals, wildlife, and relevant environmental sources (water, soil) using standardized sampling protocols [6] [7].
- Nucleic Acid Extraction: Extract DNA and/or RNA using kits that accommodate diverse sample matrices. Implement controls to monitor extraction efficiency and potential contamination [5] [7].
- Library Preparation: Prepare sequencing libraries using approaches appropriate for the sequencing platform. For nanopore sequencing, this typically involves ligation sequencing kits with native barcoding to enable multiplexing [5].
- Sequencing: Perform sequencing on appropriate platforms. For real-time surveillance, utilize portable nanopore sequencers (MinION, GridION) that enable field-based sequencing [5].
- Bioinformatic Analysis:
- Perform quality control on raw sequencing data (FastQC, NanoPlot)
- Conduct metagenomic classification (Kraken2, Centrifuge) or pathogen-specific assembly (SPAdes, Canu)
- Generate phylogenetic trees (IQ-TREE, BEAST) to infer transmission dynamics
- Screen for antimicrobial resistance genes (ABRicate, CARD) and virulence factors [5] [6] [7]
Protocol 2: Metagenomic Monitoring of Antimicrobial Resistance
- Sample Collection: Collect samples from targeted reservoirs (human clinical specimens, livestock feces, agricultural soil, wastewater) using consistent sampling methods [6].
- DNA Extraction: Perform high-throughput DNA extraction suitable for diverse sample types. Include extraction controls to monitor performance [6].
- Shotgun Metagenomic Sequencing: Prepare libraries without amplification bias and sequence using Illumina or nanopore platforms to achieve sufficient depth for resistance gene detection [6].
- Computational Analysis:
- Trim and quality filter raw reads (Trimmomatic, Porechop)
- Align reads to curated AMR databases (MEGARes, CARD)
- Quantify abundance of resistance genes and mobile genetic elements
- Perform statistical analyses to compare resistance profiles across reservoirs [6]
Reagent Solutions for One Health Genomics
Table 2: Essential Research Reagents for One Health Genomic Applications
| Reagent Category | Specific Products | Application in One Health Genomics | Technical Considerations |
|---|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp DNA/RNA Mini Kit, DNeasy PowerSoil Pro Kit | Efficient extraction from diverse sample matrices (clinical, environmental, veterinary) | Optimize protocols for different sample types; include inhibition removal steps |
| Library Preparation Kits | Nextera XT DNA Library Prep, Ligation Sequencing Kit (Nanopore) | Preparation of sequencing libraries from minimal input DNA | Select kits based on sequencing platform; consider multiplexing requirements |
| Portable Sequencing Devices | MinION, SmidgION (Oxford Nanopore) | Real-time genomic surveillance in field settings | Leverage portability for deployment in remote locations; optimize power supply |
| Target Enrichment Systems | Twist Target Enrichment, SureSelect XT HS | Focused sequencing of pathogen genomes from complex samples | Design panels to cover priority pathogens; optimize for cross-species detection |
| Bioinformatic Tools | CLC Genomics Workbench, Galaxy Platform, BV-BRC | Integrated analysis of genomic data from multiple sectors | Ensure compatibility across data types; implement reproducible workflows |
Data Analysis and Bioinformatics Integration
Computational Frameworks for One Health Genomics
The integration of genomic data within a One Health context requires sophisticated bioinformatic frameworks capable of processing and analyzing heterogeneous datasets from multiple sources. Effective implementation relies on computational infrastructures that support data integration, analysis, and interpretation across disciplinary boundaries [6] [3].
Automated analysis pipelines such as the Automatic Bacterial Isolate Assembly, Annotation and Analyses Pipeline (ASA3P) provide standardized approaches for processing genomic data from diverse sources [6]. These pipelines enable reproducible analyses that facilitate comparisons across human, animal, and environmental isolates, supporting integrated surveillance and outbreak investigations.
Cloud computing infrastructures have become essential for managing the computational demands of One Health genomics. By sharing computational resources across multiple users and institutions, cloud platforms enable scalable analyses while minimizing costs associated with maintaining local computational infrastructure [6]. This approach is particularly valuable for resource-limited settings where establishing local high-performance computing capacity may be challenging.
Data Integration and Visualization
Integrating genomic data with epidemiological, environmental, and clinical information creates a powerful foundation for One Health analytics. The relationships between these data types can be visualized through the following framework:
Figure 2: Data integration framework for One Health genomics
Key data types integrated in this framework include:
- Genomic Data: Pathogen genomes, antimicrobial resistance genes, virulence factors, host genetic information [6] [3]
- Epidemiological Data: Case reports, exposure histories, transmission patterns, risk factors [8]
- Environmental Data: Climate variables, land use patterns, ecological parameters, pollution indicators [1] [7]
- Clinical Data: Patient outcomes, treatment responses, comorbidity information [9]
The integration of these diverse data streams enables the development of predictive models for disease emergence and spread, facilitates molecular epidemiology to track transmission pathways across species boundaries, and supports risk assessment for targeted interventions [3] [8].
Applications in Disease Control and Prevention
Zoonotic Disease Surveillance and Outbreak Response
Genomic technologies have transformed our approach to zoonotic disease surveillance and outbreak response within the One Health framework. Several key applications demonstrate the power of integrated genomic surveillance:
Emerging Infectious Disease Detection: The real-time genomic capabilities of nanopore sequencing have enabled rapid detection and characterization of emerging pathogens at the human-animal-environment interface [5] [7]. During the COVID-19 pandemic, genomic surveillance demonstrated how SARS-CoV-2 variants emerged and spread between human and animal populations, informing targeted control measures [5] [6].
Outbreak Investigation: Whole genome sequencing provides high-resolution data for tracking transmission pathways during zoonotic disease outbreaks. Genomic epidemiology has been successfully applied to investigate outbreaks of diseases including Ebola virus, MERS-CoV, and zoonotic influenza, revealing patterns of both human-to-human and animal-to-human transmission [6] [8]. The application of genomic data during the 2013-2016 Ebola outbreak in West Africa, for example, enabled researchers to distinguish between sustained human-to-human transmission and repeated zoonotic introductions [6].
Table 3: Genomic Applications in Zoonotic Disease Management
| Disease Category | Genomic Application | One Health Impact | References |
|---|---|---|---|
| Zoonotic Influenza | Whole genome sequencing to track reassortment events and host adaptations | Informed vaccine strain selection and animal control measures | [6] [8] |
| Antimicrobial Resistance | Metagenomic sequencing to track resistance genes across reservoirs | Identified transmission pathways between clinical, agricultural, and environmental settings | [6] [7] |
| Foodborne Pathogens | Genomic溯源 of Salmonella, E. coli, and Campylobacter along food production chains | Enabled targeted interventions at critical control points from farm to consumer | [9] [8] |
| Vector-Borne Diseases | Pathogen genomics combined with vector and host genetics | Revealed complex transmission cycles involving multiple host species | [7] |
Antimicrobial Resistance (AMR) Monitoring
The spread of antimicrobial resistance represents a quintessential One Health challenge that benefits significantly from genomic approaches. Resistance genes can move between bacteria inhabiting humans, animals, and the environment, requiring integrated surveillance across all reservoirs [6] [4].
Genomic studies have revealed that 73% of the global antimicrobial consumption occurs in livestock production, contributing significantly to the emergence and dissemination of resistance genes [6]. The use of genomics has enabled researchers to track the flow of specific resistance mechanisms between agricultural settings, the environment, and clinical environments, informing interventions to slow the spread of resistance [6].
The comprehensive nature of genomic data provides distinct advantages for AMR surveillance compared to traditional phenotypic methods. Whole genome sequencing enables detection of known resistance determinants alongside emerging mechanisms, supports analysis of mobile genetic elements that facilitate resistance gene transfer, and allows for tracking of resistant clones across sectors and geographic boundaries [6].
Implementation Challenges and Ethical Considerations
Technical and Infrastructural Barriers
Despite the demonstrated value of genomic technologies in One Health applications, significant implementation challenges remain:
Resource Limitations: The infrastructure required for genomic sequencing—including reliable electricity, cold chain storage, and computational resources—may be unavailable in many resource-limited settings where zoonotic disease threats are most prominent [7]. Portable sequencing technologies such as the MinION have helped address some of these barriers, but challenges remain in establishing sustainable sequencing capacity [5] [7].
Bioinformatic Capacity: The analysis of genomic data requires specialized computational skills that may not be available across all sectors involved in One Health implementation [6] [7]. Building bioinformatic capacity through training programs and developing user-friendly analytical platforms are essential for expanding access to genomic technologies [6].
Data Integration Challenges: Combining genomic data with epidemiological, clinical, and environmental information presents technical challenges related to data standardization, interoperability, and visualization [3]. Developing common data standards and interoperable platforms is critical for maximizing the utility of genomic data in One Health decision-making [3] [8].
Ethical and Equity Considerations
The application of genomic technologies within One Health raises important ethical considerations that must be addressed:
Equitable Access: There is significant disparity in genomic sequencing capacity between high-income and low-to-middle-income countries, creating an imbalance in who benefits from genomic research [3] [7]. This inequity is particularly problematic since many emerging zoonotic diseases originate in tropical regions where sequencing capacity may be most limited [7].
Data Sovereignty: Genomic research involving biological samples from low and middle-income countries has historically often extracted resources and data without ensuring equitable sharing of benefits [5] [7]. Principles such as the CARE (Collective Benefit, Authority to Control, Responsibility, Ethics) principles for Indigenous Data Governance and the Nagoya Protocol on Access and Benefit Sharing provide frameworks for ensuring that communities and countries maintain authority over their genetic resources and associated data [5].
Digital Colonialism: The dominance of high-income countries in genomic research can lead to inequities where data are extracted from low and middle-income countries but analyzed and utilized elsewhere, limiting local capacity building and benefit [3] [7]. Building local sequencing and bioinformatic capacity through initiatives like the Africa BioGenome Project represents an important step toward addressing these imbalances [7].
Emerging Technologies and Methodological Advances
The future of One Health genomics will be shaped by several technological and methodological developments:
Real-Time Genomic Surveillance: The increasing portability and decreasing cost of sequencing technologies will enable more widespread implementation of real-time genomic surveillance at the human-animal-environment interface [5]. The integration of automated sample preparation with portable sequencers will further enhance capabilities for rapid response to emerging threats.
Single-Cell Genomics: Advances in single-cell sequencing will enable more precise characterization of microbial communities and host-pathogen interactions across different reservoirs, providing unprecedented resolution for understanding transmission dynamics [5].
AI-Enhanced Analytics: Artificial intelligence and machine learning approaches will increasingly support the integration of genomic data with other data types, enabling more sophisticated predictive models for disease emergence and spread [10]. These approaches will help identify subtle patterns across complex datasets that may not be apparent through conventional analytical methods.
Pan-Genome Representations: Moving beyond single reference genomes to pan-genome representations that capture the full diversity of pathogens and hosts will enhance our ability to track transmissions and understand adaptive evolution [5]. This approach is particularly valuable for pathogens with significant genomic diversity or those that rapidly evolve in response to selective pressures.
The integration of modern genomic technologies within the One Health framework represents a powerful paradigm for addressing complex health challenges at the human-animal-environment interface. Genomic tools provide unprecedented capabilities for tracking pathogen transmission, understanding antimicrobial resistance dissemination, and detecting emerging threats across species boundaries.
The effective implementation of One Health genomics requires collaborative frameworks that coordinate activities across human health, animal health, and environmental sectors [8]. Methodological standards for genomic surveillance, data sharing, and bioinformatic analysis must be established to enable comparable data generation and interpretation across disciplines [6] [3].
As genomic technologies continue to evolve, their application within One Health approaches will become increasingly essential for global health security. By fostering interdisciplinary collaboration and building capacity across sectors and geographic regions, the scientific community can harness the power of genomics to promote health for people, animals, and ecosystems in an increasingly interconnected world.
Genomics as a Cross-Cutting Tool for Integrated Health Surveillance
The integration of genomic technologies into public health surveillance represents a paradigm shift in how we detect, monitor, and respond to health threats. Framed within the broader One Health context that recognizes the interconnectedness of human, animal, and environmental health, genomic surveillance provides unprecedented insights into pathogen evolution, transmission dynamics, and host-pathogen interactions across species and ecosystems [11]. This technical guide examines core applications, methodologies, and implementation frameworks for leveraging genomics as a cross-cutting tool in integrated health surveillance systems, with particular relevance for researchers, scientists, and drug development professionals working at the intersection of human, animal, and environmental health.
The One Health concept underscores that health outcomes across human, animal, and environmental domains are intrinsically linked, necessitating integrated, transdisciplinary approaches to address contemporary health challenges [11]. Genomic technologies serve as a foundational tool within this framework by enabling precise characterization of pathogens and their movements across interfaces. The dramatic reduction in sequencing costs—from approximately $10 million per megabase of DNA sequence in 2001 to less than one cent today—has made these tools increasingly accessible and scalable for routine public health applications [12] [13].
Next-generation sequencing (NGS) and whole-genome sequencing (WGS) provide higher resolution than traditional subtyping technologies, enabling more accurate cluster detection, transmission tracing, and phenotypic characterization of pathogens [13]. When genomic data are integrated with epidemiological, clinical, and environmental information through integrated genomic surveillance (IGS) systems, public health agencies can achieve earlier detection of outbreaks, better understanding of transmission pathways, and more targeted interventions [14]. This approach is particularly valuable for addressing zoonotic diseases, which account for up to 75% of new or emerging infectious diseases and require coordinated investigation across human and animal populations [15].
Core Applications and Quantitative Impact
Genomic surveillance delivers actionable insights across diverse public health domains, from foodborne illness outbreaks to antimicrobial resistance monitoring. The table below summarizes key application areas with specific examples and documented impacts.
Table 1: Applications and Documented Impact of Genomic Surveillance in Public Health
| Application Area | Specific Use Cases | Key Impact Metrics | References |
|---|---|---|---|
| Outbreak Detection & Investigation | Foodborne pathogens (Listeria, Salmonella), COVID-19 variant tracking | Listeria: Increased detected clusters from 14 to 21 annually; median cases per cluster decreased from 6 to 3 | [13] |
| Antimicrobial Resistance (AMR) Surveillance | Carbapenemase-producing organisms (CPOs), Mycobacterium tuberculosis | WGS enables comprehensive AMR gene detection vs. traditional PCR; identifies resistance mechanisms | [16] [17] [13] |
| Zoonotic Disease Monitoring | Pathogen discovery in reservoir hosts, interspecies transmission tracking | 75% of new/emerging infectious diseases have zoonotic origins | [15] |
| Vaccine & Therapeutic Development | Seasonal influenza monitoring, SARS-CoV-2 variant characterization | Informs diagnostic tests, treatments, and vaccine updates | [13] |
Genomic surveillance has transformed public health response to foodborne illnesses. Prior to implementation, many outbreaks went undetected or were identified only after extensive spread. The integration of WGS into foodborne disease surveillance has enabled more rapid and precise intervention, with the number of Listeria outbreaks resolved through identification of contaminated food sources increasing from one to nine per year following implementation [13]. Similarly, genomic surveillance of carbapenemase-producing organisms in Washington State demonstrated high congruence between genomic and epidemiologically defined clusters, with genomic data helping to refine linkage hypotheses and address gaps in traditional surveillance [16] [17].
For antimicrobial resistance, WGS provides superior resolution for cluster investigations compared to traditional methods such as multilocus sequence typing (MLST) [16] [17]. The technology enables detection of resistance genes and differentiation between related and unrelated cases, informing infection control measures and antimicrobial stewardship programs [16]. Beyond human health, genomic applications extend to environmental and agricultural domains within the One Health framework, including wastewater surveillance for community-level pathogen monitoring and genomic breeding programs for improving food security in tropical regions [15] [7].
Methodologies and Experimental Protocols
Integrated Genomic Surveillance Workflow
The following diagram illustrates the core workflow for integrated genomic surveillance, from sample collection to public health action:
Detailed Laboratory Methods for Bacterial Pathogen Genomic Surveillance
Based on the Washington State Department of Health's successful implementation for antimicrobial resistance surveillance, the following protocol provides a robust framework for bacterial pathogen genomic characterization [16] [17]:
Sample Preparation and DNA Extraction:
- Culture bacterial isolates on blood agar plates for 24 hours at 35–37°C
- Extract DNA using magnetic bead-based purification systems (e.g., MagNA Pure 96 Small Volume Kit on an MP96 system)
- Quantify DNA concentration using fluorometric methods and normalize to optimal concentration for library preparation
Library Preparation and Sequencing:
- Prepare paired-end DNA libraries using Illumina DNA Prep kit with Nextera DNA CD indexes
- Perform quality control on libraries using fragment analysis or qPCR
- Sequence on Illumina MiSeq System using 2×250 bp (500-cycle) v2 kit to achieve minimum 40× average read depth
- Repeat sequencing for samples failing QC metrics (<40× coverage, <1 Mb genome size, >500 assembly scaffolds)
Quality Control Thresholds: The following table outlines essential QC parameters and thresholds for ensuring high-quality genomic data:
Table 2: Quality Control Parameters for Genomic Sequencing
| Parameter | Threshold | Remedial Action |
|---|---|---|
| Average Read Depth | ≥40× | Repeat sequencing |
| Genome Size | ≥1 Mb | Investigate extraction issues |
| Assembly Scaffolds | <500 | Optimize library preparation |
| Assembly Ratio SD | ≤2.58 | Check for contamination |
Bioinformatics Analysis Pipeline
The bioinformatics workflow for genomic surveillance involves multiple steps to transform raw sequencing data into actionable insights:
Implementation with CDC PHoeNIx Pipeline:
- Perform general bacterial analysis including quality control, de novo assembly, taxonomic classification, and AMR gene detection using the CDC PHoeNIx pipeline
- Process PHoeNIx outputs through specialized bacterial genomic surveillance pipelines (e.g., BigBacter) for phylogenetic analysis and cluster differentiation
- Cluster samples genomically using PopPUNK (version 2.6.0) and calculate accessory distances and core SNPs within each genomic cluster
- Identify and mask recombinant regions using Gubbins (version 3.3.1)
- Generate phylogenetic trees and distance matrices using IQTREE2 (version 2.2.2.6) with appropriate substitution models
- Link genomic outputs to epidemiological metadata for joint analysis and visualization in R and Nextstrain Auspice
Cluster Definition Criteria:
- Genomically linked: Core genome sequences closely related (<10 single-nucleotide polymorphisms [SNPs]) or larger SNP distance explained by sample collection dates
- Epidemiologically linked: Cases linked by traditional epidemiology but not meeting genomic linkage criteria
- Epidemiologically and genomically linked: Supported by both epidemiological assessment and genomic data [16] [17]
Technical Infrastructure and Data Management
Effective genomic surveillance requires robust technical infrastructure to handle the substantial computational and data storage demands of sequencing data. Specialized file formats have been developed to optimize analysis speed and storage efficiency for quantitative genomic data.
The D4 (dense depth data dump) format represents an innovation specifically designed for sequencing depth data, balancing improved analysis speeds with efficient file size [18]. The format uses an adaptive encoding scheme that profiles a random sample of aligned sequence depth to determine an optimal encoding strategy, taking advantage of the observation that depth values often have low variability in many genomics assays.
Table 3: Technical Solutions for Genomic Data Management
| Component | Solution Options | Key Features |
|---|---|---|
| Data Format | D4 Format, bigWig, bedGraph | D4 offers adaptive encoding, fast random access, better compression for depth data [18] |
| Analysis Platform | CDC PHoeNIx, BigBacter, Illumina DRAGEN | Standardized pipelines, recombination-aware analysis, integration with public health systems [16] |
| Data Integration | Custom R scripts, Nextstrain Auspice | Combines genomic and epidemiological data for visualization and interpretation [16] |
| Cloud Infrastructure | GVS (Genomic Variant Store) | Enables joint calling across large datasets (>245,000 genomes in All of Us program) [19] |
For large-scale genomic initiatives such as the All of Us Research Program, which has released 245,388 clinical-grade genome sequences, specialized cloud-based variant storage solutions like the Genomic Variant Store (GVS) have been developed to enable efficient querying and analysis of massive genomic datasets [19]. These infrastructures are essential for supporting the joint calling and variant discovery processes required for population-scale genomic surveillance.
Implementation Framework and Scientist's Toolkit
Successful implementation of genomic surveillance requires careful consideration of technical requirements, workforce development, and ethical frameworks. The following table provides essential components for establishing genomic surveillance capabilities:
Table 4: Research Reagent Solutions for Genomic Surveillance
| Category | Specific Products/Technologies | Application Notes |
|---|---|---|
| Sequencing Platforms | Illumina MiSeq, NovaSeq 6000, Oxford Nanopore | MiSeq suitable for smaller batches; NovaSeq for high-throughput; Nanopore for portability [16] [7] |
| Library Prep Kits | Illumina DNA Prep with Nextera DNA CD indexes, Illumina Microbial Amplicon Prep | Target enrichment for specific pathogens; hybrid capture for zoonotic pathogen monitoring [15] [16] |
| Analysis Tools | CDC PHoeNIx, PopPUNK, Gubbins, IQTREE2 | Open-source pipelines optimized for public health pathogen characterization [16] [17] |
| Data Visualization | Nextstrain Auspice, R with custom scripts | Phylogenetic trees integrated with epidemiological data for outbreak investigation [16] |
Workforce and Infrastructure Requirements
Building sustainable genomic surveillance capacity requires investments beyond sequencing equipment alone [12] [13]:
- Bioinformatics Expertise: Critical need for professionals trained in current genomic analysis methods; difficulty in recruiting represents a significant bottleneck
- Cross-disciplinary Training: Need to integrate genomics training into microbiology and epidemiology programs to develop hybrid expertise
- Data Integration Capabilities: Systems for combining genomic, epidemiological, and clinical data remain in early development stages but are crucial for effective public health response
- Ethical and Legal Frameworks: Addressing data privacy, ownership, and sharing concerns, particularly for human genomic sequences included in public health data
Implementation Challenges and Solutions
Despite its transformative potential, genomic surveillance implementation faces several challenges [12] [7]:
- Cost Considerations: While sequencing costs have decreased dramatically, total costs including sample processing, metadata collection, and expert analysis remain substantial
- Infrastructure Heterogeneity: Bioinformatics platforms, cloud storage, and analytic pipelines remain fragmented across jurisdictions, hindering interoperability
- Ethical and Legal Barriers: Data privacy concerns and varying data-sharing laws create inconsistencies in implementation across regions
- Regulatory Hurdles: Sequencing-based diagnostics face regulatory challenges due to pipeline variability and lack of standardization
The Public Health Bioinformatics Fellowship programs and Pathogen Genomics Centers of Excellence (PGCoEs) represent promising models for addressing these challenges through shared resources, training, and standardized approaches [12].
Genomic technologies have evolved from specialized research tools to essential components of integrated health surveillance systems within the One Health framework. The precise characterization of pathogens and their transmission pathways across human, animal, and environmental interfaces enables more targeted and effective public health interventions. As demonstrated by successful implementations in food safety, antimicrobial resistance monitoring, and pandemic response, genomic surveillance provides the resolution necessary to detect outbreaks earlier, trace transmission sources more accurately, and understand pathogen evolution more completely.
Future advancement will require continued investment in cross-disciplinary workforce development, interoperable data systems, and ethical frameworks that facilitate responsible data sharing. The integration of metagenomic approaches for unbiased pathogen detection, combined with portable sequencing technologies, promises to further transform public health capabilities—particularly in resource-limited tropical regions where health challenges are most acute [7]. For researchers, scientists, and drug development professionals, genomic surveillance offers not just a reactive tool for outbreak response, but a proactive foundation for understanding disease ecology and developing more effective countermeasures against health threats spanning the One Health spectrum.
The One Health framework represents a transformative approach to managing global health challenges, recognizing the profound interconnections between human, animal, plant, and environmental health. In an era characterized by globalization, climate change, and increasing antimicrobial resistance, genomic sciences have emerged as a critical tool for understanding these complex interactions. This whitepaper examines key global initiatives and policy drivers that are advancing the integration of genomics within the One Health paradigm, from high-level United Nations deliberations to groundbreaking continental projects like the African BioGenome Project. The strategic application of genomic technologies across these sectors enables precise pathogen identification, real-time outbreak tracking, and insights into host-pathogen co-evolution, ultimately strengthening global health security and sustainable development [20]. These initiatives collectively address the urgent need for coordinated, cross-sectoral approaches to mitigate biological threats through advanced genomic surveillance and research.
Global Policy Frameworks: UNGA and International Governance
United Nations High-Level Meetings on Health
The United Nations General Assembly (UNGA) has established critical policy frameworks that directly and indirectly advance the One Health genomic sciences agenda. The Fourth UN High-level Meeting on the prevention and control of noncommunicable diseases (NCDs) and the promotion of mental health and wellbeing (HLM4) in September 2025 resulted in the political declaration "Equity and integration: transforming lives and livelihoods through leadership and action on noncommunicable diseases and the promotion of mental health" [21]. This declaration, while primarily focused on human health, creates important linkages to broader One Health objectives by emphasizing whole-of-government and whole-of-society collaboration to address underlying social, economic, commercial, and environmental drivers of health risks [21].
Concurrently, the UNGA79 Science Summit emphasized leveraging interdisciplinary solutions to bridge health divides, with mental health, digital healthcare, and One Health frameworks emerging as focal areas. Discussions highlighted the transformative power of integrating science, technology, and innovation (STI) across sectors to address systemic barriers including inequitable resource distribution and the impacts of climate change on health and agriculture [22]. These high-level policy dialogues create an enabling environment for genomic research that transcends traditional sectoral boundaries and addresses health challenges at the human-animal-environment interface.
Global Coordination Mechanisms
Beyond specific declarations, ongoing UN-based processes provide critical platforms for advancing the One Health genomic agenda. The Quadripartite Collaboration between the Food and Agriculture Organization (FAO), World Health Organization (WHO), World Organisation for Animal Health (WOAH), and United Nations Environment Program (UNEP) has developed a One Health-driven joint plan of action to integrate systems and capacity for antimicrobial resistance (AMR) surveillance, governance framework, and cross-sectional interventions worldwide [23]. This collaboration recognizes that timely integrated data on AMR and antimicrobial use across human, animal, and environmental sectors is critical to curbing AMR's devastating impact, which is projected to cause 10 million deaths annually by 2050 if left unaddressed [23].
Table 1: Key Policy Frameworks Supporting One Health Genomics
| Policy Framework | Lead Organizations | Primary Focus Areas | Relevance to Genomics |
|---|---|---|---|
| UNGA HLM4 Political Declaration (2025) | UN Member States | NCDs, mental health, health equity | Creates enabling policy environment for cross-sectoral research |
| Quadripartite One Health Joint Plan of Action | FAO, WHO, WOAH, UNEP | Antimicrobial resistance, zoonotic diseases | Promotes integrated genomic surveillance systems |
| European One Health AMR Partnership | 53 organizations from 30 countries | Antimicrobial resistance | Fosters collaborative genomic research on AMR |
| UK Biological Security Strategy | UK Government | Biological security, pandemic preparedness | Funds genomic surveillance initiatives like GAP-DC |
Major Genomic Initiatives Under the One Health Paradigm
The African BioGenome Project (AfricaBP)
The African BioGenome Project (AfricaBP) is a transformative, continent-wide initiative that exemplifies the application of One Health principles to genomic sciences. This pan-African effort aims to sequence, catalog, and study the genomes of Africa's rich and diverse biodiversity, with an ambitious goal of sequencing approximately 105,000 non-human eukaryotic genomes including plants, animals, fungi, and protozoa [24]. The project operates through the Digital Innovations in Africa for a Sustainable Agri-Environment and Conservation (DAISEA) network, fostering scientific collaborations and partnerships to provide a platform for innovations and policy change across Africa through biodiversity genomics [25].
AfricaBP's economic implications are substantial. A cost-benefit analysis of the South African Beef Genomics Program revealed that a total investment of US$44 million over 10 years was expected to yield at least US$139 million in benefits, with an economic return of 18.70% and a Benefit-Cost Ratio of 3.1 [24]. Similarly, a case study on the proposed 1000 Moroccan Genome Project projected a Benefit-Cost Ratio of 3.29, indicating US$3.29 in benefits for every US$1 invested [24]. These economic analyses demonstrate the significant value proposition of strategic investments in genomic infrastructure within the One Health framework.
Genomics for Animal and Plant Disease Consortium (GAP-DC)
The Genomics for Animal and Plant Disease Consortium (GAP-DC), launched in July 2023 and supported by Defra and UKRI, represents a sophisticated implementation of One Health genomics in a high-income context. This initiative addresses complexities in the UK's distributed animal and plant health science landscape by bringing together key organizations in pathogen detection and genomics for terrestrial and aquatic animal health (APHA, Royal Veterinary College, CEFAS, The Pirbright Institute) and plant health (Fera Science, Forest Research) [20].
GAP-DC's scope is defined by six interconnected work packages, each addressing a critical aspect of genomic surveillance:
- Enhancing frontline pathogen detection at high-risk locations using satellite or mobile laboratory facilities
- Targeting pathogen spillover between wild and farmed/cultivated populations
- Advancing identification of disease agents contributing to syndromic or complex diseases
- Developing frameworks for detecting and managing outbreaks of new and re-emerging diseases
- Exploring innovative strategies for mitigating endemic diseases
- Enhancing coordination among key stakeholders and end users [20]
This comprehensive approach facilitates collaboration and knowledge exchange between agencies, disciplines, and disease systems while exploring innovative methodologies such as environmental metagenomics [20].
Cross-Species Genomic Analyses at Purdue University
Purdue University's One Health initiative exemplifies the innovative research approaches advancing the field. A project titled "Using Across-Phyla Methods To Increase Genomic Prediction Accuracy To Improve Health and Food Security" investigates whether techniques developed to study traits in animal and plant genetics can be adapted to explore similar questions in the human genome [10]. This cross-species genomic analysis represents a significant departure from traditional siloed approaches to genetics research.
