Comparative Genomic Analysis of Bacterial Pathogens: Unveiling Evolution, Resistance, and Precision Targets
This article provides a comprehensive exploration of comparative genomic methodologies and their pivotal role in deciphering the evolution, adaptation, and antimicrobial resistance of bacterial pathogens.
Comparative Genomic Analysis of Bacterial Pathogens: Unveiling Evolution, Resistance, and Precision Targets
Abstract
This article provides a comprehensive exploration of comparative genomic methodologies and their pivotal role in deciphering the evolution, adaptation, and antimicrobial resistance of bacterial pathogens. Tailored for researchers, scientists, and drug development professionals, it synthesizes foundational principles, advanced bioinformatic workflows, and solutions for data challenges. By integrating current case studies—from bovine health to zoonotic diseases—and highlighting validation frameworks, the content establishes how genomic insights are driving the development of targeted therapies, novel antimicrobials, and precision medicine strategies to combat the global threat of antibiotic resistance.
Decoding Pathogen Evolution: Core Principles and Genomic Diversity
Defining Comparative Genomics and Its Impact on Human Health
Comparative genomics is the comparison of genetic information within and across organisms to understand the evolution, structure, and function of genes, proteins, and non-coding regions [1]. This field leverages a variety of tools to compare complete genome sequences of different species, pinpointing regions of similarity and difference to uncover fundamental biological insights [2]. By examining sequences from bacteria to humans, researchers can identify conserved DNA sequences preserved over millions of years, highlighting genes essential to life and genomic signals that control gene function across species [2] [3].
The field has evolved significantly since its origins in the 1980s with comparisons of viral genomes [3]. The first comparative genomic study at a larger scale was published in 1986, comparing the genomes of varicella-zoster virus and Epstein-Barr virus [3]. The completion of the first cellular organism genome (Haemophilus influenzae) in 1995 marked the beginning of modern comparative genomics, where every new genome sequence is now analyzed through this comparative lens [3] [4]. With advances in next-generation sequencing, comparative genomics has become increasingly sophisticated, enabling researchers to deal with many genomes simultaneously and apply these approaches to diverse areas of biomedical research [1] [3].
Key Concepts and Terminology
Understanding comparative genomics requires familiarity with several core concepts and terms that form the foundation of analytical approaches.
Table 1: Fundamental Concepts in Comparative Genomics
| Concept | Definition | Biological Significance |
|---|---|---|
| Orthologs | Genes in different species that evolved from a common ancestral gene by speciation [3] | Often retain the same function in the course of evolution, crucial for functional annotation |
| Paralogs | Genes related by duplication within a genome [3] | May evolve new functions, contributing to functional diversification |
| Synteny | Preserved order of genes on chromosomes of related species [3] | Indicates descent from a common ancestor; identifies conserved genomic regions |
| Pan-genome | The full complement of genes in a species, including core and accessory genes [5] [6] | Core genes often encode essential functions; accessory genes confer niche-specific adaptations |
| Core genome | Genes shared by all strains of a species [5] [6] | Defines species identity and conserved biological functions |
| Accessory genome | Genes present in some but not all strains of a species [6] | Source of genetic variability, often associated with virulence, antibiotic resistance, and niche adaptation |
The principles of evolutionary selection form the theoretical foundation for interpreting comparative genomic data. Elements responsible for similarities between species are conserved through stabilizing selection, while differences result from divergent (positive) selection [3]. Elements unimportant to evolutionary success remain unconserved through neutral selection [3]. This evolutionary framework enables researchers to distinguish functionally important genomic elements from neutral sequences.
Impact on Human Health: Bacterial Pathogen Research
Comparative genomics provides powerful approaches for understanding bacterial pathogenesis, transmission, and treatment. The systematic comparison of bacterial pathogen genomes has yielded significant insights into mechanisms of virulence, antibiotic resistance, and host adaptation.
Understanding Pathogen Evolution and Virulence
Comparative genomic analyses of bacterial pathogens reveal how genetic variation contributes to differences in virulence and host specificity. By comparing genomes of pathogenic and non-pathogenic strains, researchers can identify genetic factors underlying pathogenicity.
Table 2: Key Findings from Comparative Genomic Analyses of Bacterial Pathogens
| Pathogen | Genomic Insight | Impact on Human Health |
|---|---|---|
| Listeria spp. | Absence of LIPI-1, LIPI-2, and LIPI-3 gene islands in non-pathogenic species despite conservation of other virulence genes [7] | Elucidates genetic basis of listeriosis; enables identification of hypervirulent strains |
| W. chitiniclastica | Pan-genome comprises 3,819 genes with 1,622 core genes (43%), indicating metabolic conservation [5] | Reveals evolutionary history of an emerging human pathogen; identifies potential drug targets |
| Multiple pathogens | Accessory genome is source of genetic variability allowing subpopulations to adapt to specific niches [6] | Explains how pathogens evolve to colonize new environments and hosts |
The analysis of Listeria species provides a compelling case study. Comparative genomics of pathogenic (L. monocytogenes, L. ivanovii) and non-pathogenic (L. innocua, L. welshimeri) strains revealed that while all species share many virulence-associated genes, the absence of key pathogenicity islands (LIPI-1, LIPI-2, and LIPI-3) in non-pathogenic species likely explains their reduced virulence despite maintaining adhesion and invasion capabilities in vitro [7]. This demonstrates how comparative genomics can distinguish genuine virulence determinants from ancillary factors.
Antimicrobial Resistance and Therapeutic Development
Comparative genomics plays a crucial role in addressing the global threat of antimicrobial resistance by mapping the resistome - the full complement of antibiotic resistance genes in an organism. The World Health Organization has declared antimicrobial resistance one of the top ten global public health threats, necessitating novel approaches to combat this issue [1].