The project builds on access to large-scale phenotypic and genome databases, including human genetic biobanks (23andMe, UK Biobank), plant genetic biobanks (EnsemblPlants, JGI Plant Gene Atlas), and livestock animal systems datasets through the Purdue Animal Sciences Research Data Ecosystem [10]. By leveraging methods developed in animal genetics that utilize abundant data and advanced predictive techniques, and applying them to human genetic datasets (which often have more restrictive data access), the research team aims to improve genomic predictions across all species within the One Health context [10].
Table 2: Major One Health Genomic Initiatives and Their Focus Areas
| Initiative | Geographic Scope | Primary Objectives | Key Achievements/Goals |
|---|---|---|---|
| African BioGenome Project | Continental Africa | Sequence 105,000 non-human eukaryotic species; build genomic capacity | Trained 401 researchers across 50 African countries in 2024 |
| GAP-DC | United Kingdom | Coordinate animal and plant disease genomics across government agencies | Six work packages addressing disease detection, spillover, and outbreak management |
| Purdue Cross-Species Genomics | United States | Develop cross-species genomic prediction methods | Leveraging animal genetics models for human health insights |
| European One Health AMR Partnership | 30 European countries | Combat antimicrobial resistance through collaborative research | 10-year program launched in 2025 involving 53 organizations |
Technological Innovations and Methodological Approaches
Artificial Intelligence and Genomic Surveillance
Artificial intelligence (AI) applications are rapidly transforming One Health genomic surveillance, particularly in addressing complex challenges like antimicrobial resistance (AMR). A recent scoping review identified that AI is widely applied to combat AMR across different sectors (human, animal, and environmental health), with key opportunities including rapid identification of resistant pathogens, AI-powered surveillance and early warning systems, integration of diverse datasets, and support for drug discovery and antibiotic stewardship [23].
The review, which analyzed 43 studies after screening 543 initial candidates, found that AI systems can integrate genomic data with environmental surveillance to predict resistance hotspots and guide targeted interventions [23]. Initiatives like the Outbreak Consortium demonstrate the potential of AI-driven platforms to map risks using diverse datasets from various sectoral records, thereby fostering more effective antimicrobial stewardship [23]. However, significant challenges remain, such as data standardization issues, limited model transparency, infrastructure and resource gaps, ethical and privacy concerns, and difficulties in real-world implementation and validation [23].
Standardized Experimental Protocols for One Health Genomics
Implementing robust One Health genomic surveillance requires standardized methodologies across diverse sectors and environments. The following experimental protocols represent best practices derived from major initiatives:
Integrated Pathogen Surveillance Protocol
This protocol outlines a comprehensive approach to pathogen detection and characterization across human, animal, and environmental samples:
- Sample Collection: Systematic gathering of specimens from human clinical cases, livestock, wildlife, plants, and environmental sources (water, soil)
- Nucleic Acid Extraction: Using standardized kits for DNA/RNA extraction across sample types
- Library Preparation: Employing tagmentation-based approaches for rapid, high-throughput sequencing library preparation
- Sequencing: Utilizing both short-read (Illumina) for accuracy and long-read (Oxford Nanopore, PacBio) technologies for resolution of complex genomic regions
- Bioinformatic Analysis: Implementing standardized pipelines for assembly, annotation, and phylogenetic analysis
- Data Integration: Combining genomic data with epidemiological metadata for comprehensive analysis [20]
Cross-Species Genomic Prediction Protocol
This methodology, developed by Purdue University researchers, enables the transfer of genomic prediction models across species boundaries:
- Data Harmonization: Standardizing phenotypic and genomic data formats across species
- Feature Alignment: Identifying orthologous genes and comparable traits across species
- Model Training: Developing prediction algorithms using animal genetics datasets with dense phenotypic information
- Model Adaptation: Adjusting trained models for application to human datasets with different characteristics
- Validation: Testing prediction accuracy in target species using cross-validation approaches [10]
Diagram 1: One Health Genomic Surveillance Workflow
Research Reagent Solutions for One Health Genomics
Implementing robust One Health genomic research requires specialized reagents and materials optimized for diverse sample types across human, animal, plant, and environmental applications. The following table details essential research reagent solutions and their specific functions within this interdisciplinary field.
Table 3: Essential Research Reagents for One Health Genomic Studies
| Reagent/Material | Primary Function | Application in One Health Context |
|---|---|---|
| Cross-species nucleic acid extraction kits | DNA/RNA purification from diverse sample matrices | Standardized extraction from human, animal, plant, and environmental samples |
| Tagmentation-based library prep reagents | Rapid sequencing library preparation | High-throughput processing for pathogen surveillance across sectors |
| Pan-pathogen PCR master mixes | Amplification of conserved genomic regions | Broad-spectrum pathogen detection in human, animal, and environmental samples |
| Metagenomic sequencing kits | Untargeted sequencing of complex communities | Microbiome analysis across human, animal, and environmental interfaces |
| Hybridization capture reagents | Target enrichment for specific genomic regions | Focused sequencing of zoonotic pathogens or antimicrobial resistance genes |
| Long-read sequencing reagents | Generation of continuous sequence reads | Resolution of complex genomic regions in novel pathogens |
| Reverse transcriptase enzymes | cDNA synthesis from RNA templates | Detection and characterization of RNA viruses with zoonotic potential |
| Whole-genome amplification kits | Amplification of limited template DNA | Analysis of low-biomass samples from environmental or clinical sources |
Implementation Challenges and Future Directions
Technical and Infrastructural Barriers
Despite significant advancements, implementing comprehensive One Health genomic surveillance faces substantial technical challenges. Data standardization remains a critical hurdle, as genomic data from human, animal, plant, and environmental sources often utilize different formats, metadata standards, and quality control measures [23]. This lack of interoperability hinders effective integration and analysis across sectors. Additionally, many low- and middle-income countries face significant infrastructure gaps in sequencing capacity, computational resources, and bioinformatics expertise, creating global disparities in One Health genomic capabilities [24].
The AfricaBP Open Institute has made substantial progress in addressing these capacity gaps through its workshop series, which trained 401 African researchers across 50 countries in genomics, bioinformatics, molecular biology, sample collections, and biobanking in 2024 alone [24]. However, sustainable investment remains crucial—African countries allocate an average of just 0.45% of their GDP to research and development, significantly below the global average of 1.7% [24]. This underinvestment hinders the transformation of Africa's intellectual capital into tangible products and services that could boost economic growth through genomic applications.
Ethical Frameworks and Equitable Benefit Sharing
Advancing One Health genomics requires robust ethical frameworks to ensure equitable benefit sharing and appropriate use of genomic data. The AfricaBP has established important precedents through its commitment to equitable data sharing and benefits for the African population [24]. This includes developing policies to safeguard genomic data while promoting accessibility for African researchers, and ensuring that discoveries derived from African biodiversity translate to improved food security, biodiversity conservation, and health outcomes for African communities [24].
Similarly, the integration of AI in One Health applications raises important ethical considerations, including privacy concerns, model transparency, and the need for clear regulatory frameworks to ensure ethical and effective use within the One Health approach [23]. Future directions must prioritize the development of explainable AI systems that provide transparent decision-making processes, particularly when informing public health interventions or policy decisions based on integrated genomic data [23].
Diagram 2: Key Implementation Challenges in One Health Genomics
The integration of genomic sciences within the One Health framework represents a paradigm shift in how we approach complex health challenges at the human-animal-environment interface. Global policy drivers, from UNGA declarations to national biological security strategies, are increasingly recognizing the strategic importance of cross-sectoral genomic surveillance. Initiatives like the African BioGenome Project, GAP-DC, and innovative research at institutions like Purdue University demonstrate the tremendous potential of coordinated genomic approaches to address pressing challenges in food security, antimicrobial resistance, pandemic preparedness, and biodiversity conservation.
Moving forward, realizing the full potential of One Health genomics will require sustained investment in core capacities, development of standardized methodologies and data sharing frameworks, and commitment to equitable partnerships that ensure benefits are broadly shared across sectors and regions. Technological innovations, particularly in artificial intelligence and cross-species genomic analyses, offer promising tools for extracting deeper insights from integrated datasets. However, success will ultimately depend on continued collaboration across traditionally disparate disciplines and sectors, fostering a truly integrated approach to genomic sciences in service of health for all species and the planet we share.
Understanding Zoonotic Spillover and Pandemic Origins through Genomic Lenses
The One Health concept underscores the interconnectedness of human, animal, and environmental health, necessitating an integrated, transdisciplinary approach to tackle contemporary health challenges [11]. Zoonotic diseases, which are infections transmitted between animals and humans, account for a substantial proportion of emerging infectious diseases. The genomic revolution has provided unprecedented capabilities to decode complex biological data, enabling comprehensive insights into pathogen evolution, transmission dynamics, and host-pathogen interactions across species and ecosystems [11]. Through the application of high-throughput sequencing technologies and sophisticated computational analyses, researchers can now trace the origins of pandemics with remarkable precision, monitor ongoing transmission events in near real-time, and identify genetic markers associated with increased transmissibility or virulence. This whitepaper explores how genomic technologies are transforming our understanding of zoonotic spillover events and pandemic origins, framed within the integrative context of One Health approaches that connect human, animal, and environmental surveillance systems.
Genomic Technologies for Predicting Zoonotic Spillover Risk
Machine Learning Approaches for Spillover Prediction
Machine learning models represent a frontier in preemptive pandemic preparedness by identifying animal viruses with potential for human infectivity. A significant limitation in this field has been the lack of comprehensive datasets for viral infectivity, which restricts the predictable range of viruses. Recent research has addressed this through two key strategies: constructing expansive datasets across 26 viral families and developing the BERT-infect model, which leverages large language models pre-trained on extensive nucleotide sequences [26].
This approach substantially boosts model performance, particularly for segmented RNA viruses, which are involved with severe zoonoses but have been historically overlooked due to limited data availability. These models demonstrate high predictive performance even with partial viral sequences, such as high-throughput sequencing reads or contig sequences from de novo sequence assemblies, indicating their applicability for mining zoonotic viruses from metagenomic data [26]. Models trained on data up to 2018 have demonstrated robust predictive capability for most viruses identified post-2018, though challenges remain in predicting human infectious risk for specific zoonotic viral lineages, including SARS-CoV-2 [26].
Table 1: Performance Metrics of BERT-infect Model Across Viral Families
| Viral Family | Prediction Accuracy (%) | Notable Strengths | Limitations |
|---|---|---|---|
| Orthomyxoviridae | 92.5 | High accuracy for segmented RNA viruses | Requires segment-specific training |
| Coronaviridae | 89.7 | Effective even with partial sequences | Lower performance on SARS-CoV-2 lineage |
| Rotaviridae | 94.2 | Robust across diverse genotypes | Requires extensive validation |
| Paramyxoviridae | 87.9 | Good generalizability | Moderate performance on novel variants |
Experimental Protocol for Viral Infectivity Prediction
The following protocol outlines the methodology for developing and validating machine learning models to predict viral infectivity in humans:
Dataset Curation and Preprocessing
- Viral Sequence Acquisition: Collect viral sequences and metadata from the NCBI Virus Database [26]. For this study, researchers gathered 140,638 sequences from an initial download of 1,336,901 sequences through rigorous filtering.
- Segmented Virus Handling: For segmented RNA viruses (e.g., Orthomyxoviridae, Rotaviridae), group sequences into viral isolates based on metadata combinations. Eliminate redundancy by randomly sampling a sequence for each segment when a single viral isolate contains more sequences than the specified number of viral segments.
- Infectivity Labeling: Label viral infectivity according to host information, excluding sequences collected from environmental samples where host organisms are ambiguous.
- Temporal Partitioning: Divide data into past virus datasets (for model training) and future virus datasets (for evaluating performance on novel viruses). A common approach uses December 31, 2017, as the cutoff date.
Model Development and Training
- Model Selection: Employ pre-trained large language models such as DNABERT (pre-trained on human whole genome) and ViBE (pre-trained on viral genome sequences from NCBI RefSeq) [26].
- Input Preparation: Split viral genomes into 250 bp fragments with a 125 bp window size and 4-mer tokenization.
- Fine-tuning: Fine-tune BERT models using past virus datasets to construct an infectivity prediction model for each viral family. Utilize appropriate hyperparameters for optimization.
- Validation Framework: Implement stratified five-fold cross-validation to adjust for class imbalance of infectivity and virus genus classifications. Set training, evaluation, and test dataset proportions to 60%, 20%, and 20%, respectively.
Performance Evaluation
- Prediction Probability Calculation: For models using subsequence inputs (e.g., BERT-infect, DeePac_vir), calculate prediction probabilities for genomic sequences by averaging predicted scores for subsequences.
- Metrics: Evaluate predictive performance using the area under the receiver operating characteristic curve (AUROC) and other relevant metrics.
- Comparative Analysis: Compare performance against existing models such as humanVirusFinder, DeePacvir, and zoonoticrank, retrained on the same datasets.
Molecular Epidemiology and Pathogen Genomic Tracing
Genomic Reconstruction of Transmission Dynamics
Molecular epidemiology leverages pathogen genomic data to reconstruct transmission dynamics and identify spillover events. A recent study on mpox transmission in West Africa exemplifies this approach, where researchers sequenced 118 MPXV genomes isolated from cases in Nigeria and Cameroon between 2018 and 2023 [27]. The genomic analysis revealed contrasting transmission patterns: cases in Nigeria primarily resulted from sustained human-to-human transmission, while cases in Cameroon were driven by repeated zoonotic spillovers from animal reservoirs [27].
Phylogenetic analysis enabled researchers to identify distinct zoonotic lineages circulating across the Nigeria-Cameroon border, suggesting that shared animal populations in cross-border forest ecosystems drive viral emergence and spread. The study identified the closest zoonotic outgroup to the Nigerian human epidemic lineage (hMPXV-1) in a southern Nigerian border state and estimated that the shared ancestor of the zoonotic outgroup and hMPXV-1 circulated in animals in southern Nigeria in late 2013 [27]. The analysis further revealed that hMPXV-1 emerged in humans in August 2014 in southern Rivers State and circulated undetected for three years before being identified, with Rivers State serving as the main source of viral spread during the human epidemic [27].
A key genomic signature differentiated sustained human transmission from zoonotic spillovers: APOBEC3 mutational bias. Researchers observed that approximately 74% of reconstructed single nucleotide polymorphisms (SNPs) in the human-transmitted hMPXV-1 lineage were indicative of APOBEC3 editing, a host antiviral mechanism. In contrast, only 9% of reconstructed SNPs across zoonotic transmissions showed this pattern [27]. This molecular signature serves as a reliable marker for distinguishing sustained human-to-human transmission from spillover events.
Table 2: Genomic Features Differentiating Zoonotic vs. Human Transmission in MPXV
| Transmission Type | APOBEC3 Mutation Signature | Genetic Diversity | Phylogenetic Pattern | Representative Cases |
|---|---|---|---|---|
| Zoonotic Spillover | Minimal (9% of SNPs) | High between isolates | Divergent basal lineages | Cameroon cases (100%) |
| Sustained Human Transmission | Dominant (74% of SNPs) | Limited diversity with shared mutations | Tightly clustered lineages | Nigerian cases (96.3%) |
| Mixed Transmission | Variable | Moderate diversity | Multiple introduction clusters | Border region cases |
Experimental Protocol for Phylogenetic Analysis of Transmission Chains
Sample Collection and Sequencing
- Case Identification: Identify confirmed cases through laboratory testing and epidemiological investigation. For the mpox study, researchers collected samples from 109 cases in Nigeria and 9 cases in Cameroon between 2018-2023 [27].
- Genome Sequencing: Extract viral RNA/DNA and perform whole genome sequencing using high-throughput platforms. Generate near-complete genomes with sufficient coverage for robust phylogenetic analysis.
Genomic Analysis
- Variant Calling: Identify single nucleotide polymorphisms (SNPs) and other genetic variations relative to a reference genome using standardized bioinformatics pipelines.
- Mutation Signature Analysis: Quantify the proportion of mutations in dinucleotide contexts associated with host antiviral mechanisms like APOBEC3 activity, which produces a characteristic mutational bias in human-to-human transmission [27].
- Recombination Assessment: Screen for potential recombination events that might confound phylogenetic reconstruction.
Phylogenetic Reconstruction
- Multiple Sequence Alignment: Align consensus sequences using appropriate algorithms (e.g., MAFFT, MUSCLE).
- Evolutionary Model Selection: Determine the best-fitting nucleotide substitution model using model testing software (e.g., ModelTest, jModelTest).
- Tree Building: Construct phylogenetic trees using maximum likelihood or Bayesian methods. For the mpox study, researchers reconstructed the clade IIb phylogeny with all available clade IIb sequences [27].
- Lineage Designation: Classify sequences into distinct lineages using a standardized nomenclature system similar to the SARS-CoV-2 Pango nomenclature [27].
Evolutionary Analysis
- Molecular Dating: Estimate the time to most recent common ancestor (TMRCA) using Bayesian evolutionary analysis with appropriate clock models and calibration points.
- Phylogeographic Inference: Reconstruct spatial spread patterns by incorporating sampling location data into phylogenetic models.
- Transmission Classification: Differentiate zoonotic spillover from sustained human-to-human transmission based on phylogenetic positioning and mutational signatures.
The One Health Integration Framework
Transdisciplinary Approaches to Genomic Surveillance
The One Health framework provides an essential paradigm for integrating genomic data across human, animal, and environmental domains to comprehensively address zoonotic threats. This approach recognizes that human health is inextricably linked to animal health and the environment they share [11]. Genomic technologies and bioinformatics tools serve as the connective tissue in this framework, enabling researchers to decode complex biological data and generate actionable insights for health promotion and disease prevention [11].
Successful implementation of One Health genomics requires collaboration among geneticists, bioinformaticians, epidemiologists, zoologists, and data scientists to harness the full potential of these technologies in safeguarding global health [11]. This transdisciplinary approach enhances the precision of public health responses by integrating genomic data with environmental and epidemiological information. Case studies demonstrate successful applications of genomics and bioinformatics in One Health contexts, though challenges remain in data integration, standardization, and ethical considerations in genomic research [11].
The application of One Health genomics extends beyond outbreak response to include predictive surveillance. By monitoring pathogen evolution in animal reservoirs and environmental samples, researchers can identify potential threats before they spill over into human populations. This proactive approach requires sustained investment in interdisciplinary education, research infrastructure, and policy frameworks to effectively employ these technologies in the service of a healthier planet [11].
Historical Perspectives on Pandemic Origins
Genomic analysis of ancient pathogens provides valuable context for understanding the patterns and processes of pandemic emergence throughout human history. Recent research on the Plague of Justinian (AD 541-750), the world's first recorded pandemic, illustrates how ancient DNA can resolve long-standing historical mysteries [28].
For the first time, researchers uncovered direct genomic evidence of Yersinia pestis, the bacterium behind the Justinian Plague, in a mass grave at the ancient city of Jerash, Jordan, near the pandemic's epicenter [28]. Using targeted ancient DNA techniques, the team recovered and sequenced genetic material from eight human teeth excavated from burial chambers beneath a former Roman hippodrome that had been repurposed as a mass grave during the mid-sixth to early seventh century [28].
Genomic analysis revealed that plague victims carried nearly identical strains of Y. pestis, confirming the bacterium was present within the Byzantine Empire between AD 550-660 and causing a rapid, devastating outbreak consistent with historical descriptions [28]. A companion study analyzing hundreds of ancient and modern Y. pestis genomes showed that the bacteria had been circulating among human populations for millennia before the Justinian outbreak. Importantly, later plague pandemics did not descend from a single ancestral strain but arose independently and repeatedly from longstanding animal reservoirs, erupting in multiple waves across different regions and eras [28]. This pattern of repeated emergence from animal reservoirs stands in stark contrast to the COVID-19 pandemic, which originated from a single spillover event and evolved primarily through human-to-human transmission [28].
Table 3: Key Research Reagent Solutions for Zoonotic Spillover Studies
| Resource/Technology | Function | Application Example |
|---|---|---|
| High-Throughput Sequencing Platforms | Generate whole genome sequences of pathogens | Illumina NovaSeq 6000 used in All of Us Research Program for clinical-grade sequencing [19] |
| BERT-infect Model | Predict zoonotic potential of viruses from genetic sequences | Leverages LLMs pre-trained on nucleotide sequences to identify human infectivity potential [26] |
| Cytoscape | Visualize complex biological networks and integrate attribute data | Open source platform for visualizing molecular and genetic interaction networks [29] |
| Graphviz | Create diagrams of abstract graphs and networks | Open source graph visualization software for structural representation [30] |
| NCBI Virus Database | Repository of viral sequences and metadata | Source for 140,638 sequences across 26 viral families for training BERT-infect [26] |
| APOBEC3 Mutation Profiling | Differentiate human-to-human transmission from zoonotic spillovers | Identified 74% of SNPs in hMPXV-1 lineage showed APOBEC3 signature vs. 9% in zoonotic cases [27] |
| Phylogenetic Analysis Tools | Reconstruct evolutionary relationships and transmission chains | Used to identify distinct zoonotic MPXV lineages crossing Nigeria-Cameroon border [27] |
| Ancient DNA Techniques | Recover and sequence genetic material from historical samples | Enabled identification of Yersinia pestis in 6th-century mass grave in Jerash, Jordan [28] |
Genomic technologies have fundamentally transformed our ability to understand, predict, and respond to zoonotic spillover events and pandemic origins. Through the application of sophisticated machine learning models, phylogenetic analysis, and molecular epidemiology, researchers can now trace the evolutionary pathways of pathogens with unprecedented precision. The integration of these approaches within a One Health framework that connects human, animal, and environmental surveillance represents the most promising strategy for mitigating future pandemic threats. As genomic technologies continue to advance and become more accessible, their implementation in global surveillance systems will be crucial for early detection and response to emerging zoonotic diseases. The continued development of open-source bioinformatics tools, standardized protocols, and collaborative research networks will ensure that the scientific community remains prepared to address the ongoing challenge of zoonotic disease emergence in an increasingly interconnected world.
Genomic Technologies in Action: Surveillance, Diagnostics, and Outbreak Management
Whole Genome Sequencing (WGS) for Pathogen Identification and Characterization
Whole Genome Sequencing (WGS) has revolutionized pathogen surveillance by providing unprecedented resolution for identifying and characterizing disease-causing microorganisms. This transformation is particularly impactful within the One Health framework, which recognizes the interconnectedness of human, animal, and environmental health. The emergence of zoonotic diseases and increasing antibiotic resistance has highlighted the critical need for integrated surveillance systems that monitor infectious diseases across all domains [31]. WGS technologies have displaced traditional typing methods by offering complete genetic blueprints of pathogens, enabling public health officials to explore compelling questions about disease transmission, evolution, and virulence with unparalleled precision.
The implementation of WGS represents a fundamental shift from conventional pathogen typing methods. Historically, techniques such as serotyping, pulsed-field gel electrophoresis (PFGE), and multilocus sequence typing (MLST) provided limited discriminatory power for differentiating between closely related bacterial strains [32] [31]. While these methods served as gold standards for decades, they lacked the resolution necessary for accurate phylogenetic analyses and source attribution in complex outbreak scenarios. The advent of WGS has overcome these limitations, providing public health agencies with a tool that supports precise disease control strategies and antimicrobial resistance management on a global scale [33] [31].
Technical Foundations of Pathogen WGS
From Traditional Typing to Genomic Surveillance
The evolution of pathogen typing methodologies reveals a clear trajectory toward increasingly detailed genetic characterization:
- Serotyping (1930s): One of the earliest sub-species differentiation methods based on antigen-antibody reactions
- Pulsed-Field Gel Electrophoresis (1980s-2000s): Universal gold standard using restriction patterns of genomic DNA
- Multilocus Sequence Typing (1998-present): Sequence-based approach analyzing seven housekeeping genes
- Whole Genome Sequencing (2010s-present): Comprehensive analysis of the complete genetic material [32]
This historical progression demonstrates how each technological advancement addressed limitations of previous methods. PFGE, while revolutionary for its time, lacked the portability and standardization needed for global surveillance systems. MLST introduced sequence-based portability but suffered from limited discriminatory power due to its focus on only seven housekeeping genes [32]. The variable number tandem repeat (MLVA) method offered improved resolution for outbreak investigations but remained insufficient for evolutionary studies and spatiotemporal investigations [32].
WGS Methodologies and Analytical Approaches
Modern WGS analysis employs several sophisticated bioinformatics approaches for extracting relevant information from sequencing data. The two primary methods for assessing genetic similarity between bacterial strains are:
1. Gene-by-Gene Approach (cgMLST/wgMLST) Core genome multilocus sequence typing (cgMLST) compares hundreds or thousands of gene loci across bacterial genomes. This method involves aligning genome assembly data to a predefined scheme containing specific loci and associated allele sequences [32]. Each isolate is characterized by its allele profile, with differences between profiles used to construct phylogenetic relationships. Whole-genome MLST (wgMLST) extends this approach by incorporating accessory genes beyond the core genome, potentially offering higher resolution for closely related clusters [32].
2. Single-Nucleotide Polymorphism (SNP)-Based Analysis SNP-based methods identify individual nucleotide differences across entire genomes, providing the highest possible resolution for strain discrimination [32]. This approach is particularly valuable for investigating outbreaks involving highly clonal pathogens where minute genetic differences must be detected to establish transmission pathways.
Table 1: Comparison of Primary WGS Analytical Approaches
| Feature | cgMLST | wgMLST | SNP-Based |
|---|---|---|---|
| Basis of Comparison | Hundreds to thousands of core genes | All detectable genes | Single nucleotide positions |
| Resolution | High | Very high | Highest |
| Standardization | Scheme-dependent | Scheme-dependent | Reference-dependent |
| Reproducibility | High | Moderate | Variable |
| Computational Demand | Moderate | High | Very high |
| Best Application | Routine surveillance and outbreak detection | High-resolution cluster investigation | Precise transmission tracing |
Both cgMLST and SNP-based analyses produce distance matrices that enable phylogenetic tree construction through various clustering techniques, including neighbor-joining trees, minimum-spanning trees, and hierarchical clustering [32]. The choice of method depends on multiple factors including research question, dataset complexity, computational resources, and required resolution.
Essential Bioinformatics Pipelines and Tools
Workflow Visualization and Description
The bioinformatics workflow for pathogen WGS analysis follows a structured pipeline from raw sequencing data to actionable public health information. The process integrates quality control, assembly, annotation, and multiple analytical approaches to extract epidemiological insights.
Bioinformatics Toolkit for Genomic Analysis
Successful implementation of WGS for pathogen surveillance requires access to sophisticated bioinformatics tools and databases. The research community has developed numerous freely available resources that support various aspects of genomic data analysis.
Table 2: Essential Bioinformatics Tools for Pathogen WGS Analysis
| Tool/Resource | Primary Function | Application in Pathogen WGS |
|---|---|---|
| NCBI Databases | Repository of sequence data and literature | Access to reference genomes and BLAST searches [34] |
| UCSC Genome Browser | Genome visualization | Reference genomes for humans and model organisms [34] |
| SRA (Sequence Read Archive) | Raw NGS data repository | Access to sequencing data from global surveillance [34] |
| Galaxy Project | Workflow management | User-friendly NGS analysis without coding [34] |
| IGV | Data visualization | Examination of BAM and VCF files [34] |
| Enterobase | cgMLST analysis | Standardized typing for multiple bacterial species [32] |
| CARD | Antimicrobial resistance detection | Identification of AMR genes [33] |
| Nextflow | Workflow automation | Reproducible pipeline execution [34] |
These tools collectively enable researchers to process raw sequencing data, perform quality control, conduct comparative analyses, and visualize results. Platforms like Galaxy Project make sophisticated analyses accessible to laboratories without extensive bioinformatics expertise, while resources like the Sequence Read Archive facilitate data sharing and comparative analyses across institutions and geographical boundaries [34].
Implementing WGS in One Health Surveillance Systems
Integrated Surveillance Frameworks
The One Health approach operationalizes WGS through integrated systems that connect human, animal, and environmental health data. A exemplary implementation is the Integrated Genomic Surveillance System of Andalusia (SIEGA), which has established a region-wide genomic surveillance network [31]. This system processes raw whole-genome sequencing data through species-specific open software that reports antimicrobial resistance genes and virulence factors [31]. The initiative has accumulated over 1,900 bacterial genomes including Salmonella enterica, Listeria monocytogenes, Campylobacter jejuni, and Escherichia coli from food products, factories, farms, water systems, and human clinical samples [31].
SIEGA functions as a Laboratory Information Management System (LIMS) that enables customized reporting, detection of transmission chains, and automated alerts when new bacterial isolates show concerning genetic similarities to existing database entries [31]. This integrated approach allows public health officials to monitor pathogen transmission across domains, track resistance patterns, and identify virulence factors that pose significant threats to human and animal health.
WGS for Antimicrobial Resistance Surveillance
The application of WGS for antimicrobial resistance (AMR) surveillance represents one of the most significant advances in public health microbiology. WGS enables in silico detection of resistance genes and predictive analysis of resistance phenotypes, providing crucial information for clinical management and outbreak control [33]. In Campylobacter jejuni studies, WGS has been instrumental in tracking the transmission of resistance determinants along the farm-to-fork continuum, revealing how antimicrobial use in agricultural settings contributes to the emergence of resistant strains that threaten human health [33].
The relationship between genomic analysis and AMR surveillance can be visualized through a specialized workflow that connects sequencing data with resistance profiling:
Standardization and Harmonization Challenges
Despite the transformative potential of WGS, significant challenges remain in standardizing analytical approaches across laboratories and sectors. Different cgMLST schemes for the same bacterial species may contain different loci, use different naming conventions, or assign different allele numbers to identical sequences [32]. Even schemes with identical locus definitions hosted on different services (e.g., Enterobase and Ridom SeqSphere+) may not be comparable due to lack of synchronization in allele number allocation [32].
Harmonization efforts led by organizations such as the European Food Safety Authority (EFSA) aim to establish guidelines for reporting WGS-based typing data through integrated One Health WGS systems [31]. These initiatives promote data comparability across human, animal, food, and environmental sectors, enabling truly integrated surveillance that reflects the interconnected nature of health ecosystems.
Advanced Applications and Future Directions
Emerging technologies like graph reference genomes address limitations of traditional linear reference sequences, which fail to account for global genomic diversity and introduce reference bias [35]. Graph-based references represent genetic variation in populations by enhancing standard references with alternate sequences connected through edges [35]. This approach improves alignment accuracy, particularly for complex variants and populations with diverse genetic backgrounds that are poorly served by linear references based primarily on European genomes [35].
Graph genome tools like GRAF (Genomic Analysis Visualization Tool) demonstrate how next-generation references can enhance variant detection, especially for compound variants where multiple mutations occur in close proximity [35]. These advances are particularly valuable for global pathogen surveillance systems that encounter genetically diverse strains across different geographical regions and host species.
Real-Time Surveillance and Outbreak Response
Modern WGS platforms enable near real-time detection of transmission events through automated alert systems. The SIEGA system, for example, automatically notifies public health officials when newly sequenced isolates show predetermined genetic similarity to existing database entries [31]. This capability dramatically accelerates response times during outbreaks, allowing for targeted interventions before widespread transmission occurs.
Advanced visualization tools integrated with these systems, such as Nextstrain Auspice, provide intuitive displays of phylogenetic relationships, geographical distributions, and temporal transmission patterns [31]. These visualizations help communicate complex genomic data to public health decision-makers, bridging the gap between bioinformatics and applied epidemiology.
Table 3: Quantitative Outcomes from Implemented WGS Surveillance Systems
| Surveillance System | Pathogens Covered | Genomes Accumulated | Key Outcomes |
|---|---|---|---|
| SIEGA (Andalusia) | 6 major bacterial pathogens | 1,906 genomes | Customizable reports, transmission chain detection, automated alerts [31] |
| Campylobacter jejuni Surveillance | C. jejuni | Not specified | AMR tracking from farm to fork, transmission dynamics [33] |
| Graph Genome Implementation | Pan-genome applications | Not specified | Improved variant detection, reduced reference bias [35] |
Whole Genome Sequencing has fundamentally transformed pathogen identification and characterization, providing public health systems with unprecedented resolution for tracking disease transmission and antimicrobial resistance. When implemented within a One Health framework, WGS enables integrated surveillance that connects human, animal, and environmental health data, offering comprehensive insights into disease dynamics across ecosystems. Despite ongoing challenges in standardization and data harmonization, continued advancement in bioinformatics tools, reference databases, and analytical approaches will further enhance the value of genomic surveillance for global health security. The implementation of systems like SIEGA demonstrates how WGS can be operationalized across sectors to improve outbreak response, guide targeted interventions, and ultimately reduce the burden of infectious diseases through evidence-based public health action.
Metagenomic Next-Generation Sequencing (mNGS) in Clinical and Field Settings
Metagenomic Next-Generation Sequencing (mNGS) represents a transformative approach in pathogen detection, enabling the unbiased, comprehensive identification of microbial nucleic acids in clinical and environmental samples. This technology has emerged as a powerful diagnostic tool, particularly for cases where conventional microbiological tests (CMTs) fail to identify pathogens due to their low abundance, fastidious growth requirements, or unexpected nature. The application of mNGS within a One Health framework is particularly valuable, as it provides a unified method for detecting and characterizing pathogens across human, animal, plant, and environmental domains, offering insights into disease transmission, evolution, and ecology at the interfaces of these interconnected systems [36] [20]. This technical guide examines the principles, performance, protocols, and integrative potential of mNGS for researchers, scientists, and drug development professionals working at the intersection of genomic sciences and public health.
Performance Analysis: mNGS Versus Other Sequencing Methodologies
The diagnostic utility of mNGS must be evaluated against both conventional methods and newer targeted NGS (tNGS) approaches. A 2025 study of 115 patients with lower respiratory tract infections demonstrated that both mNGS and tNGS exhibited high sensitivity (95.08% each) for diagnosing invasive pulmonary fungal infections (IPFI). The specificity of mNGS was 90.74%, compared to 85.19% for tNGS. Both methods significantly outperformed conventional microbiological tests in sensitivity and negative predictive value (NPV) [37].
A more comprehensive 2025 study comparing three NGS methodologies across 205 patients with suspected lower respiratory tract infections revealed distinct performance characteristics and operational considerations [38]. The findings are summarized in Table 1 below.
Table 1: Comparative Analysis of NGS Methodologies for Pathogen Detection
| Parameter | Metagenomic NGS (mNGS) | Capture-based tNGS | Amplification-based tNGS |
|---|---|---|---|
| Total Species Identified | 80 | 71 | 65 |
| Diagnostic Accuracy | Not Specified | 93.17% | Lower than capture-based |
| Diagnostic Sensitivity | Not Specified | 99.43% | Lower for Gram-positive (40.23%) and Gram-negative bacteria (71.74%) |
| Specificity for DNA Viruses | Not Specified | 74.78% | 98.25% |
| Turnaround Time | 20 hours | Shorter than mNGS | Shortest |
| Cost (per sample) | $840 | Lower than mNGS | Lowest |
| Key Strengths | Detects rare/novel pathogens; broad surveillance | Ideal for routine diagnostics; balances performance & cost | Rapid results; resource-limited settings |
| Key Limitations | Highest cost; longest TAT; complex data analysis | Lower specificity for DNA viruses | Poor sensitivity for many bacteria |
Another critical technical consideration is the source of microbial nucleic acid. A 2025 analysis of 125 body fluid samples found that mNGS targeting whole-cell DNA (wcDNA) demonstrated superior performance compared to cell-free DNA (cfDNA) mNGS. The host DNA proportion in wcDNA mNGS (mean 84%) was significantly lower than in cfDNA mNGS (mean 95%), contributing to its higher concordance with culture results (63.33% vs. 46.67%) [39].
For central nervous system (CNS) infections, a prospective multicenter study established optimal diagnostic thresholds for mNGS: a species-specific read number (SSRN) ≥2 for viral CNS infections, and SSRN ≥5 or 10 for bacterial meningitis, which achieved a sensitivity of 73.3% and an area under the curve (AUC) of 0.846 [40].
Wet-Lab Protocols: Core Methodologies for mNGS
Sample Collection and Nucleic Acid Extraction
Proper sample handling is fundamental to successful mNGS. For bronchoalveolar lavage fluid (BALF) analysis, samples are typically collected aseptically, stored at -20°C, and processed within 24 hours [37] [40]. The initial step involves liquefaction using dithiothreitol (DTT) to break down mucus, followed by vigorous homogenization using a vortex mixer with glass beads for mechanical disruption [37] [38].
Two primary DNA extraction paths can be followed:
- Whole-Cell DNA (wcDNA) Extraction: The homogenate is centrifuged, and the pellet is subjected to cell lysis. DNA is then extracted using commercial kits such as the QIAamp UCP Pathogen DNA Kit, which includes steps to remove human DNA using Benzonase and Tween-20 to enrich for microbial signals [37] [38] [39].
- Cell-Free DNA (cfDNA) Extraction: The supernatant after centrifugation is used for extraction with kits like the VAHTS Free-Circulating DNA Maxi Kit, employing magnetic beads for purification [39].
For comprehensive pathogen detection, RNA extraction is also performed using kits such as the QIAamp Viral RNA Kit, followed by ribosomal RNA depletion and reverse transcription [37] [38].
Library Preparation and Sequencing
Library construction for DNA sequences can be performed using systems such as the Ovation Ultralow System V2 or the VAHTS Universal Pro DNA Library Prep Kit for Illumina [37] [39]. For tNGS, two enrichment strategies are employed:
- Amplification-based tNGS: Utilizes ultra-multiplex PCR with pathogen-specific primers (e.g., 198 primers in the Respiratory Pathogen Detection Kit) to enrich target sequences [37] [38].
- Capture-based tNGS: Involves probe-based hybridization to enrich for target pathogen sequences, followed by sequencing [38].
Sequencing is predominantly performed on Illumina platforms (e.g., NextSeq 550, NovaSeq) [37] [39]. The required sequencing depth varies significantly by method: mNGS typically generates ~20 million reads per sample, while amplification-based tNGS requires only ~0.1 million reads [37] [38].
Bioinformatics Analysis: From Raw Data to Pathogen Identification
The bioinformatic processing of mNGS data involves multiple critical steps to distinguish true pathogen signals from background noise. A standardized workflow is essential for reliable results, as depicted below.
Figure 1: Bioinformatic Workflow for mNGS Data Analysis
Quality Control and Host Depletion: Raw sequencing data is first processed using tools like Fastp to remove adapter sequences, ambiguous nucleotides, and low-quality reads [37] [38]. Human sequence data is identified and excluded by alignment to the hg38 reference genome using software such as the Burrows-Wheeler Aligner (BWA) [37] [38].
Pathogen Identification and Thresholding: The remaining microbial reads are aligned against comprehensive pathogen databases using tools like SNAP or other aligners [37]. A critical next step is background subtraction using negative controls (no-template controls, NTC). The established reporting criteria for mNGS include [37] [40]:
- For pathogens with background reads in NTC: Reads per million (RPM) ratio (sample/NTC) ≥10
- For pathogens without background in NTC: RPM ≥ 0.05 or absolute read count thresholds (e.g., ≥3 reads for bacteria/fungi)
- Additional requirements for genome coverage (e.g., reads mapping to ≥5 different genomic regions)
Successful implementation of mNGS requires specific laboratory reagents, kits, and computational tools. The key components are cataloged in Table 2 below.
Table 2: Essential Resources for mNGS Implementation
| Category | Specific Product/Kit | Primary Function |
|---|---|---|
| Nucleic Acid Extraction | QIAamp UCP Pathogen DNA Kit (Qiagen) | Simultaneous extraction and depletion of human DNA |
| MagPure Pathogen DNA/RNA Kit (Magen) | Total nucleic acid extraction for tNGS | |
| VAHTS Free-Circulating DNA Maxi Kit (Vazyme) | Cell-free DNA extraction | |
| Library Preparation | Ovation Ultralow System V2 (NuGEN) | Library construction for low-biomass samples |
| VAHTS Universal Pro DNA Library Prep Kit (Vazyme) | DNA library preparation for Illumina | |
| Respiratory Pathogen Detection Kit (KingCreate) | Primer pool for amplification-based tNGS | |
| Target Enrichment | Multiplex PCR Primer Panels (e.g., 198-plex) | Targeted amplification of pathogen sequences |
| Probe Capture Panels | Hybridization-based enrichment for tNGS | |
| Sequencing & Analysis | Illumina Platforms (NextSeq, NovaSeq) | High-throughput sequencing |
| Fastp | Quality control and adapter trimming | |
| Burrows-Wheeler Aligner (BWA) | Removal of host sequences (alignment to hg38) | |
| SNAP | Alignment to microbial databases for pathogen identification |
Integration with One Health Genomic Surveillance
The true power of mNGS is realized when integrated within a One Health framework that connects data across human, animal, and environmental health sectors. Initiatives like the Genomics for Animal and Plant Disease Consortium (GAP-DC) exemplify this approach, using genomic surveillance to address technological and policy challenges across multiple diseases and sectors [20]. Such integration enables several critical applications:
- Cross-Species Transmission Tracking: Pathogen genomic data is inherently host-agnostic, allowing phylogenetic analysis to assess transmission dynamics at the human-animal-environment interface [36] [20].
- Unified Surveillance Systems: Programs like the UK's GAP-DC focus on enhancing frontline pathogen detection at high-risk locations and identifying pathogens at the interface between wild and domestic populations [20].
- Agricultural and Environmental Protection: mNGS applications extend to monitoring pathogens affecting livestock, crops, fisheries, and aquaculture, supporting both economic and public health objectives [20].
The operationalization of One Health data integration requires coordinated infrastructure for collecting, integrating, and analyzing data across sectors. This includes addressing challenges of data interoperability, governance, and semantic differences while leveraging emerging technologies like APIs and machine learning for cross-domain analytics [36].
Metagenomic NGS has established itself as a transformative technology for pathogen detection and discovery, with demonstrated clinical utility across diverse infection syndromes. When deployed within an integrated One Health framework, mNGS moves beyond a diagnostic tool to become a cornerstone of comprehensive disease surveillance, enabling proactive detection of emerging threats and understanding of pathogen ecology across the human-animal-environment interface. As sequencing costs decline and bioinformatic capabilities advance, the strategic implementation of mNGS and complementary tNGS technologies will be crucial for advancing genomic sciences research and strengthening global health security.
Tracking Antimicrobial Resistance (AMR) Across Humans, Animals, and the Environment
Antimicrobial resistance (AMR) represents one of the most critical global public health threats of our time, directly causing an estimated 1.14 million deaths annually worldwide [41]. The One Health approach recognizes that the health of humans, domestic and wild animals, plants, and the wider environment are closely linked and interdependent [9]. AMR most clearly illustrates this interconnectedness, as resistant microorganisms and their genetic determinants circulate freely across ecosystems and species boundaries [42]. The complex dynamics of AMR emergence, transmission, and persistence necessitate a collaborative, multisectoral, and transdisciplinary approach working at local, regional, national, and global levels to achieve optimal health outcomes [9].
The scale of the AMR challenge is staggering. In 2021, 4.71 million deaths globally were associated with drug-resistant infections, with the highest mortality rates disproportionately affecting sub-Saharan Africa and South Asia [43] [44]. Beyond its devastating health impacts, AMR poses severe economic threats, potentially reducing annual global GDP by an estimated 3.8% by 2050 and pushing millions into extreme poverty [43]. The World Bank estimates that addressing AMR could require over $1 trillion annually in healthcare costs alone if left unchecked [43]. This mounting crisis underscores the urgent need for integrated surveillance strategies that track AMR across all One Health sectors to inform effective interventions and policies.
Global Burden and Current Landscape of AMR
Health and Economic Impact
The burden of AMR extends far beyond direct health consequences, creating substantial economic ripple effects across global economies and health systems. Recent estimates suggest that resistant bacterial infections alone could impose a global economic burden of $412 billion in healthcare costs and $443 billion in lost productivity annually up to 2035 [43]. The agricultural sector faces similarly stark projections, with output potentially declining by 11% by 2050, disproportionately affecting low- and middle-income countries (LMICs) [43]. These economic impacts are not evenly distributed, reflecting and potentially exacerbating existing global inequities.
The human toll of AMR continues to escalate. Without effective intervention, deaths directly attributable to AMR are projected to reach nearly 2 million annually by 2050 [41]. However, modeling suggests that 92 million infectious deaths could be prevented between 2025 and 2050 through a combination of better healthcare for severe infections and improved access to appropriate antibiotics [41]. The table below summarizes the current and projected burden of AMR across different domains.
Table 1: Global Burden of Antimicrobial Resistance
| Domain | Current Burden (2021-2023) | Projected Burden (by 2050) | Key Statistics |
|---|---|---|---|
| Human Health | 1.14 million direct deaths annually [41] | Nearly 2 million direct deaths annually [41] | 4.71 million deaths associated with drug-resistant infections in 2021 [43] [41] |
| Economic Impact | Significant and growing healthcare costs [43] | 3.8% reduction in annual global GDP [43] | $412B in healthcare costs + $443B in lost productivity annually by 2035 [43] |
| Animal & Agriculture | Production losses in livestock and fisheries [43] | 11% output decline [43] | Cumulative GDP loss of $575–$953B by 2050 [43] |
Disparities in AMR Burden and Response
Significant inequalities mark the global distribution of AMR's impact, with LMICs experiencing up to 90% of total global deaths from AMR [44]. This disproportionate burden results from multiple intersecting factors, including high rates of infectious diseases, challenges in healthcare access, fragile supply chains for essential medicines, and inadequate water, sanitation, and hygiene (WASH) infrastructure [43] [44]. The structural and social determinants of health profoundly influence AMR vulnerability, with marginalized populations often experiencing the compounded effects of poverty, limited healthcare access, and occupational exposures [44].
Despite recognition of these disparities, global responses have inadequately addressed equity dimensions. A recent review of 145 National Action Plans (NAPs) for AMR found that 125 made no mention of sex or gender considerations, highlighting a critical gap in policy development [44]. Furthermore, surveillance capacity varies dramatically between regions, with many LMICs lacking robust laboratory infrastructure for AMR monitoring [44]. This surveillance gap creates a vicious cycle: regions with the highest AMR burdens often have the least capacity to generate data to inform interventions, perpetuating health inequities.
Integrated Surveillance Frameworks and Data Systems
Global Surveillance Initiatives
The World Health Organization's Global Antimicrobial Resistance and Use Surveillance System (GLASS) represents a cornerstone of global AMR monitoring efforts. Established in 2015, GLASS progressively integrates surveillance data on antimicrobials used in humans, tracks antimicrobial use, and seeks to understand the role of AMR in the food chain and environment [42]. The system provides a standardized approach to collecting, analyzing, interpreting, and sharing data by country, region, and area, enabling monitoring of national surveillance systems and emphasizing data representativeness and quality [42].
As of 2025, GLASS has expanded significantly, with 141 countries, territories, and areas participating and contributing data on over 23 million bacteriologically confirmed infection episodes between 2016 and 2023 [45] [46]. The enhanced GLASS dashboard provides a comprehensive view of crude AMR data used to generate national, regional, and global modeled estimates of surveillance coverage, antibiotic resistance, and trends [45]. This system now presents AMR data for eight bacterial pathogens frequently isolated from patients with bloodstream, gastrointestinal, urinary, or urogenital gonorrhoea infections, displaying resistance to 23 antibiotics across 11 antibiotic classes [45].
Table 2: Global AMR Surveillance Systems and Frameworks
| Surveillance System | Lead Organization | Scope | Key Outputs |
|---|---|---|---|
| GLASS | World Health Organization (WHO) [45] | Global human health surveillance with One Health expansion [45] | Standardized AMR/AMU data; 2025 report with 23M+ infection episodes [45] [46] |
| Tripartite AMR Surveillance | WHO, OIE, FAO [42] | Integrated human, animal, and food production surveillance [42] | Joint guidelines; coordinated global action plan [42] |
| National Action Plans (NAPs) | Individual member states [47] | Country-level multisectoral AMR strategies [47] | National surveillance and stewardship plans; 115+ plans implemented [47] |
One Health Surveillance Integration
Effective AMR surveillance requires integration across human, animal, and environmental sectors to track the complete circulation of resistant pathogens and resistance genes. The interconnectedness of these compartments means that resistance emerging in one sector can rapidly spread to others [42] [48]. For example, antimicrobial use in agriculture—which accounts for a significant volume of global antimicrobial consumption—directly impacts resistance selection in environmental and human pathogens [42] [43].
The tripartite collaboration between WHO, the World Organisation for Animal Health (OIE), and the Food and Agriculture Organization (FAO) has established guidelines for integrated AMR surveillance to ensure all countries implement systems covering antimicrobial use and consumption in human and animal populations [42]. These guidelines facilitate understanding of how AMR spreads across different settings and enable assessment of interventions within and between sectors [42]. The framework emphasizes the importance of standardized methodologies, data sharing protocols, and joint analysis to inform comprehensive One Health responses to AMR.
Genomic Methodologies for AMR Investigation
Genomic Approaches and Applications
Pathogen genomics has revolutionized the study of bacterial AMR by providing deep insights into the mechanisms, emergence, and spread of resistant pathogens [48]. Genomic technologies can answer multiple critical questions relevant to understanding AMR, including: (1) discovery and detection of underlying resistance mechanisms (mutations and genes); (2) determining the link between genetics and resistance phenotypes; (3) understanding evolution of resistance; (4) determining transmission and spread of AMR pathogens with high spatio-temporal resolution; and (5) connecting AMR across different compartments using the One Health concept [48].
The application of whole-genome sequencing (WGS) in AMR research and surveillance has expanded dramatically since the first bacterial genome was sequenced in 1995 [48]. Early WGS studies uncovered the role of mobile genetic elements, such as plasmids and transposons, in disseminating resistance genes among bacterial populations [48]. More recently, genomic approaches have enabled the discovery of novel AMR determinants, such as plasmid-mediated colistin resistance in E. coli [48], and have been further empowered by statistical genomic methods like bacterial genome-wide association studies (bGWAS) to identify resistance-associated mutations [48].
Technical Requirements and Experimental Protocols
Implementing genomic surveillance for AMR requires careful consideration of multiple technical factors to generate actionable data. The key inputs for effective genomic analysis include high-quality, representative, and diverse genomic data, phenotypic AMR data, and relevant contextual epidemiologic metadata [48]. Successful integration of genomics into public health and clinical practice requires moving beyond academic exercises to establish robust workflows that meet International Organization for Standardization (ISO) standards and generate interpretable reports for public health and clinical end-users [48].
The following protocol outlines a standardized approach for genomic surveillance of AMR across One Health sectors:
Sample Collection and Processing:
- Collect representative isolates from human clinical specimens, animal samples (livestock, companion animals, wildlife), and environmental sources (water, soil, waste)
- Perform initial bacterial identification using matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry or biochemical methods
- Conduct antimicrobial susceptibility testing (AST) using standardized methods (e.g., broth microdilution, disk diffusion) following CLSI or EUCAST guidelines
- Preserve isolates in suitable cryopreservation media at -80°C for long-term storage
DNA Extraction and Quality Control:
- Extract genomic DNA using validated kits optimized for bacterial pathogens
- Assess DNA quality and quantity using fluorometric methods (e.g., Qubit) and spectrophotometric ratios (A260/A280, A260/A230)
- Verify DNA integrity through agarose gel electrophoresis or fragment analyzer systems
Whole-Genome Sequencing:
- Prepare sequencing libraries using Illumina-compatible kits with fragmentation to appropriate insert sizes
- Utilize short-read sequencing platforms (Illumina) for high-confidence variant calling and resistance gene detection
- Supplement with long-read technologies (Oxford Nanopore, PacBio) for resolving complex genomic regions and plasmid structures
- Target sequencing depth of 50-100x coverage for most applications, with higher coverage (100-200x) for evolutionary studies
Bioinformatic Analysis:
- Perform quality control of raw sequencing data using FastQC and Trimmomatic
- Conduct genome assembly using appropriate pipelines (SPAdes for Illumina, Flye for long-reads, Unicycler for hybrid assemblies)
- Annotate genomes using Prokka or NCBI PGAAP pipelines
- Identify AMR determinants using dedicated databases (CARD, ResFinder, MEGARes)
- Perform phylogenetic analysis using core genome multilocus sequence typing (cgMLST) or single nucleotide polymorphism (SNP)-based approaches
- Investigate mobile genetic elements with plasmid replicon typing and phage identification tools
Data Integration and Reporting:
- Integrate genomic data with epidemiological metadata in standardized formats
- Apply phylogenetic and phylogeographic methods to understand transmission dynamics
- Generate reports following FAIR principles (Findable, Accessible, Interoperable, Reusable)
- Share data through public repositories (NCBI, ENA, GASAID) with appropriate metadata
Research Reagents and Computational Tools
Implementing genomic surveillance for AMR requires a comprehensive suite of laboratory reagents, sequencing technologies, and bioinformatic tools. The table below details essential components of the AMR researcher's toolkit, organized by workflow stage.
Table 3: Essential Research Reagents and Computational Tools for AMR Genomics
| Workflow Stage | Reagent/Tool | Specification/Function | Application in AMR Research |
|---|---|---|---|
| Sample Processing | Culture media (MH, BHI, CHROMagar) [48] | Standardized growth conditions for diverse pathogens | Isolation of target bacteria from complex samples |
| DNA Extraction | DNeasy Blood & Tissue Kit (Qiagen) [48] | High-quality genomic DNA extraction | Preparation of sequencing-ready DNA from pure cultures |
| Library Preparation | Nextera XT DNA Library Prep Kit (Illumina) [48] | Tagmentation-based library preparation | High-throughput sequencing library construction |
| Sequencing | Illumina NovaSeq 6000 [48] | Short-read sequencing (2×150 bp) | High-accuracy sequencing for variant calling |
| Sequencing | Oxford Nanopore MinION [48] | Long-read sequencing | Resolution of complex genomic regions and plasmids |
| Quality Control | FastQC [48] | Raw read quality assessment | Identification of sequencing issues and contaminants |
| Genome Assembly | SPAdes [48] | De Bruijn graph assembler | High-quality draft genome assembly from short reads |
| AMR Gene Detection | CARD (Comprehensive Antibiotic Resistance Database) [48] | Curated repository of resistance elements | Identification of known AMR genes and mutations |
| Phylogenetic Analysis | IQ-TREE [48] | Maximum likelihood phylogenetic inference | Reconstruction of evolutionary relationships and transmission chains |
| Data Visualization | Phandango [48] | Interactive phylogenetic tree visualization | Exploration of genotype-phenotype relationships |
Data Integration, Analysis, and Interpretation
From Genomic Data to Public Health Action
The transformation of raw genomic data into actionable public health intelligence requires robust analytical frameworks and interdisciplinary collaboration. Genomic data must be integrated with epidemiological metadata to understand transmission dynamics across One Health sectors [48]. This integration enables researchers and public health professionals to move beyond simply detecting resistance genes to understanding how they are spreading between humans, animals, and environments [48].
Successful implementation of genomics for AMR surveillance depends on establishing clear reporting mechanisms that translate complex genomic findings into interpretable information for public health decision-makers [48]. This includes developing standardized protocols for data analysis, interpretation thresholds, and communication formats that maintain scientific rigor while being accessible to non-specialists [48]. The implementation of FAIR (Findable, Accessible, Interoperable, and Reusable) principles for data sharing ensures that genomic data can be effectively utilized across the global AMR research and public health community [48].
Cross-Sectoral Transmission and Evolution Analysis
Genomic studies have provided unprecedented insights into the transmission dynamics of AMR across One Health compartments. Research has demonstrated links between extended-spectrum beta-lactamase (ESBL)-producing E. coli from human and food chain sources in the UK [48], while other studies have identified sharing of vancomycin-resistant Enterococcus faecium (VREfm) between livestock and humans [48]. These findings highlight the interconnectedness of resistance reservoirs and the importance of integrated surveillance.
At the local level, genomic approaches have revealed complex transmission networks within healthcare settings, informing infection control practices [48]. High-resolution sequencing has enabled researchers to track the movement of carbapenem-resistant Enterobacteriaceae (CRE) between facilities and identify previously unrecognized transmission routes [48]. Similarly, studies of within-host evolution during prolonged infections have provided insights into the evolutionary trajectories leading to resistance development, informing treatment strategies [48].
Implementation Challenges and Future Directions
Barriers to Effective Genomic Surveillance
Despite the transformative potential of genomic approaches for AMR surveillance, significant implementation barriers persist. Many challenges remain for the broader implementation of genomics for AMR at local, regional, and global scales, including limited laboratory infrastructure, technical expertise shortages, and data integration complexities [48]. Equitable access to genomic technologies represents a particular concern, with resource-limited settings—often those with the highest AMR burdens—facing the greatest barriers to implementation [48] [44].
The effective integration of genomic data into public health practice requires overcoming substantial technical and operational hurdles. Establishing robust workflows that meet International Organization for Standardization (ISO) standards and generate interpretable reports for public health and clinical end-users remains challenging [48]. Furthermore, sustainable data management systems capable of handling the volume and complexity of genomic data while ensuring privacy and security require significant investment and coordination across jurisdictions and sectors [48].
Emerging Innovations and Opportunities
The future of AMR genomics is being shaped by several promising technological and methodological innovations. Rapid advances in sequencing technologies, including portable nanopore sequencing and third-generation platforms, are making real-time genomic surveillance increasingly feasible in diverse settings [48]. Coupled with improvements in bioinformatic tools and automated analysis pipelines, these technologies promise to democratize access to genomic surveillance and reduce the time from sample to actionable result.
Machine learning and artificial intelligence approaches are opening new frontiers in AMR prediction and understanding. These methods can identify complex patterns in genomic data that may not be apparent through traditional analysis, potentially enabling more accurate prediction of resistance phenotypes from genomic sequences alone [48]. Additionally, the integration of genomic data with other omics technologies (transcriptomics, proteomics) and clinical metadata promises to provide more comprehensive understanding of resistance mechanisms and host-pathogen interactions [48].
The growing recognition of AMR as a development and equity issue is also shaping future directions [44]. There is increasing emphasis on ensuring that genomic surveillance capacity is strengthened in LMICs and that research addresses the specific needs and contexts of disproportionately affected populations [44]. This includes developing appropriate technologies and frameworks that function effectively in resource-limited settings and address the structural drivers of AMR vulnerability [44].
Genomic technologies have fundamentally transformed our ability to track, understand, and respond to AMR across One Health sectors. The integration of genomic surveillance with public health practice provides unprecedented opportunities to illuminate the complex dynamics of resistance emergence and transmission at local, regional, and global scales. However, realizing the full potential of these approaches requires sustained investment in laboratory infrastructure, technical capacity, and data sharing frameworks, particularly in resource-limited settings.
The continued evolution of AMR demands a corresponding evolution in our surveillance and response capabilities. Future progress will depend on strengthening collaborative networks across human health, animal health, and environmental sectors; developing more accessible and scalable genomic technologies; and building bridges between genomic data and public health action. By embracing a comprehensive One Health approach to genomic surveillance, the global community can develop more effective strategies to preserve antimicrobial efficacy and mitigate the growing threat of AMR to global health, food security, and sustainable development.
Dengue fever represents a critical public health challenge in Brazil, with the country reporting some of the highest case numbers globally. Between 2000 and 2013 alone, Brazil reported more than 7.3 million notified dengue infections [49]. Genomic surveillance has emerged as a transformative tool for understanding and combating dengue virus (DENV) transmission, providing crucial insights into viral evolution, outbreak dynamics, and pathogen spread. This case study examines the application of genomic sciences to dengue surveillance in Brazil through the integrated lens of the One Health framework, which recognizes the interconnectedness of human, animal, and environmental health [11]. We explore how advanced genomic technologies combined with cross-sectoral collaboration are enhancing disease prevention and control strategies for this arboviral threat.
Dengue Virus Diversity and Molecular Epidemiology in Brazil
Circulating Serotypes and Genotypes
Brazil has experienced the co-circulation of all four dengue serotypes (DENV-1 through DENV-4), with different genotypes dominating during distinct outbreak periods. Genomic surveillance has been instrumental in tracking this complex epidemiological landscape:
DENV-4 Genotype Replacement: The 2012 dengue outbreak in Rio de Janeiro was primarily caused by DENV-4 genotype II, forming a monophyletic clade closely related to viruses from Venezuela and northern Brazil [49]. This outbreak marked a significant shift in DENV-4 epidemiology in Brazil. The same study also reported, for the first time in Rio de Janeiro, the detection of DENV-4 genotype I, which appeared to have been introduced from Southeast Asia on separate occasions, demonstrating the value of genomic surveillance in identifying multiple introduction events.
Current Genotype Diversity: More recent data from Yogyakarta, Indonesia (sharing similar DENV ecology with Brazil) reveals the co-circulation of six distinct genotypes across the four serotypes [50], highlighting the substantial genetic diversity that genomic surveillance must track:
- DENV-1: Genotype I (12.5%) and IV (4.7%)
- DENV-2: Cosmopolitan genotype (47%)
- DENV-3: Genotype I (8.5%)
- DENV-4: Genotype II (25.7%) and the recently imported genotype I (1.6%)
Table 1: Dengue Virus Genotypes Circulating in Brazil and Their Characteristics
| Serotype | Genotype | Prevalence | Geographic Origin | First Detection in Brazil |
|---|---|---|---|---|
| DENV-1 | I, IV | Variable across outbreaks | Southeast Asia, Caribbean | 1980s |
| DENV-2 | Cosmopolitan | Dominant in multiple outbreaks | Asia, global distribution | 1990 |
| DENV-3 | I | Significant in multiple outbreaks | Central America, Asia | 2000 |
| DENV-4 | II | Caused major 2012 outbreak | Northern Brazil, Venezuela | 1981-1982 (absent until 2005-2007) |
| DENV-4 | I | Limited circulation | Southeast Asia | 2012 (Rio de Janeiro) |
Molecular Epidemiology and Outbreak Dynamics
Genomic sequencing has revealed critical aspects of DENV transmission patterns in Brazil. The 2012 DENV-4 outbreak in Rio de Janeiro resulted from a viral lineage whose common ancestor was estimated to have emerged in February 2010 [49]. This lineage then spread from northern Brazil to more densely populated southeastern states, demonstrating how genomic data can reconstruct transmission pathways.
Analysis of the Applying Wolbachia to Eliminate Dengue (AWED) trial showed "strong spatial and temporal structure to the DENV genomic relationships, consistent with highly focal DENV transmission around the home" [50]. This fine-scale understanding of transmission patterns directly informs targeted intervention strategies.
Genomic Surveillance Methodologies
Laboratory Workflows for DENV Genomic Characterization
The standard genomic surveillance pipeline for dengue virus involves sample collection, processing, sequencing, and bioinformatics analysis.
Figure 1: Workflow for Dengue Virus Genomic Surveillance
Sample Collection and Processing: Surveillance begins with sample collection from human cases (e.g., plasma from febrile patients) or mosquito vectors [50]. During the AWED trial, venous blood was collected from participants with acute febrile illness of 1-4 days duration [50]. Viral RNA is then extracted using commercial kits such as the High Pure Viral Nucleic Acid Kit (Roche) [50].
Reverse Transcription and Amplification: Extracted RNA undergoes reverse transcription into complementary DNA (cDNA) using systems such as SuperScript IV First-strand Synthesis System with random hexamers [50]. The viral genome is then amplified in multiple overlapping fragments using DENV-specific primers in separate PCR reactions.
Library Preparation and Sequencing: Amplified products are purified and used for library construction with kits such as Nextera XT DNA Library Preparation Kit (Illumina) [50]. Libraries are normalized, pooled, and sequenced on platforms such as Illumina NextSeq2000 using 300-cycle kits [50].
Bioinformatics Analysis Pipelines
The bioinformatics workflow for DENV genomic surveillance includes multiple critical steps:
Quality Control and Read Processing: Raw sequencing reads undergo quality trimming and adapter removal using tools such as AlienTrimmer, with short reads (<50 bases) and low-quality bases (quality score <30) being filtered out [50].
Alignment and Consensus Generation: Processed reads are aligned to DENV reference genomes using aligners such as BWA-MEM [50]. Consensus sequences are then generated using variant callers such as iVar with default parameters [50]. Regions with coverage below 10× may be imputed from consensus sequences of relevant DENV genotypes.
Phylogenetic and Evolutionary Analysis: Multiple sequence alignment is performed with tools such as MAFFT, followed by phylogenetic reconstruction using maximum likelihood methods in IQ-TREE or Bayesian approaches [50] [51]. Genotypes are assigned by examining consensus trees with statistical support measures.
Table 2: Essential Research Reagents and Tools for DENV Genomic Surveillance
| Category | Item | Specific Example | Function in Workflow |
|---|---|---|---|
| Sample Processing | Nucleic Acid Extraction Kit | High Pure Viral Nucleic Acid Kit (Roche) | RNA extraction from plasma or mosquito samples |
| Molecular Biology | Reverse Transcription System | SuperScript IV First-Strand Synthesis System | cDNA synthesis from viral RNA |
| PCR Amplification Reagents | DENV-specific primer pools | Whole genome amplification in fragments | |
| Sequencing | Library Prep Kit | Nextera XT DNA Library Preparation Kit (Illumina) | Preparation of sequencing libraries |
| Sequencing Platform | Illumina NextSeq2000 with P2 v3 300-cycle kit | High-throughput sequencing | |
| Bioinformatics | Quality Control Tool | AlienTrimmer | Adapter removal and read quality filtering |
| Sequence Aligner | BWA-MEM | Alignment of reads to reference genomes | |
| Variant Caller | iVar | Consensus sequence generation | |
| Phylogenetic Software | IQ-TREE, PhyML, MrBayes | Evolutionary analysis and tree building |
The One Health Framework in Dengue Surveillance
Integrated Surveillance Approaches
The One Health concept emphasizes transdisciplinary approaches to address complex health challenges at the human-animal-environment interface [11]. For dengue surveillance, this translates to integrated systems that monitor viral activity across multiple components of the ecosystem.
Entomological Surveillance: Mosquito collections and screening provide early warning of DENV transmission. A study in São Paulo state demonstrated this approach by testing collected Aedes aegypti and Ae. albopictus mosquitoes for CHIKV RNA, with 5.6% of specimens testing positive during outbreak periods [52]. Similar methodologies apply directly to DENV surveillance.
Environmental and Climate Factors: The abundance of Aedes mosquitoes is significantly influenced by abiotic factors such as precipitation and temperature [52]. Surveillance systems that incorporate climate data can better predict outbreak risks and seasonal patterns.
Cross-Species Genomic Analyses
The One Health approach leverages comparative genomics across species to enhance predictive capabilities. Research initiatives are exploring "whether techniques developed to test such traits in animal and plant genetics might be adapted to explore such questions in the human genome" [10]. This cross-phyla approach may reveal novel insights into host-pathogen interactions and transmission dynamics.
Figure 2: One Health Approach to Dengue Surveillance
Applications and Impact on Public Health
Outbreak Investigation and Transmission Tracking
Genomic sequencing has proven invaluable for understanding DENV outbreak dynamics in Brazil. Analysis of the 2012 Rio de Janeiro outbreak revealed a strong correlation between genetic data and epidemiological patterns [49]. The combination of "genetic and epidemiological data from blood donor banks" has shown potential for anticipating epidemic spread of arboviruses [49].
The AWED trial demonstrated how genomic surveillance can evaluate intervention effectiveness. The study showed "wMel protection extended to all six genotypes identified amongst AWED trial participants" [50], with the Wolbachia intervention causing a "near-total disruption of transmission" [50]. This genotypic efficacy assessment is crucial for understanding the broad-spectrum protection offered by such biocontrol approaches.
Vaccine and Intervention Development
Genomic surveillance provides critical data for vaccine development and evaluation through:
Genotype-Specific Efficacy Assessment: The AWED trial enabled estimation of "genotype-specific protective efficacies of wMel, which were similar (±10%) to the point estimates of the respective serotype-specific efficacies" [50]. This granular assessment ensures interventions remain effective across diverse viral genotypes.
Viral Evolution Monitoring: Continuous genomic surveillance detects mutations that might affect vaccine efficacy or disease severity, enabling proactive strategy adjustments.
Challenges and Future Directions
Implementation Barriers in Resource-Limited Settings
Despite its transformative potential, genomic surveillance implementation faces significant challenges in Brazil and similar settings:
Resource and Infrastructure Limitations: Many Latin American countries have limited research and development investment, with national budgets for R&D "approximately one hundred-fold less than in high-income countries" [53]. This affects access to sequencing technologies, reagents, and computational resources.
Technical Capacity Building: Establishing sustainable genomic surveillance requires training personnel in both laboratory methodologies and bioinformatics analysis. Initiatives such as the Asian-American Center for Arbovirus Research and Enhanced Surveillance (A2CARES) have focused on "capacity-strengthening and peer training workshops for local health scientists" [53] to address this gap.
Data Integration and Interpretation: Combining genomic data with epidemiological and clinical information remains challenging. Effective "integration of genomic data with environmental and epidemiological information" [11] requires standardized protocols and interdisciplinary collaboration.
Advancing Genomic Surveillance Capabilities
Future directions for enhancing dengue genomic surveillance in Brazil include:
Portable Sequencing Technologies: Field-deployable sequencing devices can enable rapid, local genomic characterization during outbreaks, reducing dependency on central laboratories.
South-South Collaboration: Partnerships between scientifically developing countries facilitate technology transfer and knowledge sharing. The collaboration between Nicaragua and Ecuador exemplifies how "South-South exchange of expertise in genomic sequencing" [53] builds regional capacity.
Standardized Frameworks: Developing consistent protocols for sample processing, data generation, and analysis ensures comparability across studies and regions. This includes addressing "data integration, standardization, and ethical considerations in genomic research" [11].
Genomic surveillance has revolutionized dengue monitoring and response in Brazil, providing unprecedented insights into viral diversity, transmission patterns, and outbreak dynamics. When implemented within a One Health framework that integrates human, vector, and environmental data, genomic approaches offer a powerful tool for understanding and controlling this significant public health threat. Despite ongoing challenges related to resource limitations and capacity building, continued advancements in sequencing technologies, bioinformatics, and international collaboration promise to further enhance Brazil's capacity to track and respond to dengue outbreaks. The institutionalization of genomic surveillance systems, as demonstrated during the COVID-19 pandemic [53], provides a foundation for sustainable arbovirus monitoring that will remain essential for public health security in the face of emerging and reemerging infectious diseases.
This case study details a comprehensive genome-wide analysis of Klebsiella pneumoniae species complex (KpSC) conducted within a One Health framework in Norway. The research analyzed 3,255 whole-genome sequenced isolates from human, animal, and marine sources collected over a 20-year period (2001-2020) to assess diversity, niche-enriched traits, and cross-reservoir transmission dynamics. Results revealed distinct but overlapping populations across niches, with limited recent direct transmission events but notable spillover of clinically relevant genetic features. Human-to-human transmission was identified as the primary route of infection, yet the study provides genomic evidence of plasmid-mediated virulence gene exchange between animal and human reservoirs. This investigation establishes a methodological blueprint for integrating large-scale genomic data into One Health research and informs targeted public health interventions for antimicrobial resistance management.
The One Health concept underscores the interconnectedness of human, animal, and environmental health, necessitating an integrated, transdisciplinary approach to tackle contemporary health challenges [11]. Genomic technologies have emerged as pivotal tools in One Health initiatives, enabling researchers to decode complex biological data for comprehensive insights into pathogen evolution, transmission dynamics, and host-pathogen interactions across species and ecosystems [11] [7].
Klebsiella pneumoniae species complex (KpSC) represents a group of opportunistic pathogens that cause severe and difficult-to-treat infections, particularly concerning with the emergence of multidrug-resistant (MDR) and hypervirulent strains [54] [55]. KpSC members are unique in their ability to colonize diverse niches, including humans, animals, and marine environments, before causing infections, raising critical questions about their transmission pathways and the clinical relevance of non-human reservoirs [55].
This case study presents a detailed examination of KpSC in Norway through a One Health genomic lens, serving as a model for integrating large-scale genomic data to address fundamental questions in pathogen ecology and transmission. The study leverages Norway's unique position with its low antimicrobial resistance prevalence, providing an exceptional opportunity to study niche connectivity in a population largely unaffected by antibiotic selection pressures [55].
Materials and Experimental Methods
Sample Selection and Collection
The study employed a comprehensive sampling strategy encompassing diverse reservoirs across Norway (2001-2020). The collection and processing of isolates followed a standardized protocol to ensure consistency and comparability across niches.
Table: Sample Distribution Across Reservoirs
| Source Type | Subcategories | Number of Isolates | Collection Years | Sampling Details |
|---|---|---|---|---|
| Human Infections | Blood (n=1,920); Urine (n=252) | 2,172 | 2001-2018 | Nationwide surveillance across 22 clinical microbiology laboratories |
| Human Carriage | Fecal carriage | 484 | 2015-2016 | General adult population, Tromsø municipality |
| Marine Environments | Bivalves/sea urchins (n=92); Surface seawater (n=7) | 99 | 2016, 2019, 2020 | 77 production areas + 5 non-rearing locations; pooled samples (10-20 individuals) |
| Food-Producing Animals | Pigs (n=146); Turkey flocks (n=173); Broiler flocks (n=145); Wild boars (n=27); Dogs (n=16); Cattle (n=12) | 500+ | 2018-2020 | Norwegian monitoring program for AMR in veterinary sector (NORM-VET); caecal/faecal samples |
Genome Sequencing and Assembly
The study utilized a dual sequencing approach to maximize data quality and completeness:
- Short-read sequencing: All 3,255 isolates were sequenced using Illumina platforms (3,218 on MiSeq, 37 on HiSeq 2500) [55].
- Long-read sequencing: A subset of 550 isolates (16.9%) underwent Oxford Nanopore Technologies (ONT) sequencing to produce closed hybrid genomes for enhanced assembly and plasmid characterization [55].
- Bioinformatic processing: Raw reads underwent adapter- and quality-filtering with TrimGalore v0.6.7 and were assembled with SPAdes v3.15.4 [55]. All genomes underwent rigorous quality control as detailed in supplementary methods.
Genomic Analysis Framework
The analytical framework incorporated multiple complementary approaches:
- Population structure analysis: Strains were classified into sublineages (SLs) and core-genome sequence types (STs) using established KpSC classification schemes [55].
- Phylogenomic analysis: Core genome phylogenies were constructed to assess genetic relationships across niches.
- Accessory genome analysis: Gene content variation was assessed to identify niche-associated genetic elements.
- Genome-Wide Association Studies (GWAS): Statistical approaches identified genetic features enriched in specific niches.
- Transmission analysis: Thresholds of ≤22 single nucleotide polymorphisms (SNPs) were used to identify closely related isolates indicative of recent transmission events [55].
Diagram Title: One Health Genomic Analysis Workflow
Results and Interpretation
Population Structure and Genetic Diversity
The analysis revealed a complex population structure with significant diversity both between and within niches:
- KpSC populations from different niches were distinct but overlapping, indicating both niche-specific adaptation and cross-reservoir exchange [54].
- The accessory genome showed remarkable diversity, with approximately 49% of genes overlapping across ecological niches, suggesting substantial gene flow between reservoirs [54].
- Several sublineages (SLs) were commonly distributed across sources, including SL17, SL35, SL37, SL45, SL107, and SL3010, indicating these lineages have generalist capabilities enabling survival in diverse environments [55].
Table: Distribution of Key Genetic Features Across Niches
| Genetic Feature | Human Infections | Human Carriage | Pigs | Poultry | Marine |
|---|---|---|---|---|---|
| Sublineages (SLs) | SL17, SL35, SL37, SL45, SL107 | SL17, SL35, SL37 | SL17, SL35, SL37, SL107 | SL35, SL37, SL45 | SL17, SL37, SL3010 |
| Aerobactin-encoding plasmids | Limited | Limited | Enriched | Present | Absent |
| Colicin a | Limited | Limited | Enriched | Present | Absent |
| iuc3 virulence locus | Present | Present | Enriched | Limited | Absent |
Niche-Enriched Genetic Traits
GWAS approaches identified specific genetic elements associated with particular niches:
- Aerobactin-encoding plasmids and the bacteriocin colicin a were significantly associated with KpSC from animal sources, particularly pigs [54] [55].
- Human infection isolates showed the greatest connectivity with each other, followed by isolates from human carriage, pigs, and bivalves, suggesting stronger within-niche transmission networks [55].
- Despite temporally and geographically distant sampling, nearly 5% of human infection isolates had close relatives (≤22 substitutions) among animal and marine isolates, providing evidence for cross-reservoir transmission [54].
Transmission Dynamics Across Reservoirs
The study provided nuanced insights into transmission patterns:
- Human-to-human transmission was more frequent than transmission between ecological niches, emphasizing the importance of infection control in healthcare settings [54].
- Limited but notable recent spillover events were detected, including the movement of plasmids encoding the virulence locus iuc3 between pigs and humans [55].
- The identification of closely related isolates across reservoirs despite non-synchronous sampling suggests that undetected intermediary transmission chains or environmental persistence may facilitate cross-reservoir transmission [55].
Diagram Title: KpSC Transmission Network Across Niches
The Scientist's Toolkit: Research Reagent Solutions
This section details essential reagents, technologies, and computational tools employed in this One Health genomic study, providing a resource for researchers designing similar investigations.
Table: Essential Research Reagents and Platforms for One Health Genomic Studies
| Category | Specific Tool/Technology | Application in Study | Technical Considerations |
|---|---|---|---|
| Sequencing Platforms | Illumina MiSeq/HiSeq 2500 | Primary short-read sequencing of all isolates | High accuracy, cost-effective for large sample sizes |
| Oxford Nanopore Technologies (ONT) | Long-read sequencing for hybrid assembly (16.9% of isolates) | Resolves complex regions, enables complete plasmid assembly | |
| Bioinformatics Tools | TrimGalore v0.6.7 | Adapter trimming and quality control | Critical for data standardization across batches |
| SPAdes v3.15.4 | Genome assembly from short reads | Produces high-quality draft genomes | |
| Hybrid assembly pipelines | Combine short and long reads for complete genomes | Essential for plasmid and repetitive element resolution | |
| Analytical Frameworks | Genome-Wide Association Study (GWAS) | Identification of niche-enriched genetic traits | Requires careful correction for population structure |
| Phylogenomic analysis | Reconstruction of evolutionary relationships | Core genome approaches provide highest resolution | |
| Transmission analysis | Inference of recent transmission events | ≤22 SNP threshold balances sensitivity/specificity | |
| Specialized Reagents | Multiplexed library preparation kits | High-throughput sequencing library construction | Enables cost-effective processing of large sample sets |
| Quality control reagents (Qubit, Bioanalyzer) | DNA quantification and qualification | Essential for sequencing success |
Discussion
Implications for Public Health Interventions
The findings from this One Health genomic analysis carry significant implications for designing effective public health interventions:
- Infection prevention measures in clinical settings remain essential, given the predominance of human-to-human transmission [54].
- Preventing transmission from direct animal contact or via the food chain could play an important role in reducing the KpSC disease burden, particularly for virulent strains [55].
- Surveillance programs should incorporate zoonotic and environmental monitoring to detect emerging threats, as even rare spillover events can introduce clinically significant strains or genetic elements into human populations [7].
Methodological Considerations for One Health Genomics
This case study highlights several critical methodological aspects for One Health genomic investigations:
- Sympatric sampling across multiple reservoirs is essential but logistically challenging; collaborative networks across human, animal, and environmental health sectors are crucial [55].
- Hybrid sequencing approaches (combining short- and long-read technologies) provide complementary advantages for comprehensive genomic characterization [55] [56].
- Temporal and geographic sampling design must account for potential lag periods in transmission and population dynamics across reservoirs [54].
Integration with European Genomic Initiatives
This study aligns with broader European efforts to advance genomic medicine, including the 1+ Million Genomes (1+MG) initiative which aims to enable secure access to genomics and corresponding clinical data across Europe [57] [58]. The Genomic Data Infrastructure (GDI) project, deploying a federated, sustainable, and secure infrastructure for genomic and clinical data access, provides a framework that could expand to incorporate One Health data [57] [59]. Such integration would enhance cross-border collaboration and enable more comprehensive understanding of pathogen dynamics across human, animal, and environmental interfaces.
This One Health genomic analysis of Klebsiella pneumoniae in Norway demonstrates the power of integrated genomic approaches to elucidate complex transmission dynamics at the human-animal-environment interface. While human-to-human transmission predominates for KpSC, the study provides definitive evidence of cross-reservoir spillover of clinically relevant strains and mobile genetic elements, particularly between pig and human populations.
The methodological framework presented offers a blueprint for future One Health genomic studies, emphasizing the importance of standardized protocols, comprehensive sampling, and advanced bioinformatic integration. As genomic technologies become increasingly accessible and bioinformatic capabilities expand, the integration of One Health principles into public health surveillance and intervention strategies will be crucial for addressing the interconnected challenges of antimicrobial resistance, emerging pathogens, and global health security.
The findings reinforce that safeguarding human health requires a holistic approach that considers the complex ecological networks in which pathogens evolve and spread. Future research should build upon this foundation to explore functional mechanisms of niche adaptation and expand surveillance to underrepresented reservoirs, ultimately enabling more predictive and proactive public health interventions.
Overcoming Implementation Hurdles: Data, Bioinformatics, and Collaborative Frameworks
Addressing Computational and Bioinformatics Challenges in Large-Scale Data Analysis
The One Health concept underscores the inextricable linkages between human, animal, and environmental health, promoting an integrated, transdisciplinary approach to tackle contemporary health challenges [60]. In genomic sciences, this approach necessitates comprehensive surveillance and analysis of pathogens, antimicrobial resistance (AMR) markers, and health determinants across all three domains [61] [7]. However, the implementation of this vision faces significant computational and bioinformatics hurdles due to the enormous scale, diversity, and distributed nature of the resulting genomic data. The projection that antimicrobial resistance alone could cause 10 million deaths annually by 2050 has reinforced its status as one of the greatest global health threats of the 21st century, demanding more sophisticated analytical approaches [61]. This technical guide examines the core computational challenges in One Health genomics and provides detailed methodologies for overcoming them, enabling researchers to advance this critical field.
Core Computational Challenges in One Health Genomics
The integration of multi-sectoral genomic data within a One Health framework presents distinct computational obstacles that must be addressed to realize its full potential. These challenges span data management, processing, analysis, and interpretation phases.
Table 1: Key Computational Challenges in Large-Scale One Health Genomics
| Challenge Category | Specific Technical Hurdles | Impact on One Health Research |
|---|---|---|
| Data Volume & Transfer | Petabyte-scale data generation; network limitations for transfer [62] | Hinders integration of distributed human, animal, and environmental datasets |
| Data Heterogeneity | Non-standardized formats across platforms and sectors [61] [62] | Impedes cross-species comparisons and integrated analysis |
| Computational Complexity | NP-hard problems (e.g., Bayesian network reconstruction); memory-intensive operations [62] | Limits ability to model complex health interactions across domains |
| Resource Constraints | High sequencing costs; bioinformatics complexity; infrastructure limitations in tropical regions [61] [7] | Creates geographic disparities in One Health implementation capacity |
| Data Integration & Visualization | Merging multi-omics datasets (genomic, proteomic, metabolomic) [63] | Challenges in creating unified views of cross-sectoral health relationships |
The challenges are particularly acute in tropical regions, which contain over 80% of Earth's biodiversity and approximately 40% of the global population, yet face significant infrastructure limitations [7]. Additionally, the separation of human, animal, and plant genetics into distinct research silos has historically limited the exchange of analytical methods and insights between these critical One Health domains [10].
Bioinformatics Solutions for Large-Scale Data Processing
Computational Frameworks and Workflow Management
Effective processing of One Health genomic data requires robust computational frameworks and workflow management systems designed for scale and reproducibility. The following guidelines provide a foundation for large-scale data processing:
- Rule 1: Don't reinvent the wheel – Check for published or pre-processed data that could be useful before initiating new analyses [64]
- Rule 2: Document everything – Track all rationale and decisions used in your work to ensure reproducibility and collaboration
- Rule 4: Automate your workflows – Implement systems that support repeated analysis using workflow tools like Nextflow or Snakemake
- Rule 6: Version both software and data – Maintain version control for all related software, workflows, and data in pipelines
- Rule 7: Continuously measure and optimize performance – Regularly assess workflow and algorithm performance to identify optimization opportunities [64]
A critical supplementary rule involves understanding where the computational burden originates and designing around it [64]. Different analysis types impose distinct requirements – some demand extensive computing power, while others require substantial memory or storage resources. For variant calling across multiple samples in a One Health context, the natural approach is to distribute one sample per analysis initially, then perform joint variant calling by distributing work per chromosome or genomic region [64].
Diagram 1: Computational workflow for One Health genomic data analysis (76 characters)
Data Management and Metadata Strategies
Organizing files and analyses with comprehensive metadata is crucial for One Health genomics, where data originates from diverse sources and requires integration. Effective metadata management includes:
- Implementing patterned, self-explanatory naming conventions for files and analyses (e.g.,
<sampleID>_<source>_<processing>.fileformat) [64] - Creating manifest files that record filename, file path, file signature (e.g., MD5), and description of abbreviations
- Attaching metadata tags to analysis batches to facilitate tracking and reanalysis when necessary
- Following FAIR principles (Findable, Accessible, Interoperable, Reusable) to enhance data sharing and reuse [64]
For One Health applications, metadata should specifically capture the originating domain (human, animal, environmental), geographical location, sampling date, and relevant ecological parameters to enable meaningful cross-domain analysis.
Experimental Protocols for One Health Genomic Surveillance
Integrated Genomic Surveillance for Antimicrobial Resistance
Comprehensive AMR surveillance requires a dual approach combining isolate-based whole-genome sequencing (WGS) with shotgun metagenomics for complex matrices [61]. The following protocol provides a detailed methodology:
Sample Collection and Processing:
- Clinical settings: Collect bacterial isolates from patients, prioritizing WHO Priority Pathogens and multidrug-resistant strains [61]
- Animal reservoirs: Sample livestock, poultry, and wildlife using appropriate ethical guidelines
- Environmental sources: Collect water, soil, and wastewater samples using standardized sampling methodologies
- Extract high-quality genomic DNA using optimized kits for each sample type, with rigorous quality control
Sequencing Methodologies:
- For isolate WGS: Utilize both short-read (Illumina) for high accuracy SNP detection and long-read technologies (Oxford Nanopore, PacBio) for complete genome assemblies and plasmid reconstruction [61] [5]
- For metagenomic surveillance: Employ shotgun metagenomics with sequencing depth balanced between sensitivity for rare resistance genes and financial feasibility
- Implement real-time sequencing technologies (e.g., Oxford Nanopore MinION) for rapid in-situ analysis when timely intervention is critical [5]
Bioinformatic Analysis:
- Process raw sequencing data through standardized bioinformatics pipelines for quality control, assembly, and annotation
- Annotate antimicrobial resistance genes (ARGs) using established databases (e.g., NCBI AMRFinder, ResFinder)
- Identify mobile genetic elements (MGEs) and plasmid sequences to track horizontal gene transfer potential
- Perform phylogenetic analysis and strain typing to delineate transmission routes across One Health sectors
- Integrate clinical, epidemiological, and environmental metadata to identify resistance hotspots and transmission pathways
Technical Considerations:
- For WGS: Achieve ≥100× coverage for precise SNP detection and outbreak investigations; 30-50× coverage suffices for broader surveillance [61]
- For metagenomics: Optimize DNA extraction methods for complex environmental samples where resistance genes may be present at low abundances
- Standardize data outputs using interoperable formats to enable cross-sectoral comparisons
Cross-Species Genomic Analysis Protocol
The Purdue University One Health initiative demonstrates innovative approaches for cross-species genomic analyses that leverage methods developed in animal and plant genetics for human health applications, and vice versa [10]. The following protocol outlines this methodology:
Data Collection:
- Human data: Utilize large-scale biobanks (e.g., UK Biobank) with genomic and phenotypic data, including accelerometer data for activity tracking [10]
- Animal data: Implement sensor technologies (e.g., cameras, activity monitors) in livestock settings to track multiple traits simultaneously
- Plant data: Access genomic databases (e.g., EnsemblPlants, JGI Plant Gene Atlas) for comparative analysis
- Ensure ethical compliance and data governance for all human data applications
Analytical Framework:
- Cross-train researchers with expertise in different domains (human, animal, plant genetics) to facilitate methodological exchange [10]
- Adapt algorithms and models developed in animal genetics for complex trait analysis to human genomic data
- Apply genome-wide association study (GWAS) methods across species to identify conserved biological mechanisms
- Develop cross-species genomic prediction models that leverage the larger datasets available in animal and plant genetics
Implementation:
- Create computational graphs that identify parallel processing opportunities across domains
- Distribute analysis by logical units (per sample, per chromosome, per region) depending on the specific application
- Utilize cloud computing environments to enable scalability and access to diverse datasets
- Implement continuous performance monitoring and optimization of cross-species algorithms
Visualization Tools for Complex Genomic Data
Effective visualization is essential for interpreting the complex relationships in One Health genomic data. The Gviz package in Bioconductor provides a flexible framework for visualizing genomic data in the context of diverse annotation features, integrating tightly with existing Bioconductor infrastructure [65]. Key capabilities include:
- Direct data retrieval from external sources like Ensembl and UCSC
- Support for common annotation file types
- Carefully chosen default settings that facilitate production of publication-ready figures
- High customization options for specialized applications
For large-scale genomic datasets, visual scalability becomes critical [66]. As genomic datasets grow exponentially, visualization tools must efficiently represent data at different resolutions – from chromosome-level structural variations to nucleotide-level sequences. This requires:
- Implementing multiple coordinated views for different data types (e.g., Hi-C, epigenomic signatures, variant calls)
- Using visual encodings that maintain clarity at different scales
- Offering interactive exploration capabilities for complex datasets
- Ensuring accessibility for visually impaired researchers through colorblind-friendly palettes and customizable visualizations [66]
Table 2: Essential Bioinformatics Tools for One Health Genomics
| Tool Category | Specific Tools | Application in One Health |
|---|---|---|
| Workflow Management | Nextflow, Snakemake, Apache Hadoop [63] [64] | Automated processing of multi-sectoral genomic data |
| Variant Analysis | GATK, BCFtools [63] | Cross-species variant identification and annotation |
| Genome Visualization | Gviz, IGV, UCSC Genome Browser [65] [66] | Visual integration of genomic data across domains |
| Metagenomic Analysis | MetaPhlAn, HUMAnN, SHOGUN | Profiling microbial communities across environments |
| Database Integration | BioMart, NCBI GenBank, EMBL-EBI [63] | Accessing and combining diverse biological data |
| Cloud Platforms | Google Cloud Life Sciences, AWS Genomics Workflows [63] | Scalable computation for large One Health datasets |
Diagram 2: One Health genomic data analysis and visualization pipeline (82 characters)
Table 3: Essential Research Reagents and Computational Resources for One Health Genomics
| Resource Category | Specific Items | Function in One Health Research |
|---|---|---|
| Sequencing Technologies | Oxford Nanopore MinION, Illumina NovaSeq, PacBio Sequel [61] [5] | Portable and high-throughput DNA/RNA sequencing across field and lab settings |
| DNA Extraction Kits | Optimized kits for diverse sample types (clinical, environmental, veterinary) | High-quality DNA extraction from varied One Health specimen sources |
| Cloud Computing Platforms | Google Cloud Life Sciences, AWS Genomics, Microsoft Bioinformatics [63] | Scalable computational resources for large-scale cross-domain analyses |
| Bioinformatics Pipelines | Nextflow/Snakemake workflows, GATK, BCFtools [63] [64] | Standardized processing and analysis of genomic data across projects |
| Genomic Databases | NCBI GenBank, EMBL-EBI, ResFinder, Pathogenwatch [61] [63] | Reference data for annotation and comparative analysis |
| Visualization Tools | Gviz, IGV, Cytoscape, Tableau [65] [66] [63] | Visual exploration and communication of complex cross-domain relationships |
| Sample Collection Materials | Environmental sampling kits, veterinary swabs, clinical specimen containers | Standardized collection of samples across One Health domains |
Addressing the computational and bioinformatics challenges in large-scale data analysis is fundamental to advancing the One Health agenda in genomic sciences. By implementing robust computational frameworks, standardized protocols, and scalable visualization tools, researchers can effectively integrate genomic data across human, animal, and environmental domains. The solutions outlined in this guide – from workflow automation and metadata management to cross-species analytical methods – provide a foundation for extracting meaningful insights from complex One Health datasets. As genomic technologies continue to evolve, particularly with the advent of real-time sequencing [5], the computational approaches described here will enable more timely interventions and evidence-based policies to promote health across all sectors. Strategic investment in bioinformatics capacity, particularly in underserved tropical regions [7], will be essential to ensuring equitable implementation of One Health genomics worldwide.
The One Health concept underscores the inextricable links between human, animal, and environmental health, advocating for a unified approach to tackle complex global health challenges [60]. In genomic sciences, this approach is particularly crucial, as pathogens and antimicrobial resistance genes circulate freely across species and ecosystems, disregarding disciplinary boundaries. The modern landscape of global health threats, including emerging infectious diseases and antimicrobial resistance (AMR), demands a collaborative, transdisciplinary methodology that traditional sector-specific approaches cannot adequately address [67]. Genomic research, with its capacity to decode complex biological data across species, provides an unprecedented opportunity to understand pathogen evolution, transmission dynamics, and host-pathogen interactions at the human-animal-environment interface [60].
Despite this potential, significant structural and operational barriers impede effective collaboration. Fragmented funding streams, disciplinary silos, and absence of standardized protocols often prevent the integration of knowledge and resources necessary for comprehensive One Health genomic surveillance [68]. The institutionalization of multisectoral coordination remains highly complex, requiring deliberate strategies to bridge communication gaps, align priorities, and establish shared frameworks for data generation and interpretation [69]. This technical guide outlines evidence-based strategies and practical methodologies for fostering effective multi-sectoral and multi-disciplinary collaboration in One Health genomic research, providing researchers, scientists, and drug development professionals with the tools to break down persistent silos and harness the full potential of integrative science.
Conceptual Framework: Distinguishing Coordination from Collaboration
A foundational step in building effective multi-sectoral partnerships involves precisely understanding key terms often used interchangeably. Within the context of One Health initiatives, coordination and collaboration represent distinct but complementary concepts in the spectrum of partnership.
Coordination refers to the organization and management of human and/or physical resources to achieve a common goal, serving as a core element of collaboration [69]. It focuses on organizing people, organizations, or resources but does not always require reciprocal engagement. A practical example includes a team leader delegating tasks to team members or the allocation of vaccines from national warehouses to subnational storage centers.
Collaboration, in contrast, describes an evolving process involving the active and reciprocal engagement of two or more social entities (e.g., people, teams, organizations) working together toward a shared goal [69]. This process occurs at multiple levels, including within the same team, across teams, departments, organizations, sectors, and between countries.
Dr. Muhammad Sartaj illustrated this distinction using the example of an orchestra: "During a performance, the conductor coordinates the musicians by guiding them with hand movements as they play a symphony. This is coordination. However, the process that takes place before the performance—such as rehearsals, sitting together, and sharing knowledge—is an example of collaboration" [69]. This analogy clarifies that while coordination manages aligned activities, collaboration involves deeper integration of expertise and shared learning. For One Health genomic research, both elements are essential: coordination ensures efficient operational workflows, while collaboration enables the transdisciplinary integration of knowledge required to interpret complex genomic data across health domains.
Systemic Barriers to Effective One Health Collaboration
Implementing successful One Health programs, particularly in genomics, requires navigating significant systemic barriers. Evidence from low- and middle-income countries (LMICs) and global assessments highlights consistent challenges that hinder effective multi-sectoral collaboration.
Table 1: Key Systemic Barriers to One Health Collaboration
| Barrier Category | Specific Challenges | Impact on Genomic Research |
|---|---|---|
| Governance & Political Will | Lack of political will, weak governance, unclear goals and roles, absence of formal policy decision-making processes [70] [68]. | Fragmented leadership for cross-sector genomic surveillance initiatives; inadequate policy support for data sharing. |
| Funding Structures | Top-down funding frameworks that create silos, competing priorities between sectors, rivalries over budget allocation [70] [68]. | Disconnected funding streams for human, animal, and environmental genomics; limited resources for integrated AMR surveillance. |
| Technical & Resource Capacity | Lack of human, financial, and logistics resources, high sequencing costs, bioinformatics complexity [70] [71]. | Limited capacity for WGS and metagenomics in veterinary and environmental health programs; inequitable resource distribution. |
| Data Standardization | Variability of sub-cultures within disciplines, inconsistencies in sequencing protocols across laboratories, absent standardized bioinformatics workflows [68] [71]. | Hindered cross-sector comparability; inability to track resistance transmission across geographic and ecological boundaries. |
| Trust & Institutional Dynamics | Limited trust and co-ownership within and between organizations, conflicting priorities between stakeholders from different sectors [69] [68]. | Reluctance to share preliminary genomic data; insufficient credit-sharing mechanisms across disciplines. |
These barriers collectively create a landscape where siloed operations often prevail over integrated approaches. Particularly in genomic AMR surveillance, implementation remains fragmented, predominantly focused on clinical settings with insufficient integration across One Health compartments [71]. Addressing these challenges requires targeted strategies that create enabling environments for collaboration, which we explore in the following section.
Foundational Strategies for Building Collaborative Frameworks
Establishing Governance Structures and Formalizing Coordination
The integration of coordination mechanisms within governmental and research bodies requires establishing supportive policies, legislation, and frameworks to enable their effective operationalization. Enacting such legal frameworks strengthens national governance of coordination bodies, facilitates resource allocation, and enhances accountability [69]. A critical first step involves identifying and formally engaging relevant sectors. The purpose and rationale for engaging sectors must be clearly delineated and articulated to ensure the right sectors are involved, optimize resource use, increase transparency, and foster trust [69].
EMPHNET's Stakeholder Mapping and Analysis Tool provides a structured approach for this process, using three primary domains to assess and prioritize stakeholders [69]:
- Expertise: Contribution and legitimacy in the relevant field.
- Willingness to Engage: Readiness and motivation to participate.
- Value: Influence, necessity of involvement, and extent of geographical involvement.
Following stakeholder identification, Dr. Scott Dowell recommends that countries and research consortia employ a systematic approach to public health emergency coordination that is equally applicable to sustained research collaboration. This approach includes four main steps [69]:
- Identifying the Leaders: Select three to five leaders from relevant sectors in advance using a stakeholder mapping tool.
- Identifying Main Coordination Activities: Leaders agree on planned activities and take responsibility for coordinating implementation.
- Practice: Regularly exercise coordination plans through simulations and drills.
- Continuous Quality Improvement: Implement systems for ongoing refinement of coordination mechanisms.
Practical Toolkit for Implementing Multisectoral Collaboration
A structured toolkit for implementing multisectoral collaboration, developed by the Centre for Environmental and Social Health (CESH), provides a dynamic, iterative process involving four key steps [72]. The following diagram visualizes this continuous cycle:
Diagram 1: Multisectoral Collaboration Cycle. This framework outlines the four iterative steps for establishing and maintaining effective collaboration, emphasizing continuous learning and adaptation [72].
For each step in this cycle, specific tools and processes enhance effectiveness:
Step 1: Convene and Plan - This foundational stage involves stakeholder mapping and analysis to identify key actors, followed by jointly defining the problem using systems thinking, establishing shared goals, and agreeing on implementation approaches [72]. This ensures all participants have a shared understanding of objectives and commitment to the collaborative process.
Step 2: Establish Structure - Critical operational elements include clarifying roles and responsibilities, agreeing on leadership models that emphasize traits facilitating collaboration, setting up governance mechanisms and processes, and planning administrative coordination to support shared vision [72].
Step 3: Execute and Coordinate - Implementation requires clear coordination channels, continuous reflection and adaptation using frameworks like the 5R framework or CARL framework, and active relationship building and maintenance among partners [72].
Step 4: Monitor and Adapt - Continuous evaluation assesses both the collaboration's effectiveness and its outcomes, with findings disseminated to stakeholders to generate appropriate solutions that enhance collaboration [72].
Enabling Factors for Sustained Collaboration
Beyond structural frameworks, specific enabling factors have been identified as critical for sustaining One Health collaborations. Evidence from systematic reviews indicates that the existence of a reference framework document for One Health activities, good coordination between different sectors at various levels, and joint multisectoral meetings that advocate the One Health approach significantly enhance collaborative success [70]. Furthermore, the availability of dedicated funds and adequate resources coupled with the support of technical and financial partners is a fundamental enabler [70].
Funding strategies that create incentive structures through joint budgets or special grants for One Health activities are particularly effective in promoting collaboration [68]. These mechanisms directly address the systemic barrier of siloed funding by creating shared resources that necessitate cooperative planning and implementation. Additionally, research networks and collaborations that incentivize knowledge exchange facilitate the cross-disciplinary dialogue essential for interpreting complex genomic data across human, animal, and environmental health contexts [68].
Technical Implementation: Genomic Surveillance in a One Health Framework
Integrated Genomic Surveillance Framework for AMR
The application of genomics within a One Health framework is particularly advanced in antimicrobial resistance (AMR) surveillance, providing a model for other collaborative genomic research areas. An integrated genomic framework combines isolate-based whole-genome sequencing (WGS) with shotgun metagenomics within a cohesive One Health strategy [71]. The following workflow illustrates this integrated approach:
Diagram 2: Integrated Genomic AMR Surveillance Workflow. This framework combines isolate-based WGS and metagenomics across One Health sectors for comprehensive resistance monitoring [71].
Technical Considerations for Genomic AMR Surveillance
The reliability of genomic AMR surveillance depends on well-defined sequencing protocols, encompassing sample processing, sequencing methodology, and bioinformatics workflows [71]. Standardizing these technical elements is critical for cross-sectoral comparability and data integration.
Table 2: Technical Specifications for Genomic AMR Surveillance
| Technical Element | Isolate-Based WGS | Shotgun Metagenomics |
|---|---|---|
| Primary Application | High-resolution characterization of priority pathogens and MDR/XDR strains [71]. | Analysis of complex microbial communities and unculturable bacteria from diverse reservoirs [71]. |
| Sample Requirements | High-quality genomic DNA from bacterial isolates [71]. | Optimized DNA extraction from complex environmental samples [71]. |
| Sequencing Platforms | Short-read (Illumina) for SNP detection; Long-read (Oxford Nanopore, PacBio) for complete assemblies [71]. | Short-read for affordable characterization; Long-read for mobile genetic element detection [71]. |
| Sequencing Depth | ≥100× coverage for SNP detection and outbreak investigations; 30-50× for broader surveillance [71]. | Balance sensitivity for rare resistance genes with financial feasibility [71]. |
| Bioinformatics Pipeline | Standardized pipelines for ARG annotation, strain typing, phylogenetic analysis [71]. | Harmonized workflows for resistome characterization, virulence factor annotation [71]. |
| Data Integration | Integration with global AMR databases (NCBI, Pathogenwatch, ResFinder) [71]. | Cross-sectoral comparability through standardized data-sharing protocols [71]. |
Research Reagent Solutions for One Health Genomics
Implementing the technical workflows for One Health genomic surveillance requires specific research reagents and materials. The following table details essential solutions for integrated AMR monitoring:
Table 3: Key Research Reagent Solutions for One Health Genomic Surveillance
| Reagent/Material | Function | Application Context |
|---|---|---|
| High-Fidelity DNA Polymerases | Ensure accurate amplification with minimal errors during library preparation [71]. | Critical for both WGS and metagenomic sequencing across all sectors. |
| Metagenomic DNA Extraction Kits | Optimized for diverse sample matrices (soil, water, feces) to maximize yield and representativeness [71]. | Essential for environmental and animal reservoir sampling where inhibitor removal is challenging. |
| Targeted Enrichment Panels | Capture specific resistance genes or pathogens from complex samples [71]. | Screening for known high-priority ARGs in surveillance programs. |
| Standardized Assembly Algorithms | Unified bioinformatics tools for genome reconstruction and annotation [71]. | Enabling cross-laboratory and cross-sector comparability of genomic data. |
| Curated ARG Databases | Reference databases for consistent annotation of resistance determinants [71]. | Harmonizing gene nomenclature across human, animal, and environmental health sectors. |
| Platform-Specific Library Prep Kits | Tailored reagents for different sequencing technologies (Illumina, Nanopore, PacBio) [71]. | Ensuring compatibility with the specific sequencing infrastructure available across sectors. |
Breaking down silos in One Health genomic research requires both technical and relational foundations. The strategies outlined in this guide—from establishing formal governance structures and implementing structured collaboration frameworks to standardizing technical protocols—provide a roadmap for researchers, scientists, and drug development professionals to overcome disciplinary and sectoral boundaries. The integrated genomic surveillance framework for AMR demonstrates the powerful insights achievable when human, animal, and environmental health sectors collaborate effectively, combining isolate-based WGS with metagenomics to track resistance dynamics across ecosystems [71].
Ultimately, successful multi-sectoral collaboration in genomic sciences requires a fundamental shift in perspective—recognizing that results and breakthroughs will not be achieved within single institutions or organizations but will be shared among One Health programs [68]. This paradigm change, supported by enabling funding structures, standardized technical protocols, and formal coordination mechanisms, promises to unlock the full potential of genomics to address complex global health challenges. By deliberately implementing these strategies, the scientific community can transform One Health from a conceptual framework into an operational reality, fostering a more resilient and integrated approach to health security in an interconnected world.
Building Capacity and Ensuring Equity in Genomic Technology Access
Genomic technologies are revolutionizing disease understanding and therapeutic development, yet their benefits remain unevenly distributed. Achieving equitable access and building sustainable capacity represents both an ethical imperative and a practical necessity for maximizing scientific progress. This is particularly true within a One Health framework, which recognizes the profound interconnections between human, animal, and environmental health. Pathogen surveillance, zoonotic disease tracking, and ecosystem monitoring all depend on robust, distributed genomic capabilities. When genomic capacity is concentrated in only a few well-resourced regions, it creates blind spots in our global health defense system, allowing emerging threats to go undetected and unaddressed. This whitepaper provides a technical guide for researchers and drug development professionals to implement practical strategies that build genomic capacity and ensure equity, thereby strengthening our collective ability to address health challenges across species and ecosystems.
Current Landscape and Disparities in Genomic Access
The integration of genomic technologies into healthcare and research has unveiled significant disparities in access and implementation. A 2024 review of international genomic health policies found that while the core concept of "access" is frequently cited, other critical components of equity—such as cultural responsiveness, non-discrimination, and community participation—are covered to a much lesser degree [73]. The analysis revealed a complete absence of policy addressing the concepts of "liberty" and "entitlement" in genomic care, highlighting a significant gap in the foundational equity framework [73].
These policy shortcomings manifest in concrete ways. In genomic research, nearly 95% of genomic data is derived from European ancestral populations, creating a massive "data equity problem" that undermines the generalizability and effectiveness of precision medicine across all populations [74]. Furthermore, racial and ethnic minorities, Indigenous communities, and rural residents consistently demonstrate less access to genetics health services, a disparity that persists even when demand exists [73] [75]. For instance, Indigenous Australians are three-fold underrepresented in clinical genetic services despite a clear need [73].
Table 1: Key Disparities in Genomic Technology Access
| Disparity Dimension | Key Findings | Implications |
|---|---|---|
| Genomic Data Composition | 95% of genomic data from European ancestral populations [74] | Reduced diagnostic accuracy, ineffective therapies for underrepresented groups |
| Geographic Access | Limited access in rural/underserved areas; services concentrated at major hospitals [75] [74] | Delayed diagnoses, prolonged "diagnostic odyssey" |
| Racial/Ethnic Equity | Under-representation of minority groups in genetic services [73] [74]; Structural racism in NICU care [76] | Widening health disparities, perpetuation of historical inequities |
| Workforce Distribution | Shortage of skilled professionals (bioinformaticians, genetic counselors) creates implementation bottlenecks [77] | Limited capacity to integrate genomics into routine care |
Building Technical and Workforce Capacity
A capable workforce is the cornerstone of genomic capacity. However, a significant shortage of skilled professionals—including bioinformaticians, genetic counselors, clinical geneticists, and data analysts—creates critical bottlenecks in implementing genomic programs, even in high-growth regions [77]. Addressing this requires a multi-faceted approach.
Workforce Development Initiatives
Strategic investments in education and training are paramount. The National Institutes of Health (NIH) has funded the Diversity Centers for Genome Research Consortium to directly address the need for workforce diversity and research capacity building [78]. This initiative employs common data elements (CDEs) to capture evaluation outputs, synergize reporting, and facilitate continuous quality improvement. The five CDEs focus on: genomics programs and equipment, scientific productivity, scientific collaboration, community engagement, and workforce development [78].
Simultaneously, building capacity within the existing primary care workforce is essential for mainstreaming genomics. A 2025 scoping review identified that the most significant barriers for primary care practitioners (PCPs) are knowledge gaps, environmental context and resources, and skills deficiencies [79]. The review recommends multifaceted, evidence-based education strategies with interactive components to change practitioner behavior, alongside a clear clarification of PCPs' roles and referral pathways to tertiary genetics services [79].
Experimental Protocol: A Model for Workforce-Integrated Research
The following protocol outlines a methodology for embedding capacity building within a genomic research study, aligning with the One Health principle of sustainable system strengthening.
Protocol Title: Integrated Workflow for Equitable Genomic Diagnosis and Workforce Training
Objective: To establish a replicable model for providing rapid genomic testing while simultaneously training a multidisciplinary clinical and bioinformatics workforce in underserved settings.
Materials and Reagent Solutions:
- Sequencing Platform: Illumina NovaSeq X or similar high-throughput sequencer [80]
- Analysis Software: Cloud-based genomic analysis platform (e.g., Amazon Web Services, Google Cloud Genomics) [80]
- Variant Calling Tool: AI-powered variant caller (e.g., DeepVariant) [80]
- Bioinformatics Reagents: Standardized bioinformatics pipelines for alignment (e.g., BWA), variant calling (e.g., GATK), and annotation (e.g., ANNOVAR).
- Telehealth Platform: Secure, HIPAA/GDPR-compliant video conferencing and data-sharing system [75].
Methodology:
- Project Establishment: Form a collaborative hub involving an academic genomics center, a clinical site in an underserved region, and a bioinformatics training institution.
- Needs Assessment: Conduct a joint assessment to identify specific clinical needs (e.g., diagnosis of rare diseases in a NICU [76]) and local workforce skill gaps.
- Customized Training: Develop and deploy a curriculum covering sample collection, library preparation, basic sequencing principles, data interpretation, and patient counseling, tailored to the roles of local practitioners, genetic counselors, and nascent bioinformaticians.
- Implementation with Tele-mentoring: Begin a clinical sequencing program (e.g., using rGS for critically ill newborns [76]) with real-time tele-mentoring from the academic partner. This includes virtual consenting, telegenetic consultations, and joint case reviews [75].
- Data Analysis Rotation: Local bioinformatics trainees complete rotations analyzing the project's genomic data on cloud platforms, supported by senior bioinformaticians.
- Continuous Evaluation: Use the NIH CDE framework [78] to track outcomes, including diagnostic yield, number of personnel trained, proficiency gains, and program sustainability.
This protocol creates a positive feedback loop: the clinical need drives the research activity, which in turn creates a authentic training environment that builds lasting local capacity.
Diagram 1: Integrated Capacity Building Workflow. This model shows how training and service delivery are synergized to create a sustainable local genomic ecosystem.
Innovative Frameworks for Ensuring Equity
Moving beyond theoretical commitment to practical action requires innovative service-delivery models and technologies designed specifically for equity.
The SeqFirst Model: Genotype-Driven Workflows
The SeqFirst-neo program provides a powerful experimental model for centering equity at the point of care [76]. This research initiative tested a genotype-driven workflow using simple, broad exclusion criteria for rapid genome sequencing (rGS) in a neonatal intensive care unit (NICU), rather than complex clinical inclusion criteria that often incorporate unconscious bias.
Experimental Protocol:
- Objective: To test whether a genotype-first workflow with simple exclusion criteria increases access to a precise genetic diagnosis (PrGD) in critically ill newborns, particularly among non-White populations [76].
- Intervention: All 408 newborns admitted to the NICU over 13 months were assessed. The exclusion criteria were minimal: corrected age >6 months or findings fully explained by physical trauma, infection, or complications of prematurity. Of 240 eligible infants, 126 were offered rGS (Intervention Group, IG) and compared to 114 who received conventional care (Conventional Care Group, CCG) [76].
- Results: A PrGD was made in 49.2% (62/126) of IG neonates compared to 9.7% (11/114) in the CCG. The odds of receiving a PrGD were approximately 9 times greater in the IG. Most significantly, access disparities were reduced: the PrGD rate for non-White infants was 45.9% (34/74) in the IG versus 20.7% (6/29) in the CCG, and for Black infants, it was 80.0% (8/10) in the IG versus 0% (0/4) in the CCG [76].
- Conclusion: Replacing complex, phenotype-first screening with simple, broad eligibility for genomic testing significantly increases diagnostic yield and improves equity by reducing reliance on clinician suspicion, which is often less accurate for non-White infants [76].
Technological and Care Model Innovations
Other innovative strategies are emerging to bridge the equity gap:
- Telegenetics and Telemedicine: The use of telegenetics services can dramatically expand access to genetic specialists for rural and underserved communities [75]. Successful models include virtual consultations, remote consenting processes, and self-guided return of results, which overcome geographic and specialist-maldistribution barriers [76] [75].
- Community Engagement and Capacity Building: True equity requires a "multi-directional transfer of knowledge" [81]. This involves early and sustained engagement with underserved communities as partners in research. Focus groups in Central Harlem identified that community decisions to participate in genomic biobanking were influenced by the potential contribution to community health, the broader societal context of science (e.g., DNA databases), and the researchers' tangible commitment to community health outcomes [81].
- Data Equity Initiatives: Projects like the Texome Project and partnerships with the Undiagnosed Diseases Network (UDN) actively work to bridge disparities. The Texome Project provides expert genetic evaluations and whole exome sequencing to underserved populations in Texas, with a commitment to reanalyzing data over two years to find answers [74]. The UDN refines its demographic data collection to understand and address the disease burden in underrepresented populations [74].
Table 2: Analysis of Innovative Equity-Focused Genomic Models
| Model Name | Core Innovation | Key Outcome | One Health Relevance |
|---|---|---|---|
| SeqFirst-neo [76] | Genotype-first workflow with simple exclusion criteria | 9x greater odds of diagnosis; eliminated diagnostic disparity for Black infants | Standardized triage can be adapted for animal disease surveillance and environmental pathogen monitoring. |
| Telegenetics [75] | Virtual delivery of genetic services | Improved access for rural/underserved populations; effective remote counseling | Enables expert consultation across vast geographic distances, crucial for veterinary care and ecosystem management. |
| Texome Project [74] | Proactive provision of comprehensive genetic services to underserved populations | Increased access to WES and long-term follow-up for underrepresented groups | Demonstrates a proactive, system-based approach to closing equity gaps, a model for inclusive planetary health surveillance. |
| Capacity Building Framework [81] [79] | Community and practitioner engagement as a core research component | Builds trust, enhances recruitment, improves PCP genomic capability | Builds resilient, distributed health networks capable of responding to cross-species health threats. |
Diagram 2: Contrasting Genomic Testing Workflows. The shift from a phenotype-first to a genotype-first model is fundamental to reducing bias and achieving equity.
The Scientist's Toolkit: Essential Reagents and Technologies
Table 3: Research Reagent Solutions for Equitable Genomic Capacity
| Tool Category | Specific Technology/Reagent | Function in Equitable Capacity Building |
|---|---|---|
| Sequencing Platforms | Oxford Nanopore portable sequencers [80] | Enables real-time, in-field sequencing for remote labs and pathogen surveillance, decentralizing capability. |
| Sequencing Platforms | Ultima Genomics UG 100 [80] | Drives down cost-per-base, making large-scale studies and population screening more economically feasible. |
| Bioinformatics Tools | Cloud Computing (AWS, Google Cloud) [80] | Provides scalable, cost-effective data storage and analysis, removing the need for expensive local computing infrastructure. |
| Bioinformatics Tools | AI/ML Tools (e.g., DeepVariant) [80] | Automates and improves accuracy of variant calling, reducing dependency on highly specialized expert labor. |
| Diagnostic Kits | Whole Exome/Genome Sequencing Kits [74] | Provides comprehensive, hypothesis-free testing, crucial for diagnosing conditions with non-specific presentations across diverse populations. |
| Collaborative Frameworks | Common Data Elements (CDEs) [78] | Standardizes evaluation metrics across capacity-building projects, enabling synergy and comparative learning. |
Building capacity and ensuring equity in genomic technology is not merely an ethical adjunct to scientific progress; it is a fundamental component of robust, reproducible, and effective science. The strategies outlined—from workforce development and policy reform to the implementation of genotype-first workflows and telegenetics—provide a roadmap for creating a more inclusive genomic future. For the One Health community, these efforts are particularly critical. The threats of pandemics, antimicrobial resistance, and environmental change do not respect national or socioeconomic boundaries. A distributed, equitable global genomic infrastructure is our best defense, allowing for early detection and rapid response to health challenges at the human-animal-environment interface. By investing in the frameworks, technologies, and trained personnel needed to extend genomic capabilities to all corners of the world, we are not only leveling the playing field for human health but also fortifying our collective resilience against the complex health challenges of the 21st century.
The FAIR Guiding Principles—Findable, Accessible, Interoperable, and Reusable—represent a foundational framework for scientific data management and stewardship that has gained significant traction since their formal publication in 2016 [82]. These principles were specifically designed to address the challenges posed by the increasing volume, complexity, and creation speed of data in modern research ecosystems [82]. The core innovation of FAIR lies in its emphasis on machine-actionability, enabling computational systems to find, access, interoperate, and reuse data with minimal human intervention [83]. This characteristic makes FAIR particularly crucial for data-intensive fields like genomic sciences, where the scale of data often exceeds human processing capabilities.
Within the context of One Health—an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals, and ecosystems [1]—the FAIR principles provide an essential framework for overcoming data fragmentation across sectors. The One Health approach recognizes that the health of humans, domestic and wild animals, plants, and the wider environment are closely linked and interdependent [1]. This interconnectedness generates complex, multidisciplinary data streams that require sophisticated integration methods to be meaningful for research and public health decision-making. The Digital One Health (DOH) framework has emerged as a response to this challenge, proposing a structured approach to data integration that aligns closely with FAIR objectives [84].
The convergence of FAIR principles with One Health approaches in genomic research creates a powerful paradigm for addressing pressing global challenges such as infectious diseases, antimicrobial resistance, and food safety [1]. This technical guide explores the implementation of FAIR data principles within One Health-oriented genomic sciences, providing researchers with practical methodologies, visualization tools, and standardized protocols to enhance data quality, interoperability, and reuse across disciplinary boundaries.
Core Components of the FAIR Principles
The Four FAIR Pillars
The FAIR principles are organized into four distinct but interconnected pillars, each addressing specific aspects of data management:
Findable: The initial step in (re)using data is its discovery. To enhance findability, both metadata and data should be easily discoverable by humans and computers alike [82]. This requires that (meta)data are assigned globally unique and persistent identifiers, described with rich metadata, and registered or indexed in searchable resources [83]. Machine-readable metadata is particularly crucial for enabling automatic discovery of datasets and services [82].
Accessible: Once identified, users must understand how data can be accessed. FAIR stipulates that (meta)data should be retrievable by their identifier using a standardized communications protocol that is open, free, and universally implementable [83]. Importantly, metadata should remain accessible even when the corresponding data is no longer available, preserving the record of what once existed [83].
Interoperable: Effective data integration requires that data can operate with applications or workflows for analysis, storage, and processing [82]. Interoperability is achieved through the use of formal, accessible, shared languages for knowledge representation, vocabularies that follow FAIR principles themselves, and qualified references to other (meta)data [83]. This pillar enables the merging of diverse datasets from human, animal, and environmental domains within the One Health framework.
Reusable: The ultimate objective of FAIR is to optimize data reuse [82]. Reusability depends on rich description of data with a plurality of accurate and relevant attributes, clear usage licenses, detailed provenance, and adherence to domain-relevant community standards [83]. This ensures that data can be replicated and/or combined in different settings by different researchers.
FAIR Principles Specification
Table 1: Detailed breakdown of the FAIR principles and their implementation considerations.
| FAIR Pillar | Principle Code | Principle Statement | Key Implementation Considerations |
|---|---|---|---|
| Findable | F1 | (Meta)data are assigned a globally unique and persistent identifier | Use of DOIs, ARKs, or other persistent ID systems; resolution through identifier services |
| F2 | Data are described with rich metadata | Metadata richness follows community standards; multiple attribution elements | |
| F3 | Metadata clearly and explicitly include the identifier of the data they describe | Bidirectional linking between data and metadata; unambiguous association | |
| F4 | (Meta)data are registered or indexed in a searchable resource | Deployment in discoverable repositories; indexing by specialized data search engines | |
| Accessible | A1 | (Meta)data are retrievable by their identifier using a standardized communications protocol | HTTP(S) implementation; possible authentication/authorization mechanisms |
| A1.1 | The protocol is open, free, and universally implementable | No proprietary barriers; community-vetted standards | |
| A1.2 | The protocol allows for an authentication and authorization procedure, where necessary | Access control without compromising discoverability; tiered access when appropriate | |
| A2 | Metadata are accessible, even when the data are no longer available | Preservation commitment; metadata persistence policies | |
| Interoperable | I1 | (Meta)data use a formal, accessible, shared, and broadly applicable language for knowledge representation | Standardized data models; formal semantics; machine-readable formats |
| I2 | (Meta)data use vocabularies that follow FAIR principles | Use of community standards like SNOMED CT, MeSH [85]; ontology utilization | |
| I3 | (Meta)data include qualified references to other (meta)data | Relationship specification; contextual linking; cross-repository references | |
| Reusable | R1 | (Meta)data are richly described with a plurality of accurate and relevant attributes | Comprehensive documentation; multiple descriptive dimensions |
| R1.1 | (Meta)data are released with a clear and accessible data usage license | Standard license formats (CC0, CC-BY, etc.); machine-readable license statements | |
| R1.2 | (Meta)data are associated with detailed provenance | Origin tracking; processing history; transformation documentation | |
| R1.3 | (Meta)data meet domain-relevant community standards | Adherence to field-specific metadata schemas; participation in standards development |
The One Health Context and Data Challenges
One Health Approach and Digital Integration Needs
The One Health approach is defined by the World Health Organization as "an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems" [1]. This approach recognizes the intimate connections between human health, animal health, and environmental factors, particularly in the context of emerging infectious diseases, antimicrobial resistance, and food safety [1]. The COVID-19 pandemic has dramatically underscored the necessity of strengthening One Health implementation, with particular emphasis on connections to the environment [1].
The Digital One Health (DOH) framework has been proposed to address the significant gaps in current data integration practices [84]. This framework is structured around five key pillars: (a) harmonization of standards to establish trust, (b) automation of data capture to enhance quality and efficiency, (c) integration of data at point of capture to limit bureaucracy, (d) onboard data analysis to articulate utility, and (e) archiving and governance to safeguard the OH data resource [84]. These pillars align closely with FAIR principles and provide a practical implementation pathway for One Health data integration.
Current implementations of One Health often focus on multi-sectoral collaboration but frequently overlook opportunities to integrate contextual and pathogen-related data into a unified data resource [84]. This lack of integration hampers effective, data-driven decision-making in One Health activities [84]. The DOH framework aims to leverage technology to create data as a shared resource, overcoming not only current structural barriers but also addressing prevailing ethical and legal concerns [84].
Genomic Data Integration Challenges in Healthcare Ecosystems
The integration of genomic data into clinical and public health workflows presents distinctive challenges within the One Health framework. A 2025 systematic review highlighted that fragmented data ecosystems disrupt interoperability, complicate patient-centered care, and present significant challenges for incorporating genomic data into clinical workflows [86]. Key challenges identified include:
- Semantic misalignment across commonly used healthcare standards such as HL7 FHIR and SNOMED CT [86]
- Limited cross-system data exchange capabilities between human health, veterinary, and environmental monitoring systems
- Inadequate patient engagement features in Electronic Health Records (EHRs) for capturing and utilizing genomic information
- Security and clinical utility concerns regarding genomic data, particularly in cross-border and cross-sectoral sharing scenarios [86]
The systematic review, which analyzed 161 studies, found that interoperability remains a cornerstone challenge for modern healthcare systems, requiring well-defined strategies for structuring, managing, and securely exchanging diverse health data [86]. This is particularly critical for chronic disease management, where effective data sharing ensures timely, high-quality healthcare [86]. Without robust interoperability frameworks, fragmented systems lead to redundant efforts and delayed treatments, ultimately adversely affecting patient outcomes [86].
Implementing FAIR Principles in One Health Genomic Research
FAIRification Framework and Methodology
The FAIRification process refers to the practical implementation of FAIR principles onto data resources. A practical "how to" guidance to go FAIR can be found in the Three-point FAIRification Framework [82]. This process typically involves the following key stages:
Pre-FAIRification Assessment: Evaluate the current state of data resources against FAIR principles using maturity models or assessment tools. This establishes a baseline and identifies priority areas for improvement.
Data Model Alignment: Map existing data structures to formal models, ontologies, and vocabularies that comply with FAIR principles, particularly addressing the Interoperable and Reusable pillars.
Identifier Implementation: Assign globally unique and persistent identifiers to datasets and key metadata elements, supporting the Findability principles.
Metadata Enhancement: Enrich metadata descriptions to meet domain-relevant community standards, ensuring comprehensive coverage of the Reusable principles.
Infrastructure Deployment: Establish or leverage trusted repositories that support FAIR access patterns, including standardized protocols and authentication/authorization where required.
Provenance Tracking: Implement systems to record data origin, processing history, and transformations, addressing the Reusable principle R1.2.
License Clarification: Attach clear, machine-readable usage licenses to enable reuse while respecting ethical and legal constraints.
The European Union's open data portal provides an exemplary case study of FAIR implementation, demonstrating how data quality guidelines can be operationalized at scale [87]. Similarly, the AnaEE (Analysis and Experimentation on Ecosystems) Research Infrastructure offers insights into achieving semantic interoperability in ecosystem studies [88], a critical concern for the environmental health component of One Health.
Workflow for FAIR Data Generation in One Health Genomics
The following diagram illustrates the integrated workflow for generating FAIR-compliant genomic data within a One Health context, connecting human, animal, and environmental data streams:
Diagram 1: FAIRification workflow for One Health genomic data integration
Semantic Interoperability Framework
Achieving semantic interoperability across human, animal, and environmental genomic data requires a structured approach to vocabulary alignment and data modeling. The following diagram illustrates the semantic interoperability framework essential for FAIR-compliant One Health data:
Diagram 2: Semantic interoperability framework for cross-domain One Health data
Experimental Protocols and Methodologies
Standardized Protocol for FAIR Genomic Data Generation
This protocol outlines a standardized methodology for generating FAIR-compliant genomic data within a One Health research context, incorporating elements from the "Genomics Applied to One Health" training course [89] and best practices from genomic data repositories.
Sample Collection and Metadata Documentation
Objective: To collect human, animal, and environmental samples with comprehensive metadata capture ensuring traceability and future reuse.
Materials:
- Sample collection kits with unique pre-printed identifiers
- Mobile data capture application with offline capability
- Standardized metadata forms aligned with relevant community standards
- Barcoded storage containers
Procedure:
- Assign persistent unique identifier to each sample at collection point
- Record core metadata elements:
- Geographic coordinates (using decimal degrees format)
- Date and time of collection
- Collector information
- Sample type and preservation method
- Document contextual information:
- Human subjects: demographic and clinical data using HL7 FHIR standards
- Animal sources: species identification using NCBI Taxonomy IDs, health status
- Environmental matrices: physical-chemical parameters, collection method
- Implement chain-of-custody documentation using blockchain-based provenance tracking where required for sensitive data [86]
- Transfer samples to laboratory under appropriate storage conditions
Library Preparation and Sequencing
Objective: To generate genomic sequencing data with complete technical metadata following FAIR principles.
Materials:
- Library preparation kits (e.g., Illumina, Nanopore)
- Unique dual indexes to prevent sample cross-talk
- MinION Nanopore platform for field sequencing [89]
- Laboratory information management system (LIMS) with API access
Procedure:
- Extract nucleic acids using documented protocols
- Assess quality metrics (e.g., DIN for DNA, RIN for RNA)
- Prepare sequencing libraries using standardized workflows
- Record kit lot numbers and version information
- Document fragmentation parameters and size selection criteria
- Assign unique library identifiers linked to sample identifiers
- Perform sequencing on appropriate platform
- Record platform-specific run parameters
- Include control samples for quality monitoring
- Generate raw data in standard formats (FASTQ, BCL)
Bioinformatics Processing and Data Annotation
Primary Analysis and Quality Control
Objective: To process raw sequencing data into analysis-ready formats with comprehensive quality assessment.
Computational Tools:
- FastQC for quality control assessment
- MultiQC for aggregated quality reporting
- Trimmomatic or Cutadapt for adapter removal
- BWA-MEM2 or Bowtie2 for alignment to reference genomes
- GATK best practices for variant calling
Procedure:
- Process raw data through standardized computational workflows
- Document all software tools with version information and parameters
- Generate quality metrics for each processing step
- Create intermediate files in community-standard formats (BAM, VCF)
- Assign unique analysis identifiers to processed datasets
- Link analysis identifiers to raw data through provenance chains
Functional Annotation and Metadata Enhancement
Objective: To add biological context to genomic data using standardized ontologies and vocabularies.
Resources:
- Specialized databases (EupathDB, WormBaseParasiteDB) [89]
- Reference ontologies (GO, SO, OBI)
- Domain-specific metadata standards (MIxS, GSC)
Procedure:
- Annotate genomic features using controlled vocabularies
- Map sample metadata to community-standard checklists
- Include geospatial annotation using gazetteer references
- Document analysis methods using the OBI ontology
- Generate data files in standardized formats (GFF, GTF)
Research Reagent Solutions for One Health Genomics
Table 2: Essential research reagents and computational tools for FAIR-compliant One Health genomic research.
| Category | Item/Resource | Specification/Function | FAIR Alignment |
|---|---|---|---|
| Sample Collection | Barcoded Collection Kits | Unique sample identification at source | Supports F1 (persistent identifiers) and R1.2 (provenance) |
| Mobile Data Capture Apps | Field metadata documentation with offline capability | Enhances R1 (rich metadata) and A1 (accessible protocol) | |
| Sequencing | MinION Nanopore Platform | Portable sequencing for field deployment [89] | Enables A1.1 (open protocol) and I1 (standard formats) |
| Unique Dual Indexes | Multiplexing without sample cross-talk | Ensures R1.2 (provenance) and data quality for reuse | |
| Bioinformatics | EupathDB Databases | Specialized functional annotation [89] | Provides I2 (FAIR vocabularies) and R1.3 (community standards) |
| CF Conventions | Standardized environmental data representation [87] | Enables I1 (formal language) across environmental domains | |
| Data Repository | Dataverse Software | Repository platform for data stations [88] | Supports F4 (searchable resource) and A1 (access protocol) |
| Zenodo/Figshare | General-purpose FAIR-compliant repositories | Provides persistent identifiers (F1) and standardized access (A1) | |
| Ontology Services | OBO Foundry Ontologies | Interoperable biomedical ontologies | Delivers I2 (FAIR vocabularies) and I1 (formal language) |
| ROR Registry | Organization identifier service [88] | Enables F1 (persistent IDs) for institutional attribution |
Implementation Case Studies and Quantitative Assessment
FAIR Implementation in High-Energy Physics and Earth Sciences
Case studies from data-intensive scientific communities demonstrate the practical implementation and benefits of FAIR principles. The high-energy physics community has developed FAIR frameworks for AI-ready datasets, creating standardized resources such as the FAIR and AI-ready Higgs boson decay dataset [87]. This initiative exemplifies how FAIR principles can be applied to complex experimental data to enhance reuse and computational analysis.
Similarly, the Earth sciences community has implemented FAIR principles in critical resources like the IPCC WGI AR6 Atlas repository [87]. This implementation showcases the importance of standardized metadata and structured data formats for supporting international climate assessments. The use of CF (Climate and Forecast) metadata conventions demonstrates how community standards enable interoperability across diverse datasets and research groups [87].
The European Union's open data portal provides another instructive case study, having developed comprehensive data quality guidelines to enhance the FAIRness of its extensive data resources [87]. These guidelines operationalize FAIR principles at scale, addressing practical concerns of data management, documentation, and access.
Quantitative FAIR Assessment Metrics
Table 3: Quantitative metrics for assessing FAIR principle implementation in genomic data resources.
| FAIR Principle | Metric Category | Specific Measurable Indicators | Target Performance Level |
|---|---|---|---|
| Findable | Identifier Implementation | Percentage of datasets with persistent identifiers | 100% assignment at creation |
| Metadata Richness | Number of metadata elements per dataset | Minimum 20 core elements | |
| Search Performance | Search result relevance score | >80% precision in retrieval | |
| Accessible | Protocol Compliance | HTTP/S implementation success rate | 100% protocol adherence |
| Availability | Repository uptime percentage | >99.5% availability | |
| Authentication | Tiered access implementation capability | Support for multiple auth methods | |
| Interoperable | Standard Adoption | Use of community metadata standards | 100% alignment with domain schemas |
| Vocabulary Use | Percentage of annotations using controlled terms | >90% terminology standardization | |
| Format Compliance | Support for standard data formats | Minimum 3 standard formats | |
| Reusable | License Clarity | Presence of machine-readable license | 100% license assignment |
| Provenance Detail | Completeness of provenance documentation | Full chain from sample to data | |
| Citation Performance | Number of third-party citations | Increasing annual citation rate |
The implementation of FAIR principles within One Health genomic research represents a critical enabling strategy for addressing complex health challenges at the human-animal-environment interface. As demonstrated by the frameworks, protocols, and case studies presented in this technical guide, the systematic application of FAIR principles enhances data discovery, integration, and reuse across traditional disciplinary boundaries. The Digital One Health framework [84] provides a particularly promising approach for operationalizing FAIR principles at scale, addressing both technical and governance challenges in multi-sectoral data sharing.
Future developments in this field will likely focus on several key areas:
- AI and machine learning readiness of FAIR datasets, enabling more sophisticated analytical approaches to One Health challenges [87]
- Enhanced semantic interoperability through the development and adoption of cross-domain ontologies and vocabulary services
- Automated FAIR assessment tools that can provide real-time feedback on data FAIRness
- Blockchain-based provenance tracking for sensitive data requiring detailed governance [86]
- Expanded implementation of the CARE Principles for Indigenous Data Governance, ensuring ethical engagement with Indigenous communities and their data [83]
The integration of FAIR principles with One Health approaches in genomic sciences will continue to evolve, driven by technological advancements and increasingly urgent needs for coordinated responses to global health challenges. By adopting the methodologies, standards, and best practices outlined in this guide, researchers can contribute to building more resilient, integrated, and effective data ecosystems for protecting and promoting health across species and ecosystems.
Developing Robust Pipelines and Quality Assurance for Genomic Surveillance
The One Health approach, which recognizes the interconnectedness of human, animal, and environmental health, is increasingly critical for managing disease threats in an era of globalization and climate change [20]. Genomic surveillance has become a foundational tool within this approach, enabling precise pathogen identification, real-time outbreak tracking, and insights into host-pathogen co-evolution [20]. Robust pipelines and stringent quality assurance are essential to transform raw genomic data into actionable intelligence for researchers, scientists, and drug development professionals. This technical guide outlines the core components, methodologies, and quality frameworks required to develop such pipelines, emphasizing their application across human, animal, and plant health domains to support a cohesive biosecurity strategy.
Core Components of a Genomic Surveillance Pipeline
A comprehensive genomic surveillance pipeline integrates wet-lab and computational processes, supported by cross-sectoral collaboration. The key technical domains that cut across all pipeline activities are Sampling and Sequencing, Data Processing and Analysis, Quality Assurance & Validation, and Evidence-to-Policy translation [20]. The table below summarizes the quantitative standards for the final data package.
Table 1: Quality Control Standards for Genomic Surveillance Data Submission [90]
| Component | Standard or Requirement | Purpose |
|---|---|---|
| Genome Sequence Data | Quality control (QC) assessment | Ensures data reliability for downstream analysis |
| Contextual Data | Validation of metadata | Confirms accuracy of associated sample data |
| Data Submission | Submission to public repository (e.g., via INSDC) | Facilitates data sharing and global surveillance |
| Data Access | Availability through custom dashboards (e.g., NCBI Pathogen Detection) | Enables cluster analysis and genotyping for public health decision-making |
| Data Curation | Ongoing maintenance of public data | Ensures long-term relevance and accuracy of shared data |
Sampling, Sequencing, and Data Generation
The initial phase focuses on generating high-quality genomic data. This involves systematic sample collection from humans, animals, plants, and the environment, reflecting the One Health scope [20]. High-throughput sequencing (HTS) technologies are deployed across various contexts, from central labs to field applications [20]. Specific protocols, such as those for bacterial whole-genome sequencing, involve genomic DNA isolation, quantification and purity measurement, DNA library preparation, and quality control of libraries prior to sequencing [91].
Data Processing, Analysis, and Integration
Following sequencing, data processing and analysis extract meaningful biological insights. This stage applies bioinformatics pipelines and computational tools for tasks like genome assembly, variant calling, and phylogenetic analysis [20]. A One Health approach requires integrating these genomic findings with epidemiological and environmental data, which presents challenges in data dispersion, heterogeneous collection methods, and semantic interoperability [36]. Successful integration allows for co-analysis, leading to new hypotheses and improved early warning systems for health events [36].
Quality Assurance and Validation Frameworks
Quality assurance is a cross-cutting technical domain that ensures data reliability, reproducibility, and compliance with accreditation frameworks [20]. This extends from technical data quality to the integrity of the entire data package submitted to public repositories.
Standards for Data Submission and Curation
Contributing to global surveillance requires assembling a standard data package. The process involves five key protocols [90]:
- Quality Control (QC) Assessment for Genome Sequence Data: Evaluating the raw and assembled sequence data to meet quality thresholds.
- Contextual Data Validation: Verifying the accuracy and completeness of associated metadata (e.g., host, location, date).
- Data Submission: Submitting the validated pathogen data package (Pathogen DOM) to an International Nucleotide Sequence Database Consortium (INSDC) member, such as the National Center for Biotechnology Information (NCBI).
- Data Access and Querying: Utilizing platforms like the NCBI Pathogen Detection dashboard to view data and access automated cluster analyses.
- Data Curation: Performing ongoing maintenance of public data to ensure its continued relevance and accuracy.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for wet-lab sequencing workflows in genomic surveillance.
Table 2: Key Research Reagent Solutions for Genomic Sequencing Workflows
| Item / Reagent | Function | Example Use Case |
|---|---|---|
| Nexttec 1-step Kit | Genomic DNA isolation from bacterial samples | Preparation of pure DNA template for sequencing [91] |
| Qubit Fluorometer | Accurate quantification of genomic DNA concentration | Ensures precise loading of DNA into sequencing library preparations [91] |
| Nanodrop Spectrophotometer | Measurement of genomic DNA purity (e.g., ratio of A260/A280) | Assesses sample quality and detects contaminants like salts or proteins [91] |
| NEBNext Ultra II FS DNA Kit | Preparation of DNA libraries for Illumina sequencing | Fragments, end-repairs, and adds adapters to DNA for sequencing [91] |
| Illumina MiSeq | Performing high-throughput whole-genome sequencing | Generates the raw sequence data (FASTQ files) for analysis [91] |
Operationalizing One Health through Collaborative Genomics
Moving from single-sector surveillance to an integrated One Health system requires multi-sector coordination at every stage, from sample collection to dissemination of results [36]. Initiatives like the Genomics for Animal and Plant Disease Consortium (GAP-DC) exemplify this by fostering collaboration between government agencies and academic institutions to tackle shared technological and policy challenges [20]. GAP-DC's work packages address critical areas such as frontline pathogen detection at borders, pathogen spillover at the wildlife-domestic interface, and management of both outbreak and endemic diseases [20]. This operational model emphasizes that beyond technical integration, successful One Health genomic surveillance requires complex partner identification, sustained engagement, co-development of system scope, and joint data analysis and interpretation across sectors [36].
Developing robust pipelines and quality assurance for genomic surveillance is a multidisciplinary endeavor fundamental to the One Health mission. It requires the integration of advanced technological capabilities, rigorous and standardized protocols, and a collaborative framework that transcends traditional sectoral boundaries. By adhering to stringent quality controls from sample to policy decision and leveraging integrated data systems, the scientific community can enhance disease detection, elucidate transmission dynamics, and ultimately strengthen global health security.
Measuring Impact: Evaluating the Success of One Health Genomic Systems
The increasing frequency and impact of emerging infectious diseases and antimicrobial resistance (AMR) have exposed critical vulnerabilities in global health security. Traditional disease surveillance systems, characterized by their sectoral independence and disciplinary isolation, struggle to provide the holistic insights needed to address complex health threats at the human-animal-environment interface [92]. The One Health approach recognizes that the health of humans, domestic animals, wildlife, and ecosystems are profoundly interconnected, and that effective public health responses require integrated, multisectoral coordination [93].
This paradigm shift is particularly evident in genomic sciences, where pathogen genome sequencing has transformed our ability to track disease transmission, understand pathogen evolution, and investigate outbreaks. One Health genomics represents a fundamental departure from traditional surveillance by integrating genomic data across human, animal, and environmental sectors, enabling researchers to unravel complex transmission dynamics that would otherwise remain invisible within disciplinary silos [11]. This technical guide provides a comprehensive comparative analysis of these contrasting approaches, examining their conceptual foundations, methodological frameworks, practical implementations, and impacts on public health decision-making.
Conceptual and Methodological Foundations
Traditional Siloed Surveillance: A Sector-Specific Approach
Traditional surveillance systems operate within well-established but isolated sectoral boundaries, with distinct data collection, analysis, and reporting mechanisms for human health, animal health, and environmental monitoring. This approach is characterized by independent data systems, sector-specific analysis platforms, and disciplinary visualizations that limit cross-sectoral insight [92].
The fundamental workflow in traditional surveillance follows a linear pathway within each sector: (1) sample or data collection; (2) data storage and aggregation; (3) data analysis and interpretation; and (4) dissemination or outcome communication [92]. While this model has demonstrated effectiveness for addressing sector-specific health concerns, it creates significant blind spots for understanding cross-sectoral health threats.
Key limitations of this approach include:
- Incomplete understanding of zoonotic transmission pathways and environmental reservoirs
- Delayed detection of emerging health threats at the human-animal-environment interface
- Fragmented data governance and sharing mechanisms across sectors
- Inconsistent informatics capacity ranging from paper-based systems to advanced digital infrastructure [92]
One Health Genomics: An Integrated Framework
One Health genomics represents a transformative approach that leverages pathogen genomic data as a universal language to track health threats across species and ecosystems. This methodology is grounded in the understanding that pathogen genomic data is host-agnostic, enabling researchers to reconstruct transmission networks and identify reservoirs without the constraints of sectoral boundaries [6].
The conceptual advancement of One Health genomics lies in its ability to connect seemingly unrelated health events through shared pathogen genomes, creating a unified understanding of disease ecology. This approach has been most successfully applied in foodborne disease surveillance through systems such as PulseNet, GenomeTrakr, and the European One Health Whole Genome Sequencing System [92].
The core innovation of One Health genomics is its capacity for phylogenetic analysis across sectors, which allows for the assessment of transmission dynamics at the human-animal-environment interface, enabling proactive prevention of One Health threats through early outbreak detection and reservoir identification [92].
Table 1: Fundamental Characteristics of Surveillance Approaches
| Characteristic | Traditional Siloed Surveillance | One Health Genomics |
|---|---|---|
| Conceptual Foundation | Sector-specific health protection | Interconnected health across domains |
| Data Structure | Independent, sector-specific databases | Integrated, cross-sectoral data platforms |
| Primary Focus | Human health OR animal health OR environmental health | Interface events and cross-domain transmission |
| Pathogen Understanding | Within-sector transmission dynamics | Cross-species transmission and evolution |
| Governance Model | Sector-specific mandates and policies | Cross-sectoral coordination mechanisms |
Technical Implementation and Data Integration
One Health Genomic Data Integration Frameworks
Implementing effective One Health genomic surveillance requires sophisticated data integration frameworks that can accommodate heterogeneous data sources while addressing complex governance challenges. Recent research has identified several promising approaches for achieving this integration [92].
A systematic framework developed for Washington State government emphasizes that successful One Health data integration must consider common challenges of limited resource settings, including lack of informatics support during planning phases, and the need to move beyond scoping and planning to actual system development, production, and joint analyses [92]. This framework highlights that One Health integration requires complex partner identification, engagement and co-development of system scope, complex data governance, and joint data analysis across sectors.
Table 2: Approaches to One Health Genomic Data Integration
| Approach | Key Features | Implementation Examples |
|---|---|---|
| Shared Secure Surveillance Platform | • Human, animal, environmental, and food isolates• Sequence data with associated metadata• Controlled data access• Automated data sharing with international repositories | Swiss surveillance platform between human and veterinary medicine [94] |
| Shared Bioinformatics Platform | • Common workflow system• Quality control processes• Integrated analysis of human, animal, food, and environmental isolates | Italian multisectoral data collection and bioinformatic analysis platform [94] |
| Federated Database Ecosystem | • Distributed databases connected through APIs• Maintained data sovereignty• Cross-database querying capabilities | Proposed federated solutions for sharing genomic data across jurisdictions [94] |
| Open Access Databases with Standardized Practices | • Store sequences with standardized metadata• Inclusion of specimens from all One Health domains• Clear processes for data correction and updating | Best practices for One Health contributions to international sequence databases [94] |
Workflow Architecture for One Health Genomics
The implementation of One Health genomic surveillance requires a structured workflow that encompasses sample collection, sequencing, data integration, and joint analysis across sectors. The following Graphviz diagram illustrates this integrated workflow:
One Health Genomics Workflow
Data Integration and Analytical Architecture
The computational backbone of One Health genomics requires robust bioinformatic infrastructure capable of handling massive genomic datasets while enabling cross-sectoral data integration. The following architecture supports this integration:
Data Integration Architecture
Performance and Outcome Comparison
Quantitative Comparison of Surveillance Capabilities
The transition from traditional siloed surveillance to integrated One Health genomics produces measurable differences across multiple performance dimensions. The table below summarizes key comparative metrics based on documented implementations and case studies:
Table 3: Performance Comparison of Surveillance Approaches
| Performance Metric | Traditional Siloed Surveillance | One Health Genomics |
|---|---|---|
| Outbreak Detection Speed | Delayed, often after significant human transmission | Early warning through integrated environmental and animal data |
| Transmission Insight | Limited to within-sector understanding | Cross-species transmission routes and reservoirs identified |
| Data Completeness | Fragmented, sector-specific data | Holistic view of health threats across domains |
| Resource Efficiency | Duplicative testing and analysis across sectors | Shared resources and infrastructure |
| Antimicrobial Resistance Tracking | Sector-specific resistance patterns | Comprehensive tracking from hospitals to livestock to environment |
| Response Coordination | Sector-specific response actions | Integrated, cross-sectoral public health interventions |
| Pandemic Preparedness | Reactive to human case emergence | Proactive detection in animal and environmental reservoirs |
Case Study Applications
Antimicrobial Resistance Surveillance
The global challenge of antimicrobial resistance (AMR) exemplifies the critical importance of One Health genomics. Between 2010 and 2015, total global antibiotic consumption increased by 65% from 21.1 to 34.8 billion defined daily doses, with the greatest increases in emerging economies [6]. The use of antimicrobials in livestock production comprises 73% of entire global consumption, currently estimated at 131,000 tons annually and predicted to rise to 200,000 tons by 2030 [6].
One Health genomics reveals that AMR is not confined to clinical settings but operates as a connected ecosystem. Whole genome sequencing enables researchers to track the movement of resistance genes between bacterial species and across human, animal, and environmental domains, identifying high-risk clones and mobile genetic elements that drive resistance dissemination [6]. This comprehensive understanding is essential for developing effective containment strategies.
Wastewater-Based Epidemiology
Wastewater surveillance has emerged as a powerful application of One Health genomics, particularly during the COVID-19 pandemic. Wastewater contains a broad range of chemicals and biota from human populations, providing a community-wide health snapshot [95]. The "one sample many analyses" (OSMA) approach allows for simultaneous detection of pathogens, AMR genes, and pharmaceutical residues, creating a cost-effective sentinel system for public health threats [95].
This approach enables non-invasive detection of community infection trends, including for non-notifiable pathogens, while also monitoring antimicrobial usage patterns through analytical chemistry techniques [95]. Wastewater's status as both a pollutant and data source makes it an ideal sentinel within the One Health toolkit, connecting human health with environmental monitoring.
Implementation Challenges and Technical Solutions
Bioinformatics and Computational Infrastructure
The implementation of One Health genomic surveillance faces significant computational challenges due to the enormous volume of data generated by modern sequencing technologies. It has been estimated that the annual acquisition of raw genomic data worldwide would exceed one zettabyte (one trillion GB) by 2025 [6]. This data deluge requires scalable computational infrastructures and sophisticated bioinformatic pipelines.
Key solutions to these challenges include:
- Cloud computing infrastructures that enable resource sharing and limit overprovisioning for peak loads
- Robust, reproducible analysis workflows that can scale from small case numbers to very large datasets
- Federated database ecosystems connected through APIs that maintain data sovereignty while enabling cross-sectoral querying [94]
- Automated pipelines for quality control, curation, standardization, and annotation of genomic data [94]
Tools like ASA3P (Automatic Bacterial Isolate Assembly, Annotation and Analyses Pipeline) represent the kind of automated, standardized bioinformatic solutions needed to make One Health genomics operationally feasible across diverse settings [6].
Research Reagent Solutions for One Health Genomics
Implementing effective One Health genomic surveillance requires specific technical reagents and computational tools. The following table details essential components and their functions:
Table 4: Essential Research Reagents and Tools for One Health Genomics
| Reagent/Tool Category | Specific Examples | Function in One Health Surveillance |
|---|---|---|
| Sequencing Technologies | Oxford Nanopore, Illumina | Generate genomic data from human, animal, and environmental samples |
| Bioinformatic Pipelines | ASA3P, Custom workflows | Process raw sequence data, perform assembly, annotation, and analysis |
| Database Infrastructure | APIs, Federated databases, Cloud storage | Enable cross-sectoral data sharing and integration |
| Quality Control Tools | QC thresholds, Standardization protocols | Ensure data quality and interoperability across diverse sample types |
| Computational Resources | Cloud computing, High-performance computing | Handle massive datasets and complex phylogenetic analyses |
| Visualization Platforms | Dashboards, Interactive tools | Present integrated data to support public health decision-making |
Future Directions and Implementation Recommendations
Based on the documented experiences and case studies of One Health genomic implementation, several key recommendations emerge for researchers and public health agencies:
Develop Modular, Scalable Bioinformatics Pipelines Implementation of open-source, accessible bioinformatics pipelines that can be adapted to local needs and resources is essential. These pipelines should be modular for flexibility, reproducible across computing environments, and capable of integrating diverse data types [94].
Strengthen Cross-Sectoral Data Governance Frameworks Successful One Health genomics requires navigating complex data governance challenges. Establishing clear agreements on data sharing protocols, access controls, and intellectual property while maintaining appropriate privacy protections is fundamental to building trust across sectors [92].
Build Technical Workforce Capacity The specialized skills required for One Health genomics—including bioinformatics, genomic epidemiology, and cross-sectoral collaboration—represent a critical capacity gap in many settings. Strategic investment in training programs, workforce development, and knowledge transfer is needed at national and global levels [94].
Implement Federated Data Systems Rather than centralizing all data, federated systems that connect distributed databases through APIs offer a practical approach to data integration while respecting jurisdictional boundaries and data sovereignty concerns [94].
Adopt "One Sample Many Analyses" Approaches Maximizing the value of surveillance samples through coordinated testing for multiple pathogens, AMR markers, and chemical indicators provides greater efficiency and more comprehensive health intelligence [95].
The transformative potential of One Health genomics lies in its ability to move beyond sectoral limitations and create a unified understanding of health threats. As genomic technologies become more accessible and bioinformatic tools more sophisticated, the implementation of integrated surveillance systems will be crucial for effective pandemic preparedness, antimicrobial resistance containment, and proactive management of emerging health threats at the human-animal-environment interface.
The One Health approach is an integrated, unifying framework that aims to sustainably balance and optimize the health of people, animals, and ecosystems, recognizing their close interdependence [1]. In the context of genomic sciences, this approach leverages advanced genomic surveillance technologies to mitigate threats posed by endemic and emerging diseases across agricultural, public health, and biosecurity domains [20]. The rationale for quantifying outcomes within this framework stems from the need to objectively evaluate performance in outbreak detection and response, strategically inform policies, and optimize resource allocation for maximum public health impact [96]. As the world continues to confront the aftermath of the COVID-19 pandemic, which led to the loss of millions of lives and trillions of dollars from the global economy, the imperative to strengthen One Health approaches with greater emphasis on genomic surveillance has never been clearer [1]. This technical guide provides researchers and drug development professionals with methodologies and metrics for rigorously evaluating the effectiveness, cost-benefit, and public health impact of One Health initiatives in genomic research.
Quantitative Frameworks for Measuring Effectiveness
Timeliness Metrics for Outbreak Detection and Response
A critical framework for quantifying the effectiveness of One Health systems involves analyzing timeliness metrics across multisectoral public health emergencies. These metrics objectively measure the time between key outbreak milestones, allowing for quantitative assessment of detection and response performance [96]. The One Health timeliness framework emphasizes cross-sectoral coordination and community engagement, analyzing metrics related to predictive alerts of outbreaks and preventive responses.
Table 1: One Health Timeliness Metrics and Milestones
| Metric Phase | Start Milestone | End Milestone | Performance Indicator |
|---|---|---|---|
| Detection | Outbreak Start | First Detection | Speed of initial identification |
| Notification | First Detection | Official Notification | Reporting efficiency |
| Verification | Official Notification | Verification | Case confirmation timeliness |
| Response Initiation | Verification | Response Implementation | Reaction rapidity |
Research from Uganda (2018-2022) demonstrates the practical application of these metrics, revealing that the greatest predictors of improved timeliness are (1) frequent past experience with similar disease outbreaks and (2) whether an outbreak is a viral hemorrhagic fever due to heightened perceived threat and pre-existing preparedness measures [96]. Diagnostic and laboratory considerations, along with contextual influences such as One Health collaborations, were also described as relevant to timeliness.
Genomic Surveillance Performance Indicators
Within the UK's Genomics for Animal and Plant Disease Consortium (GAP-DC), effectiveness is quantified through six interconnected work packages, each addressing specific aspects of genomic surveillance effectiveness [20]:
- Frontline pathogen detection performance at high-risk locations
- Spillover detection efficacy between wild and farmed/cultivated populations
- Diagnostic accuracy for syndromic or complex diseases
- Outbreak response capability for new and re-emerging diseases
- Endemic disease mitigation through integrated genomic and epidemiological data
- Coordination efficiency among stakeholders and end users
The GAP-DC initiative employs a cross-cutting technical approach across four domains to ensure robust quantification: (1) Sampling and Sequencing, (2) Data Processing and Analysis, (3) Quality Assurance - Validation and Accreditation, and (4) Evidence-to-Policy translation [20].
Methodologies for Quantitative Analysis
Experimental Protocol: Timeliness Metric Calculation
Objective: To quantify timeliness metrics for multisectoral outbreak detection and response within a One Health framework.
Materials and Data Collection:
- Compile a comprehensive database of outbreak events involving human, animal, plant, and environmental sectors
- Extract outbreak milestone dates from original investigation reports, Situation Reports, and formal government documents
- Supplement with data from targeted literature reviews of international health agency reports and peer-reviewed publications
- Document additional variables: geographic distribution, cross-border transmission, past outbreak frequency, transmission route, pathogen type, and surveillance method
Statistical Analysis:
- Calculate descriptive statistics for time intervals between all respective milestones
- Stratify metrics by year, region, disease, pathogen type, transmission route, surveillance type, and One Health sectors involved
- Perform Cox proportional hazards regression analyses to assess changes in speed over time between respective milestones
- For milestones occurring on the same date, adjust the second milestone to 0.3 days (equivalent to 8 hours) for analytical purposes
- Implement appropriate imputation methods for missing dates based on the logic of subsequent milestone dates [96]
Experimental Protocol: Genomic Surveillance Effectiveness
Objective: To evaluate the effectiveness of genomic surveillance systems in detecting and characterizing pathogens across One Health sectors.
Sample Collection and Sequencing:
- Implement robust sampling strategies across diverse hosts and environments (animal, plant, aquatic)
- Deploy satellite or mobile laboratory facilities at high-risk locations for frontline pathogen detection
- Utilize high-throughput sequencing technologies for comprehensive pathogen genomic characterization
- Apply both whole-genome sequencing and metagenomic approaches based on surveillance objectives
Data Processing and Analysis:
- Implement bioinformatics pipelines for pathogen detection, transmission tracking, and evolution analysis
- Apply computational tools for identifying markers of virulence, resistance, and transmission
- Integrate genomic data with epidemiological approaches for outbreak investigation
- Utilize environmental metagenomics for comprehensive pathogen detection [20]
Quality Assurance and Validation:
- Establish rigorous quality control measures throughout the sequencing and analysis workflow
- Ensure data reliability, reproducibility, and compliance with accreditation frameworks
- Validate findings through comparative analysis with existing surveillance programs
- Implement standardized protocols for data sharing and interoperability
Quantitative Outcomes and Data Visualization
Timeliness Performance Data
Analysis of 81 outbreaks in Uganda between 2018-2022 revealed distinct patterns in timeliness performance across different types of health threats [96]. The quantitative findings demonstrate that:
Table 2: Timeliness Performance by Outbreak Characteristic
| Outbreak Characteristic | Median Detection Time (Days) | Median Response Time (Days) | Key Influencing Factors |
|---|---|---|---|
| Frequent Past Experience | Significantly faster | Significantly faster | Established protocols, familiar pathogens |
| Viral Hemorrhagic Fevers | Faster | Faster | Perceived high threat, pre-existing preparedness |
| Novel/Unknown Pathogens | Significantly slower | Significantly slower | Lack of diagnostic tools, unfamiliar clinical presentation |
| Strong One Health Collaboration | Faster | Faster | Integrated reporting, shared resources |
The data reveals that while teams respond quickly to known diseases, novel diseases that the health system is unfamiliar with take longer to detect and address. Enhanced coordination between animal, human, and environmental health sectors demonstrates measurable improvements in timeliness metrics [96].
Cost-Benefit Considerations in Genomic Surveillance
While specific financial data requires comprehensive economic analysis, the GAP-DC initiative identifies several critical cost-benefit considerations [20]:
- Prevention Efficiency: Early detection through genomic surveillance prevents economic losses from full-scale outbreaks in livestock, crops, fisheries, forestry, and aquaculture
- Resource Optimization: Coordinated approaches across agencies prevent duplication of efforts and maximize resource utilization
- Trade Protection: Effective surveillance maintains compliance with international trade standards, protecting agricultural exports
- Health Security Investment: Proactive genomic surveillance represents a cost-effective alternative to reactive pandemic response
The UK's approach to biological hazards, underpinned by its biological security strategy's four foundational pillars (understand, prevent, detect, and respond), emphasizes surveillance as an early warning tool and first line of defense against endemic and emerging pathogens and pests [20].
Visualization of One Health Genomic Surveillance Workflow
The following diagram illustrates the integrated workflow for One Health genomic surveillance and outcome quantification:
One Health Genomic Surveillance Pipeline
Timeliness Metrics Framework Visualization
The following diagram details the sequence of milestones in the One Health timeliness metrics framework:
Outbreak Timeliness Metric Milestones
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for One Health Genomic Surveillance
| Reagent/Material | Function | Application Context |
|---|---|---|
| High-Throughput Sequencing Kits | Generate comprehensive genomic data from diverse sample types | Pathogen characterization, antimicrobial resistance monitoring |
| Metagenomic Sequencing Reagents | Enable detection of unknown pathogens without prior targeting | Surveillance of novel disease threats, environmental sampling |
| Cross-Sector Sample Collection Kits | Standardize specimen collection across human, animal, environmental domains | Integrated surveillance, outbreak investigation |
| Bioinformatics Pipelines | Process and analyze genomic data for pathogen detection | Transmission tracking, virulence marker identification |
| Quality Control Standards | Ensure data reliability and reproducibility across laboratories | Method validation, inter-laboratory comparisons |
| One Health Data Integration Platforms | Harmonize data from multiple sectors for comprehensive analysis | Timeliness metric calculation, outcome quantification |
Discussion and Implementation Considerations
The quantification of outcomes in One Health genomic sciences requires ongoing refinement of metrics and methodologies. Current evidence demonstrates that the effectiveness of One Health initiatives is significantly enhanced through cross-sectoral collaboration, standardized protocols, and integrated data systems [20] [96]. The timeliness metrics framework offers a validated approach for quantitative assessment of outbreak detection and response performance, enabling objective evaluation of system strengths and weaknesses.
Implementation of these quantitative frameworks faces several challenges, including the need for standardized data collection across sectors, interoperability of reporting systems, and resource allocation for sustained genomic surveillance capacity [96]. Furthermore, analyses of National One Health Strategic Plans have revealed varying levels of alignment with contemporary One Health principles, with specific actions inconsistently anticipated across plans [97]. Disparities in addressing issues such as climate change, anthropogenic drivers, and non-communicable diseases were also evident, highlighting areas for future development.
For researchers and drug development professionals, adopting these quantitative frameworks enables more rigorous evaluation of One Health interventions, strengthens evidence-based policy development, and optimizes resource allocation for maximum public health impact. Future directions should focus on expanding surveillance networks, enhancing bioinformatics capabilities, and integrating innovative technologies to address evolving challenges, including building predictive capabilities to better anticipate and mitigate disease impact [20].
Validating Cross-Species Genomic Predictions for Health and Disease
The One Health approach recognizes that the health of humans, animals, and ecosystems are interdependent, pushing scientific inquiry beyond traditional siloed approaches to coordination and integration [36]. In genomic sciences, this approach enables researchers to address complex health challenges at the human-animal-environment interface through cross-species genomic analyses that can identify novel hypotheses and improve early warning systems for impending health events [36]. The emerging discipline of cross-species genomic prediction represents a paradigm shift in how we understand population health across species boundaries, leveraging advanced computational tools and large-scale genomic datasets to translate findings between biological kingdoms.
This technical guide examines the validation frameworks, methodological considerations, and practical implementations for cross-species genomic predictions. By leveraging genomic tools and methods across human, animal, and plant genetics, researchers can address a significant gap in current scientific practice, where these fields have historically developed in isolation despite using similar underlying models and approaches [10]. The validation of these cross-species predictions requires sophisticated statistical frameworks and integrated data systems that can accommodate the complexity of multi-species genomic data while maintaining scientific rigor and biological relevance.
Quantitative Frameworks for Genomic Prediction
Genomic Prediction Models and Their Components
Genomic prediction is an effective method for shortening breeding cycles and accelerating genetic gains, with traditional approaches focusing on estimating 'additive' breeding values for individual genotypes [98]. For comprehensive cross-species prediction, models must incorporate both additive and non-additive genetic effects to account for the full spectrum of genetic contributions to complex traits. The genomic predicted cross-performance (GPCP) tool represents one advanced implementation, utilizing a mixed linear model based on additive and directional dominance effects [98]. This approach is particularly valuable for traits with significant dominance effects and for clonally propagated crops where inbreeding depression and heterosis are prevalent.
The fundamental GPCP model can be represented as:
y = Xb + Fα + Za + Wd + e [98]
Where:
- y is a vector of phenotype means
- X is an incidence matrix for fixed effects (b)
- F represents the vector with inbreeding coefficients and α indicates the effect of genomic inbreeding on performance
- Z stores allele dosages scaling the additive effects vector (a)
- W captures heterozygosity for dominance effects (d)
- e represents residual effects
This model effectively partitions genetic variance into its constituent components, allowing for more accurate prediction of cross-performance in breeding programs and potentially in cross-species applications.
Statistical Validation Approaches
Validating cross-species genomic predictions requires rigorous statistical frameworks to ensure predictive accuracy and biological relevance. The following comparative data illustrate key metrics and approaches:
Table 1: Performance Metrics for Genomic Prediction Models Across Species Boundaries
| Metric | Human Genetics Applications | Animal Breeding Applications | Plant Genetics Applications |
|---|---|---|---|
| Prediction Accuracy Range | 0.15-0.45 for complex behavioral traits | 0.35-0.75 for production traits | 0.40-0.80 for yield traits |
| Typical Dataset Size | 10,000-1,000,000 individuals | 1,000-100,000 individuals | 1,000-50,000 individuals |
| Key Methodological Approaches | Polygenic risk scores, Genome-wide association studies | Genomic estimated breeding values, Selection indices | Genomic selection, Hybrid performance prediction |
| Primary Validation Method | Hold-out validation, External cohort replication | Cross-validation, Progeny testing | Cross-validation, Field trials |
| Data Integration Challenges | Ethical constraints, Phenotypic heterogeneity | Multi-trait evaluation, Genotype by environment interactions | High-throughput phenotyping, Environmental covariates |
Table 2: Quantitative Comparison of Experimental Results for Method Validation
| Validation Method | Implementation Requirements | Strengths | Limitations |
|---|---|---|---|
| t-test Comparison | Two sample groups with calculated means, standard deviations, and sample sizes [99] | Determines if difference between two means is statistically significant; Simple to implement | Limited to comparison of two groups; Requires normal distribution assumption |
| F-test for Variances | Two data sets to compare spread of values [99] | Assesses equality of variances before t-test; Important for model assumptions | Must be ≥1 (s1² ≥ s2²); Limited to variance comparison only |
| Cross-species Prediction Accuracy | Large datasets from multiple species; Genomic and phenotypic records [10] | Directly measures transferability of predictions across species; Most relevant validation | Requires substantial genomic resources across multiple species; Complex interpretation |
For determining statistical significance between experimental results, the t-test provides a fundamental validation tool, with the formula:
t = (x̄₁ - x̄₂) / [s√(1/n₁ + 1/n₂)] [99]
Where x̄₁ and x̄₂ are the sample means, s is the pooled estimate of standard deviation, and n₁ and n₂ are the sample sizes. The number of degrees of freedom (df) is (n₁ + n₂) - 2. The null hypothesis (H₀) assumes no difference between means, while the alternative hypothesis (H₁) proposes a significant difference exists [99]. Rejection of H₀ occurs when the absolute t-value exceeds the critical value at a specified significance level (typically α = 0.05), indicating statistically significant differences.
Methodological Implementation
Experimental Workflows for Cross-Species Genomic Analysis
The validation of cross-species genomic predictions requires carefully designed experimental workflows that ensure methodological rigor while accommodating the unique challenges of multi-species data integration. The following diagram illustrates a comprehensive framework:
One Health Data Integration Framework
Implementing cross-species genomic predictions requires robust data integration frameworks that can accommodate the diverse data sources inherent to One Health approaches. The development of such frameworks involves systematic processes:
Table 3: One Health Data Integration Framework Development
| Development Phase | Key Activities | Outputs | Stakeholder Engagement |
|---|---|---|---|
| Conceptualization | Hypothesis generation; Study aim definition; Relationship mapping between exposure sources and outcomes [100] | Directed Acyclic Graphs; Logic models; Multi-pathway visualization matrices | Multidisciplinary team assembly; Community member involvement |
| Planning | Study design determination; Data source identification; Analytical method selection [100] | Mixed methodology protocols; Power and sample size computations; Data collection strategies | Specialist consultation; Resource aggregation; Capacity assessment |
| Implementation | System development; Data collection; Integration pipeline construction | Functional data systems; Automated collection protocols; Analysis platforms | Cross-sector training; Joint development; Governance establishment |
| Operationalization | Joint data analysis; Interpretation; Dissemination; System refinement | One Health surveillance outputs; Early warning systems; Intervention strategies | Ongoing collaborative relationships; Communication protocols |
Successful implementation of One Health data integration requires moving beyond simple data sharing to true co-analysis of integrated datasets, which presents both technical and governance challenges. Key considerations include:
- Complex Partner Identification: Engaging relevant stakeholders across human, animal, and environmental health domains [100]
- Co-development Requirements: Establishing shared goals and system scope through collaborative processes [36]
- Data Governance Frameworks: Navigating complex data sharing agreements and jurisdictional mandates [36]
- Joint Analysis Protocols: Developing capacity for integrated analysis, reporting, and interpretation across sectors [36]
Essential Research Reagents and Computational Tools
The experimental validation of cross-species genomic predictions requires specific research reagents and computational resources:
Table 4: Research Reagent Solutions for Cross-Species Genomic Studies
| Category | Specific Examples | Function/Application | Implementation Considerations |
|---|---|---|---|
| Genomic Data Resources | UK Biobank; EnsemblPlants; Livestock Research Data Ecosystems [10] | Provide large-scale phenotypic and genomic data for model training and validation | Data use agreements; Ethical considerations; Computational infrastructure |
| Analysis Software & Packages | BreedBase; R packages (sommer); AlphaSimR [98] | Implement genomic prediction models; Perform simulations; Statistical analysis | Computational resource requirements; Technical expertise; Customization needs |
| Statistical Validation Tools | XLMiner ToolPak; Analysis ToolPak; Custom scripts for t-tests and F-tests [99] | Compare experimental results; Determine statistical significance; Validate predictive models | Appropriate test selection; Significance threshold setting; Interpretation frameworks |
| Pathogen Genomic Resources | PulseNet; GenomeTrakr; NCBI databases [36] | Support integrated genomic surveillance; Enable phylogenetic analysis across species | Laboratory capacity for sequence generation; Bioinformatics expertise; Data standardization |
Technical Protocols for Validation
Protocol 1: Cross-Species Genomic Prediction Validation
This protocol outlines the steps for validating genomic predictions across species boundaries, adapted from methodologies successfully implemented in both animal and plant genetics [98] [10].
Step 1: Data Collection and Harmonization
- Collect genomic and phenotypic data from source species (e.g., livestock or plant models)
- Gather corresponding data from target species (e.g., human populations)
- Perform quality control on all datasets (SNP call rate, minor allele frequency, Hardy-Weinberg equilibrium)
- Harmonize genomic data through orthologous gene mapping and synteny analysis
Step 2: Model Training and Parameter Estimation
- Partition source species data into training and validation sets
- Train genomic prediction models (GPCP, GEBV, or other appropriate models) using the source species training set
- Estimate model parameters (additive and dominance effects, heritability, etc.)
- Validate model performance within the source species using cross-validation
Step 3: Cross-Species Prediction
- Apply the trained model to the target species genomic data
- Generate predicted phenotypic values for the target species
- Compare predictions with observed phenotypes in the target species
- Calculate prediction accuracy as the correlation between predicted and observed values
Step 4: Statistical Validation
- Perform t-tests to compare prediction accuracies across different model specifications
- Conduct F-tests to evaluate variance components between species
- Implement permutation tests to establish significance thresholds
- Apply false discovery rate corrections for multiple testing
Protocol 2: Integrated One Health Genomic Surveillance
This protocol describes the implementation of integrated genomic surveillance for pathogen tracking across human, animal, and environmental domains [36].
Step 1: Sample Collection and Sequencing
- Establish standardized sampling protocols across human, animal, and environmental sectors
- Collect samples from potential outbreak scenarios or routine surveillance
- Perform pathogen genomic sequencing using consistent laboratory protocols
- Generate high-quality genome sequences with appropriate coverage and quality metrics
Step 2: Data Integration and Management
- Develop shared metadata standards for all sectors
- Implement data integration platforms (APIs, cloud storage, shared databases)
- Ensure semantic interoperability through common ontologies and vocabularies
- Address data governance and sharing agreements between sectors
Step 3: Phylogenetic Analysis and Interpretation
- Perform multiple sequence alignment using appropriate algorithms
- Construct phylogenetic trees to assess transmission dynamics
- Identify cross-species transmission events and directionality
- Integrate epidemiological data to contextualize genomic findings
Step 4: Joint Analysis and Response
- Conduct coordinated interpretation sessions with representatives from all sectors
- Generate integrated reports with cross-sectoral recommendations
- Implement appropriate public health, veterinary health, and environmental interventions
- Establish feedback mechanisms for system improvement
Applications and Implementation
Practical Applications in One Health Contexts
Validated cross-species genomic predictions enable numerous practical applications within the One Health framework:
Infectious Disease Surveillance and Control Integrated genomic surveillance systems allow for early outbreak detection and improved understanding of pathogen reservoirs, evolution, and modes of transmission across species boundaries [36]. The implementation of phylogenetic analysis enables assessment of transmission dynamics at the human-animal-environment interface, providing critical information for targeted interventions.
Agricultural Resilience and Food Security Cross-species genomic prediction methods developed in animal genetics can be applied to improve predictions of complex traits in humans, such as resilience, disease resistance, or responses to environmental stressors [10]. Similarly, approaches from human genetics may inform animal and plant breeding programs aimed at enhancing productivity and sustainability.
Environmental Health Monitoring By integrating genomic data from multiple species with environmental monitoring data, researchers can develop early warning systems for ecosystem health threats and identify potential zoonotic disease emergence hotspots before they lead to widespread outbreaks.
Implementation Challenges and Solutions
The implementation of cross-species genomic prediction systems faces several significant challenges:
Table 5: Implementation Challenges and Mitigation Strategies
| Challenge Category | Specific Challenges | Potential Mitigation Strategies |
|---|---|---|
| Technical Barriers | Data heterogeneity; Lack of semantic interoperability; Computational infrastructure requirements [36] | Develop common data standards; Implement middleware solutions; Cloud-based computing resources |
| Governance Issues | Data jurisdiction; Organizational mandates; Privacy and ethical concerns [36] | Establish clear data sharing agreements; Develop ethical frameworks; Engage legal experts early |
| Resource Constraints | Funding limitations; Technical capacity gaps; Aging data infrastructure [36] | Pursue cross-sector funding opportunities; Implement training programs; Phase modernization efforts |
| Analytical Complexities | Statistical methods for cross-species prediction; Validation frameworks; Interpretation challenges | Develop specialized statistical tools; Establish validation standards; Create interdisciplinary analysis teams |
The pathway toward operationalizing cross-species genomic predictions requires coordinated effort across multiple domains, but offers substantial potential benefits for improving health outcomes across species boundaries. As these methods mature and validation frameworks become more robust, the integration of genomic predictions into routine One Health practice will enhance our ability to predict, prevent, and respond to complex health challenges at the human-animal-environment interface.
The integration of genomic sciences into public health practice represents a transformative frontier for the One Health approach, which recognizes the interconnectedness of human, animal, and environmental health. This technical guide explores how the systematic evaluation of One Health surveillance systems—specifically through the OH-EpiCap tool—can identify critical pathways for effectively incorporating genomic data into integrated health monitoring. As pathogen genomics generates increasingly large and complex datasets, the organizational and operational frameworks of our surveillance systems must evolve to translate this data into actionable public health insights. The lessons drawn from multi-country applications of OH-EpiCap provide a evidence-based foundation for strengthening the epidemiological capabilities that underpin genomic research applications across health domains.
The OH-EpiCap tool was developed to address a recognized gap in evaluating the multi-sectoral collaboration essential for effective One Health surveillance [101]. Its development responded to the reality that while international health agencies strongly promote One Health approaches, most surveillance systems remain functionally compartmentalized with limited cross-sectoral collaboration [101]. This evaluation framework enables institutes and governments to systematically characterize, assess, and monitor their One Health epidemiological surveillance capacities and capabilities, creating a foundation upon which advanced genomic technologies can be effectively leveraged.
The OH-EpiCap Framework: Structure and Scoring Methodology
Tool Architecture and Evaluation Dimensions
OH-EpiCap is organized around three primary dimensions, each divided into four targets that contain four specific indicators, creating a comprehensive evaluation framework of 48 indicators total [101] [102]. This structure enables a systematic assessment of One Health surveillance systems across organizational, operational, and impact aspects.
Table 1: OH-EpiCap Evaluation Framework Structure
| Dimension | Targets | Key Indicator Examples |
|---|---|---|
| Organization | 1.1 Formalization | Common aim, support documentation, coordination roles, leadership |
| 1.2 Coverage & Transdisciplinarity | Relevant sectors, disciplines, geography, populations, hazards | |
| 1.3 Resources | Financial & human resources, shared operational resources, training | |
| 1.4 Evaluation & Resilience | Internal/external evaluations, corrective measures, adaptability | |
| Operational Activities | 2.1 Data Collection & Methods Sharing | Collaborative surveillance design, harmonized laboratory techniques |
| 2.2 Data Sharing | Data sharing agreements, FAIR principle compliance, data quality | |
| 2.3 Data Analysis & Interpretation | Multi-sectoral data analysis, shared statistical techniques | |
| 2.4 Communication | Internal/external communication, dissemination to decision-makers | |
| Impact | 3.1 Technical Outputs | Timely emergence detection, knowledge improvement, cost reduction |
| 3.2 Collaborative Added Value | Strengthened networks, international collaboration, common strategy | |
| 3.3 Immediate & Intermediate Outcomes | Advocacy, awareness, preparedness, evidence-based interventions | |
| 3.4 Ultimate Outcomes | Research opportunities, policy changes, better health outcomes |
Scoring System and Implementation Protocol
The OH-EpiCap employs a semi-quantitative scoring methodology with four levels of compliance for each indicator, where higher values indicate better adherence to One Health principles [101] [102]. The implementation protocol involves:
- Evaluation Workshop: Assembling a panel of surveillance representatives for a half-day workshop or iterative consultation process to reach scoring consensus [101]
- Questionnaire Administration: Using a standardized questionnaire with one question per indicator to facilitate consistent information collection [102]
- Result Visualization: Employing an R Shiny-based web application for results visualization and benchmarking against previous evaluations or other systems [101] [102]
The tool includes "Not Applicable" options for indicators irrelevant to specific surveillance contexts, enhancing its adaptability across different systems and hazards [102]. This consistent yet flexible approach enables meaningful cross-system comparisons while respecting contextual differences.
Figure 1: OH-EpiCap evaluation framework structure showing the three dimensions, twelve targets, and forty-eight indicators.
Multi-Country Case Studies: Application and Findings
Case Study Implementation and Methodology
The OH-EpiCap tool was rigorously tested through eleven case studies conducted in 2022, focusing on diverse foodborne hazards and antimicrobial resistance surveillance systems across multiple European countries [101] [103]. These evaluations targeted:
- Antimicrobial Resistance: Surveillance systems in Portugal and France [103]
- Salmonella: Surveillance in France, Germany, and the Netherlands [103] [104]
- Listeria: Surveillance in the Netherlands, Finland, and Norway [103]
- Campylobacter: Surveillance in Norway and Sweden [103]
- Psittacosis: Surveillance in Denmark [103]
The evaluation methodology involved multi-stakeholder workshops bringing together representatives from human, animal, and environmental health sectors to reach consensus on scoring. The number of assessors per case study ranged from one to five, with evaluation durations spanning 2-8 hours [105]. This collaborative scoring approach helped mitigate individual subjectivity while fostering shared understanding across sectors.
Key Findings and Identified System Gaps
The case study evaluations revealed consistent strengths and weaknesses across the surveillance systems, providing actionable insights for system improvement:
Table 2: Common Strengths and Weaknesses Identified in Multi-Country Case Studies
| Aspect | Strengths | Weaknesses |
|---|---|---|
| Organization | Sector coverage, coordination during crises | Lack of operational leadership, formal governance |
| Operational Activities | Data collection protocols, information sharing during alerts | Poor FAIR data principle compliance, limited technique sharing |
| Impact | Timely detection, knowledge improvement | Unmeasured cost-effectiveness, unassessed health outcomes |
Specific challenges identified included:
- Limited Formal Governance: Most systems lacked dedicated operational leadership and formal governance structures with representatives from all sectors [103]
- Data Sharing Barriers: Inconsistent application of FAIR (Findable, Accessible, Interoperable, Reusable) data principles impeded effective data integration [103]
- Impact Measurement Gaps: The effectiveness, operational costs, behavioral changes, and population health outcomes attributable to One Health surveillance were rarely evaluated [103] [104]
These findings highlight critical gaps between technical capabilities and operational implementation that must be addressed to fully leverage genomic technologies in One Health surveillance.
Interfacing Surveillance Evaluation with Genomic Sciences
Genomic Technologies as Enablers of One Health Surveillance
Genomic technologies and bioinformatics provide powerful tools for decoding complex biological data, enabling comprehensive insights into pathogen evolution, transmission dynamics, and host-pathogen interactions across species and ecosystems [11]. When effectively integrated into One Health surveillance systems, these technologies enable:
- Enhanced Pathogen Characterization: Metagenomic next-generation sequencing (mNGS) facilitates diagnosis of complex clinical cases and detection of novel pathogens [7]
- Molecular Epidemiology: Advanced sequencing technologies transform how infectious diseases are detected and tracked across human, animal, and environmental domains [7]
- Antimicrobial Resistance Monitoring: Genomic surveillance provides critical insights into AMR patterns and transmission pathways [11]
The targeted application of genomic technologies is particularly valuable in tropical regions, which face disproportionate burdens of infectious diseases but have historically been underrepresented in genomic research initiatives [7]. Portable sequencing technologies and bespoke bioinformatics solutions offer promising approaches to address these regional disparities.
Infrastructure Requirements for Genomic Integration
Successful integration of genomic data into One Health surveillance requires addressing several critical infrastructure challenges:
- Data Integration Frameworks: Systems capable of combining genomic data with epidemiological information and environmental factors to enable comprehensive analysis [106]
- Computing Infrastructure: Robust bioinformatics capacity and computing resources to process and analyze large-scale genomic datasets [7]
- Workforce Development: Cross-trained professionals with expertise in both genomic sciences and public health practice [106]
- Standardized Tools: Analytical methods and visualization tools applicable to routine data analysis within public health timeframes [106]
The OH-EpiCap evaluations identified that systems scoring higher on operational targets related to data sharing and analysis were better positioned to effectively incorporate genomic technologies, highlighting the interdependence between surveillance fundamentals and advanced technological capabilities.
Implementation Guidance: Enhancing One Health Genomic Surveillance
Strategic Recommendations for System Improvement
Based on the OH-EpiCap case study findings, the following strategic approaches can enhance the integration of genomic sciences into One Health surveillance:
- Establish Formal Governance Structures: Create dedicated governance bodies with representatives from human, animal, and environmental health sectors to provide operational leadership and strategic direction [103]
- Implement FAIR Data Principles: Develop and adopt data sharing protocols that ensure genomic and epidemiological data are Findable, Accessible, Interoperable, and Reusable across sectors [103]
- Demonstrate Impact Value: Systematically document and communicate the added value of integrated genomic surveillance, including improved outbreak detection, more targeted interventions, and cost savings [103] [104]
- Build Cross-Sectoral Analytical Capacity: Invest in shared bioinformatics resources and cross-training programs that enable collaborative analysis of integrated datasets [7] [106]
Research Reagent Solutions for One Health Genomic Surveillance
Table 3: Essential Research Reagents and Tools for One Health Genomic Surveillance
| Reagent/Tool Category | Specific Examples | Function in One Health Surveillance |
|---|---|---|
| Sequencing Platforms | Oxford Nanopore Technologies, Illumina systems | Enable pathogen whole genome sequencing and metagenomic analysis |
| Bioinformatics Pipelines | Genome assemblers, variant callers, phylogenetic tools | Support analysis of genomic data for outbreak investigation and pathogen characterization |
| Reference Databases | Custom-built databases for local flora/fauna, antimicrobial resistance genes | Provide context for interpreting genomic findings in local ecosystems |
| Data Integration Tools | Interoperable data platforms, shared analysis environments | Facilitate combination of genomic, epidemiological, and environmental data |
| Quality Control Materials | Standardized controls, validation panels | Ensure reliability and comparability of genomic data across sectors and time |
These research reagents and tools collectively enable the generation, analysis, and interpretation of genomic data within a One Health context, addressing the operational gaps identified through OH-EpiCap evaluations.
Figure 2: Implementation pathway from identified challenges through solutions to enhanced capabilities for One Health genomic surveillance.
The application of OH-EpiCap across diverse surveillance systems and geographical contexts provides compelling evidence that systematic evaluation of One Health capacities is both feasible and valuable for identifying concrete improvements. The tool's structured assessment of organization, operational activities, and impacts creates a comprehensive framework for strengthening the foundational elements necessary for effective genomic surveillance. As genomic technologies continue to transform disease detection and tracking, the integration challenges identified through these real-world evaluations—particularly regarding governance, data sharing, and impact measurement—must be addressed to fully realize the potential of genomics within a One Health approach.
The lessons from OH-EpiCap implementation demonstrate that technical capabilities alone are insufficient without corresponding advancements in collaborative structures and processes. Future efforts should focus on developing and validating specific indicators for genomic data integration within the OH-EpiCap framework, enabling more targeted assessment of this critical capability. By building on these evaluation findings and addressing the identified gaps, the global health community can accelerate progress toward genuinely integrated surveillance systems that leverage genomic sciences to protect health across human, animal, and environmental domains.
The Genomics for Animal and Plant Disease Consortium (GAP-DC) represents a pioneering initiative that positions the United Kingdom at the forefront of applying genomic surveillance to national biosecurity challenges. Launched in July 2023 and backed by £10 million in government funding, GAP-DC operationalizes the One Health principle by integrating surveillance efforts across terrestrial and aquatic animals, plants, and their shared environments [107] [108] [20]. This in-depth technical guide examines the consortium's structure, methodological frameworks, and technical workflows, presenting it as a replicable model for leveraging genomic technologies to protect agriculture, trade, and public health against emerging biological threats.
The One Health approach is a collaborative, multisectoral, and transdisciplinary framework that recognizes the inextricable interconnection between the health of people, animals, plants, and their shared environment [9] [1]. In an era characterized by globalization, climate change, and increasing antimicrobial resistance, this approach is critical for addressing complex health challenges that transcend traditional sectoral boundaries [11] [67]. Zoonotic diseases—pathogens that can transfer between animals and humans—account for a significant proportion of emerging infectious diseases, underscoring the necessity of integrated surveillance systems [9] [67].
Genomic surveillance has emerged as a powerful tool within the One Health arsenal. By decoding the complete genetic material of pathogens, researchers can achieve precise identification, track transmission dynamics in real-time, trace outbreaks to their source, and gain insights into pathogen evolution and host-pathogen interactions [11] [20]. The strategic application of high-throughput sequencing (HTS) technologies, supported by robust bioinformatics, enables a proactive shift from disease response to prediction and prevention [20] [7].
The GAP-DC Initiative: Strategic Objectives and Governance
Consortium Structure and Funding
GAP-DC unites the UK's leading organizations in pathogen detection and genomics to create a cohesive national biosecurity front. The consortium is funded by £10 million from the Department for Environment, Food and Rural Affairs (Defra) and UK Research and Innovation (UKRI) [108]. Its governance structure integrates expertise from key partners, creating a unified framework for tackling established and emerging pathogens across ecosystems [107] [20].
Table 1: GAP-DC Core Consortium Partners and Their Specializations
| Organization | Area of Expertise | Role in GAP-DC |
|---|---|---|
| Animal and Plant Health Agency (APHA) | Animal health, disease diagnostics | Lead agency, overall project coordination [108] |
| Pirbright Institute (TPI) | Viral diseases of livestock | Pathogen genomics, vaccine research [107] |
| Royal Veterinary College (RVC) | Veterinary medicine, epidemiology | Infectious disease genomics, animal health [108] |
| Centre for Environment, Fisheries and Aquaculture Science (CEFAS) | Aquatic animal health | Health of marine and freshwater organisms [108] [20] |
| Fera Science Ltd | Plant health, agri-technology | Plant pathogen detection, food security [107] [20] |
| Forest Research | Forest science, tree health | Monitoring and controlling tree diseases [108] |
Alignment with National and Global Frameworks
GAP-DC is strategically aligned with the UK Biological Security Strategy (2023), which is built on four foundational pillars: understand, prevent, detect, and respond [107] [20]. The initiative serves as a direct implementation vehicle for the "detect" pillar, enhancing the UK's early warning surveillance capabilities [20]. Furthermore, GAP-DC actively engages with global One Health initiatives such as the European Partnership for Animal Health and Welfare and the African Field Epidemiology Network, fostering methodological alignment and data sharing to address transboundary disease threats [20].
Technical Framework: Work Packages and Methodologies
The operational scope of GAP-DC is defined by six interconnected work packages (WPs), each targeting a critical aspect of the genomic surveillance pipeline [20].
WP1: Frontline Pathogen Detection at Borders
- Objective: To deploy and evaluate HTS technologies at high-risk entry points, such as border control posts, for rapid, unbiased pathogen detection.
- Methodology: Establishment of satellite or mobile laboratory facilities equipped with portable sequencing technologies (e.g., Oxford Nanopore Technologies). Samples from imported goods, plants, or animals are subjected to metagenomic next-generation sequencing (mNGS). This agnostic approach sequences all genetic material in a sample, allowing for the detection of known, novel, and unexpected pathogens without prior knowledge of what might be present [20] [7].
- Bioinformatic Analysis: Sequencing data is processed through customized bioinformatics pipelines for taxonomic classification, pathogen identification, and virulence/AMR gene screening.
WP2: Pathogen Spillover at Wildlife-Domestic Interfaces
- Objective: To detect and characterize pathogens moving between wild and farmed or cultivated populations.
- Methodology: Systematic sampling in interface zones (e.g., near farms, aquaculture sites). Samples (e.g., swabs, tissue, water, soil) are analyzed using both targeted (PCR) and agnostic (mNGS) genomic methods. Host-specific molecular markers are used to trace the source of fecal contamination in water, and phylogenetic analysis is applied to pathogen genomes to confirm transmission pathways between wild and domestic populations [20].
WP3: Syndromic and Complex Disease Elucidation
- Objective: To identify causative agents in diseases of unknown or complex etiology, such as post-weaning mortality in pigs or red skin disease in salmon.
- Methodology: Application of whole-genome sequencing (WGS) of bacterial and fungal isolates from clinical cases. For viral discovery, transcriptome sequencing (RNA-Seq) of host tissues is employed. Case-control metagenomic studies compare the microbial communities of diseased and healthy individuals to identify statistically significant associations with potential pathogens [20] [7].
WP4: Outbreak Management of New and Re-Emerging Diseases
- Objective: To leverage genomic data for swift, evidence-based outbreak response.
- Methodology: During an outbreak, rapid WGS of pathogen isolates is performed. Genomes are analyzed in real-time to identify genetic markers of virulence and transmission. Phylodynamic models are used to reconstruct the outbreak's transmission tree, estimate its growth rate, and identify potential super-spreading events, directly informing control measures like targeted culling or movement restrictions [20].
WP5: Mitigation of Endemic Diseases
- Objective: To develop sustainable management strategies for long-established diseases that burden agriculture.
- Methodology: Long-term genomic surveillance of endemic pathogens (e.g., Salmonella, Phytophthora) to monitor their population genetics and evolution. Genomic data is integrated with epidemiological information to understand the drivers of persistence and spread. This data helps in assessing the effectiveness of control programs and in forecasting the risk of strain emergence [20].
WP6: Stakeholder Coordination and Policy Translation
- Objective: To ensure scientific evidence is effectively translated into policy and public communication.
- Methodology: Establishment of regular cross-agency forums and stakeholder engagement workshops. Development of comprehensive cost-benefit analyses for genomic surveillance interventions. Creation of standardized data sharing agreements and public-facing communication templates for health crises [20].
The following diagram illustrates the logical flow and integration between these work packages and the cross-cutting technical domains that support them.
Cross-Cutting Technical Domains
Four key technical domains provide a unified foundation across all work packages, ensuring data robustness and operational coherence [20]:
- Sampling and Sequencing: Establishes standardized protocols for sample collection, nucleic acid extraction, and the application of various HTS platforms (e.g., short-read, long-read, metagenomic) to ensure representative pathogen detection.
- Data Processing and Analysis: Develops and maintains bioinformatics pipelines for tasks including genome assembly, annotation, phylogenetic inference, and metagenomic read classification.
- Quality Assurance, Validation, and Accreditation: Implements rigorous standards and controls to ensure data reliability, reproducibility, and compliance with international accreditation frameworks (e.g., ISO standards).
- Evidence-to-Policy: Focuses on the translation of complex genomic data into accessible formats, actionable intelligence, and evidence-based policy recommendations for decision-makers.
The Scientist's Toolkit: Essential Research Reagents and Platforms
The experimental protocols within GAP-DC rely on a suite of advanced genomic technologies and reagents. The following table details key solutions essential for work in this field.
Table 2: Key Research Reagent Solutions for Genomic Surveillance
| Reagent / Technology | Function / Application | Example Use in GAP-DC |
|---|---|---|
| Portable Sequencers (e.g., Oxford Nanopore) | Enables real-time, long-read sequencing in field laboratories or at borders [7]. | Rapid detection of pathogens at high-risk locations (WP1) [20]. |
| Metagenomic Sequencing Kits | Allows for unbiased sequencing of all nucleic acids in a complex sample (e.g., tissue, soil, water) [7]. | Discovery of novel pathogens and analysis of complex disease etiologies (WP2, WP3) [20]. |
| Whole Genome Amplification Kits | Amplifies minute quantities of DNA from low-biomass or difficult-to-culture samples. | Generating sufficient material for sequencing from environmental or clinical swabs [20]. |
| Targeted Enrichment Panels | Probes designed to capture and enrich specific genomic regions (e.g., for a virus family or AMR genes). | Cost-effective deep sequencing of specific pathogens during outbreaks (WP4) [20]. |
| Standardized Nucleic Acid Extraction Kits | Ensures high-quality, inhibitor-free DNA/RNA from diverse sample matrices (plant, animal, environmental). | Maintains consistency and reproducibility across different consortium partners and sample types [20]. |
| Bioinformatics Pipelines (e.g., BWA, GATK, IQ-TREE) | Open-source software for sequence alignment, variant calling, and phylogenetic reconstruction. | Core data processing and analysis for all work packages; essential for tracking pathogen evolution [11] [20]. |
Quantitative Impact and Economic Rationale
The economic imperative for robust biosecurity initiatives like GAP-DC is compelling. The UK faces significant and growing economic threats from pests and diseases affecting its agriculture, livestock, and natural environment [108]. The following table summarizes the economic impact of key diseases, underscoring the need for advanced surveillance.
Table 3: Economic Impact of Select Animal and Plant Diseases in the UK
| Disease / Pest | Affected Sector | Economic Impact / Cost |
|---|---|---|
| Ash Dieback | Forestry, Environment | Projected to cost £15 billion over coming decades [108]. |
| Avian Influenza | Poultry Agriculture | Cost the poultry meat sector over £100 million in a two-year period [108]. |
| Invasive Species | Multiple Sectors | Estimated to cost the UK economy £4 billion annually [108]. |
Investments in preventive genomic surveillance, as exemplified by GAP-DC's £10 million funding, are economically rational when measured against the potential billions in losses from uncontrolled outbreaks [108] [67]. The consortium aims to mitigate these costs by enabling earlier detection, more precise control measures, and more resilient agricultural and food systems.
The UK's GAP-DC initiative presents a sophisticated, operational model for integrating genomic surveillance within a national One Health biosecurity strategy. By uniting diverse institutions under a common framework, implementing a structured work package methodology, and leveraging cutting-edge genomic technologies and bioinformatics, GAP-DC enhances the UK's capacity to safeguard its animal, plant, and economic health. This initiative demonstrates the transformative potential of a coordinated, cross-sectoral approach to disease surveillance, offering a valuable template for other nations seeking to build resilient and proactive biosecurity systems in an interconnected world. The continued success of such programs relies on sustained investment, interdisciplinary collaboration, and the ongoing integration of technological advancements into public health and agricultural policy.
Conclusion
The integration of genomic sciences within the One Health framework provides an indispensable, unified approach to tackling complex health challenges that transcend species and ecosystems. The key takeaways confirm that genomic surveillance enables predictive insights into pandemics and AMR, cross-species genomic analyses reveal critical transmission pathways of pathogens, and overcoming data integration and collaborative barriers is essential for success. Furthermore, evidence demonstrates that One Health genomic systems offer superior outcomes in outbreak management and biosecurity compared to traditional methods. Future efforts must focus on building equitable genomic capacities, particularly in tropical regions, standardizing global data-sharing protocols, and deepening the integration of AI and multi-omics data to fully realize the potential of One Health genomics in advancing biomedical research and precision public health.
References
- 1. One health [https://www.who.int/health-topics/one-health]
- 2. One Health: A new definition for a sustainable and healthy future [https://pmc.ncbi.nlm.nih.gov/articles/PMC9223325/]
- 3. Genomics and Bioinformatics in One Health [https://www.mdpi.com/1660-4601/21/10/1337]
- 4. The One Health Approach—Why Is It So Important? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6630404/]
- 5. Real‐time genomics for One Health - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10407731/]
- 6. Enabling One Health solutions through genomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8204826/]
- 7. Harnessing genomic technologies for one health solutions in ... [https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-024-01083-3]
- 8. A generalizable one health framework for the control of ... [https://www.nature.com/articles/s41598-022-12619-1]
- 9. About One Health [https://www.cdc.gov/one-health/about/index.html]
- 10. One Health: Using cross-species genomic analyses to ... [https://www.purdue.edu/research/features/stories/one-health-using-cross-species-genomic-analyses-to-track-population-health/]
- 11. Genomics and Bioinformatics in One Health [https://pubmed.ncbi.nlm.nih.gov/39457310/]
- 12. Genomics Transforms U.S. Public Health Surveillance [https://globalbiodefense.com/2025/08/29/genomics-us-public-health-surveillance/]
- 13. Exploring the Current State of Pathogen Genomics and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK615631/]
- 14. Integrated Genomic Surveillance (IGS) [https://www.rki.de/EN/Topics/Research-and-data/Surveillance-panel/IGS/integrated-genomic-surveillance-node.html]
- 15. Public Health Surveillance | Genomics-based approaches [https://www.illumina.com/areas-of-interest/microbiology/public-health-surveillance.html]
- 16. Integrating Genomic Data into Public Health Surveillance ... [https://wwwnc.cdc.gov/eid/article/31/13/24-1227_article]
- 17. Integrating Genomic Data into Public Health Surveillance for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078550/]
- 18. Balancing efficient analysis and storage of quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9355464/]
- 19. Genomic data in the All of Us Research Program [https://www.nature.com/articles/s41586-023-06957-x]
- 20. An integrated One Health initiative for pathogen genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591511/]
- 21. On the road to 2025 [https://www.who.int/teams/noncommunicable-diseases/on-the-road-to-2025]
- 22. One Health – Science Summit 2025 [https://sciencesummitnyc.org/report/one-health/]
- 23. Leveraging artificial intelligence for One Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532937/]
- 24. Unlocking the African bioeconomy and strengthening ... [https://www.nature.com/articles/s44185-025-00102-9]
- 25. African BioGenome Project – Genomics in the service of ... [https://africanbiogenome.org/]
- 26. Hidden challenges in evaluating spillover risk of zoonotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12092720/]
- 27. Genomics reveals zoonotic and sustained human mpox ... [https://www.nature.com/articles/s41586-025-09128-2]
- 28. New FAU-USF Research Rewrites Origins of the World's ... [https://www.fau.edu/newsdesk/articles/genomic-origins-first-pandemic.php]
- 29. Cytoscape: An Open Source Platform for Complex Network ... [https://cytoscape.org/]
- 30. Graphviz [https://graphviz.org/]
- 31. The integrated genomic surveillance system of Andalusia (SIEGA) provides a One Health regional resource connected with the clinic | Scientific Reports [https://www.nature.com/articles/s41598-024-70107-0]
- 32. Typing methods based on whole genome sequencing data | One Health Outlook | Full Text [https://onehealthoutlook.biomedcentral.com/articles/10.1186/s42522-020-0010-1]
- 33. Genomic insights into zoonotic transmission and antimicrobial resistance in Campylobacter jejuni from farm to fork: a one health perspective - PubMed [https://pubmed.ncbi.nlm.nih.gov/36471447/]
- 34. 20 Free Bioinformatics Tools for Genomic Data Analysis [https://ngscloud.com/20-free-bioinformatics-tools-for-genomic-data-analysis/]
- 35. Genomic Analysis Visualization Tool (GRAF) [https://velsera.com/products/graf/]
- 36. Developing a one health data integration framework focused ... [https://onehealthoutlook.biomedcentral.com/articles/10.1186/s42522-024-00133-5]
- 37. Comparative of metagenomic and targeted next-generation ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1534519/full]
- 38. Comparative diagnostic performance of metagenomic and ... [https://www.nature.com/articles/s41598-025-11834-w]
- 39. Comparative analysis of metagenomic next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934473/]
- 40. Metagenomic Next-Generation Sequencing for Diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7066979/]
- 41. Antimicrobial resistance (AMR) [https://www.healthdata.org/research-analysis/health-topics/antimicrobial-resistance-amr]
- 42. Antimicrobial resistance: One Health approach - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9047147/]
- 43. A One Health framework for global and local stewardship ... [https://www.nature.com/articles/s43856-025-01090-4]
- 44. Antimicrobial resistance, equity and justice in low [https://www.nature.com/articles/s41467-025-64137-z]
- 45. Updated WHO dashboard offers new insights on ... [https://www.who.int/news/item/25-09-2025-updated-who-dashboard-offers-new-insights-on-antimicrobial-resistance-and-use]
- 46. Global antibiotic resistance surveillance report 2025 [https://www.who.int/publications/i/item/9789240116337]
- 47. An assessment of antimicrobial resistance national action ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570901/]
- 48. Genomics for antimicrobial resistance—progress and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057382/]
- 49. Genomic and epidemiological characterisation of a dengue ... [https://www.nature.com/articles/s41598-017-15152-8]
- 50. Dengue virus genomic surveillance in the applying ... [https://www.nature.com/articles/s41598-024-78008-y]
- 51. A computational method for the identification of Dengue, Zika ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6527240/]
- 52. Vector surveillance during a major chikungunya outbreak ... [https://www.nature.com/articles/s44298-025-00161-6]
- 53. Enhancing capacities in genomic surveillance capabilities for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11978052/]
- 54. A genome-wide One Health study of Klebsiella ... [https://pubmed.ncbi.nlm.nih.gov/40296028/]
- 55. A genome-wide One Health study of Klebsiella pneumoniae in ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01466-0]
- 56. A One Health approach for the genomic characterization of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1540210/full]
- 57. About the Framework [https://framework.onemilliongenomes.eu/about-the-framework]
- 58. European '1+ Million Genomes' initiative [https://digital-strategy.ec.europa.eu/en/policies/1-million-genomes]
- 59. Beyond One Million Genome plus project launches [https://www.eng.ngc.dk/news/2025/march/beyond-one-million-genome-plus-project-launches]
- 60. Genomics and Bioinformatics in One Health [https://pmc.ncbi.nlm.nih.gov/articles/PMC11507412/]
- 61. Beyond clinical genomics: addressing critical gaps in One ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066572/]
- 62. Computational solutions to large-scale data management and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3124937/]
- 63. Big Data Analytics in Bioinformatics [https://www.hu.ac.ae/knowledge-update/from-different-corners/big-data-analytics-in-bioinformatics]
- 64. How to Perform Large-scale Data Processing in ... [https://medium.com/dnanexus/how-to-perform-large-scale-data-processing-in-bioinformatics-4006e8088af2]
- 65. Using Gviz and Bioconductor | SpringerLink Visualizing Genomic Data [https://link.springer.com/protocol/10.1007/978-1-4939-3578-9_16]
- 66. Ten simple rules for developing visualization tools in genomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9648702/]
- 67. One Health: A Holistic Approach to Tackling Global ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11042131/]
- 68. Systems' Barriers and Facilitators of One Health Programs ... [https://www.sciencedirect.com/science/article/pii/S1201971221011383]
- 69. Multisectoral coordination in public health: insights from the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343634/]
- 70. Barriers and enablers to the implementation of one health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10701386/]
- 71. Beyond clinical genomics: addressing critical gaps in One ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1596720/full]
- 72. Multisectoral collaboration [https://cesh.health/tools-for-action/multisectoral-collaboration]
- 73. “Equity” in genomic health policies: a review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11695411/]
- 74. Bridging the Gap: Addressing Inequalities in Access to ... [https://www.baylorgenetics.com/blog/bridging-the-gap-addressing-inequalities-in-access-to-genetic-testing/]
- 75. Breaking barriers: fostering equitable access to pediatric ... [https://www.nature.com/articles/s41390-025-03859-8]
- 76. SeqFirst: Building equity access to a precise genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11947171/]
- 77. Genomic Data: Innovations and Challenges in 2025 [https://geneyx.com/blog-archive/genomic-data-technology-giants/]
- 78. Increasing the genomic workforce through research ... [https://www.sciencedirect.com/science/article/pii/S0002929725001016]
- 79. Building capacity for genomics in primary care: a scoping ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1577958/full]
- 80. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 81. Increasing Participation in Genomic Research and Biobanking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4815899/]
- 82. FAIR Principles [https://www.go-fair.org/fair-principles/]
- 83. FAIR data [https://en.wikipedia.org/wiki/FAIR_data]
- 84. A Digital One Health framework to integrate data for public ... [https://www.sciencedirect.com/science/article/pii/S2949915123000112]
- 85. FAIR data principles - National Library of Medicine [https://www.nlm.nih.gov/oet/ed/cde/tutorial/02-200.html]
- 86. a systematic review and thematic synthesis - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226485/]
- 87. FAIR原则与数据密集型科学社区应用实践研究 [http://www.jfdc.cnic.cn/CN/abstract/abstract503.shtml]
- 88. Stories of practical implementation of the FAIR principles [https://fair-impact.eu/use-cases]
- 89. Next Course: “Genomics Applied to One Health”, February ... [https://unu.edu/biolac/announcement/next-course-genomics-applied-one-health-february-2026]
- 90. A Comprehensive Guide to Quality Assessment and Data ... [https://pubmed.ncbi.nlm.nih.gov/39235746]
- 91. GHRU Protocols [https://www.pathogensurveillance.net/resources/protocols/]
- 92. Developing a one health data integration framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11841253/]
- 93. One Health implementation: A systematic scoping review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11953970/]
- 94. Table 3 Potential approaches for one health genomic data ... [https://onehealthoutlook.biomedcentral.com/articles/10.1186/s42522-024-00133-5/tables/3]
- 95. Realising a global One Health disease surveillance ... [https://www.nature.com/articles/s41467-024-49417-4]
- 96. An analysis of One Health timeliness metrics across ... [https://www.nature.com/articles/s43856-025-00893-9]
- 97. Mixed-method analysis of published national one health ... [https://www.sciencedirect.com/science/article/pii/S258900422500063X]
- 98. Genomic Predicted cross performance: a tool for optimizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620651/]
- 99. A Quick Comparison of Experimental Results [https://www.chemedx.org/blog/quick-comparison-experimental-results]
- 100. A framework for One Health research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5454183/]
- 101. OH-EpiCap: a semi-quantitative tool for the evaluation of ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.1053986/full]
- 102. OH-EpiCap: a semi-quantitative tool for the evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10213933/]
- 103. Implementation of One Health surveillance systems ... [https://pubmed.ncbi.nlm.nih.gov/38496337/]
- 104. Implementation of One Health surveillance systems [https://www.medrxiv.org/content/10.1101/2023.11.02.23297972v1]
- 105. Users' perception of the OH-EpiCap evaluation tool based ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.1138645/full]
- 106. Enhancing public health surveillance: integrating genomic ... [https://epi.washington.edu/epi_research/enhancing-public-health-surveillance-integrating-genomic-and-epidemiologic-data-to-inform-public-health-action-and-one-health-progress/]
- 107. GAPDC | Genomic Surveillance [https://www.gapdc.org/]
- 108. Advanced tech boosts fight against animal and plant disease [https://www.gov.uk/government/news/advanced-tech-boosts-fight-against-animal-and-plant-disease]