The analysis of W. chitiniclastica illustrates how comparative genomics reveals resistance mechanisms. While macrolide resistance genes macA and macB are located within the core genome of this species, additional antimicrobial resistance genes for tetracycline, aminoglycosides, sulfonamide, streptomycin, chloramphenicol, and beta-lactamase are distributed among the accessory genome [5]. Notably, the type strain DSM 18708ᵀ does not encode clinically relevant antibiotic resistance genes, whereas drug resistance is increasing within the W. chitiniclastica clade, demonstrating the evolution of resistance in this emerging pathogen [5].
Comparative genomics also facilitates the discovery of novel antimicrobial peptides (AMPs), which are gaining attention as potential therapeutic alternatives to conventional antibiotics. Frogs represent the most studied model organisms for AMPs, with 30% of peptides in the Antimicrobial Peptide Database first identified in frogs [1]. Each frog species possesses a unique repertoire of peptides (usually 10-20) that differs even from closely related species, providing a diverse library of molecules for therapeutic development [1].
Application Notes & Protocols
Protocol: Comparative Genomic Analysis of Bacterial Pathogens
This protocol outlines a comprehensive approach for comparing bacterial pathogen genomes to identify virulence factors, antibiotic resistance genes, and evolutionary relationships.
Materials Required
Table 3: Research Reagent Solutions for Comparative Genomic Analysis
| Reagent/Resource | Function/Application | Example Tools/Databases |
|---|---|---|
| Genomic DNA Extraction Kits | High-quality DNA preparation for sequencing | CTAB method, commercial kits |
| Sequence Databases | Repository of genomic data for comparison | NCBI GenBank, RefSeq [5] |
| Assembly Software | Reconstruction of genome sequences from sequence reads | SPAdes, A5-miseq, Flye, Unicycler [7] |
| Annotation Pipelines | Identification and functional assignment of genomic features | NCBI PGAP, GeneMarkS, tRNAscan-SE [5] [7] |
| Comparative Analysis Tools | Detection of genomic variants, synteny, and evolutionary relationships | MUMMER, OrthoMCL, Roary [3] [6] |
| Specialized Databases | Curated collections of specific gene families | APD, CARD, VFDB [1] |
Methodology
Genome Sequencing and Assembly
- Extract genomic DNA using standardized methods (e.g., CTAB method with modifications) [7]
- Perform whole-genome sequencing using both Illumina (short-read) and Pacific Biosciences (long-read) platforms for complementary coverage
- Assemble sequences using hybrid approaches (e.g., SPAdes for Illumina data, Flye for PacBio data) followed by integration and polishing with tools like Pilon [7]
- Assess assembly quality using metrics (N50, contig number, completeness)
Genome Annotation and Functional Prediction
- Predict protein-coding genes using GeneMarkS or similar tools [7]
- Identify non-coding RNAs using tRNAscan-SE (tRNAs), Barrnap (rRNAs), and Rfam database (other non-coding RNAs) [7]
- Annotate gene functions using multiple databases: GO, KEGG, COG, NR, TCDB, EggNOG, CAZy, Swiss-Prot [7]
- Identify genomic islands using IslandViewer and prophages using PhiSpy [7]
Specialized Annotation for Pathogens
- Annotate virulence factors using specialized databases (VFDB, PATRIC)
- Identify antibiotic resistance genes using resources like CARD
- Characterize mobile genetic elements, CRISPR systems, and restriction-modification systems
Comparative Genomic Analysis
- Perform pan-genome analysis to identify core and accessory genomes using tools like Roary
- Construct phylogenetic trees based on core genome alignments
- Identify structural variants, rearrangements, and synteny breaks using MUMMER and similar tools
- Perform positive selection analysis on specific gene families
Troubleshooting Notes
- For fragmented assemblies, consider increasing sequencing depth or incorporating additional long-read data
- When annotation yields high numbers of "hypothetical proteins," consider using more sensitive homology detection methods (HHblits, PSI-BLAST)
- For phylogenetic inconsistencies, verify orthology relationships and consider horizontal gene transfer events
Protocol: Virulence Gene Identification in Listeria Species
This specific protocol details the identification of virulence determinants in Listeria species through comparative genomics, building on the research by [7].
Experimental Workflow
Detailed Procedures
Bacterial Strains and Growth Conditions
- Obtain pathogenic (L. monocytogenes, L. ivanovii) and non-pathogenic (L. innocua, L. welshimeri) strains
- Culture strains in Brain Heart Infusion (BHI) medium at 37°C overnight with aeration
- Adjust bacterial cultures to OD₆₀₀ = 0.12 for standardized inocula
In vitro Virulence Assays
- Cell Culture: Maintain Caco-2 (human colon carcinoma) and RAW264.7 (macrophage) cells in DMEM with 10% FBS at 37°C with 5% CO₂
- Adhesion Assay:
- Seed cells in 12-well plates at 1×10⁵ cells/well and incubate until confluent
- Wash cells with PBS, add bacterial suspension at MOI of 100:1
- Incubate for 1 hour at 37°C with 5% CO₂
- Wash thoroughly with cold PBS to remove non-adherent bacteria
- Lyse cells with 0.2% Triton X-100, plate serial dilutions on BHI agar
- Calculate adhesion rate: (CFU adhered / Original inoculum CFU) × 100
- Invasion Assay:
- Infect cells as for adhesion assay and incubate for 1 hour
- Wash with PBS, add fresh medium containing 100 µg/mL gentamicin
- Incubate for additional hour to kill extracellular bacteria
- Wash with PBS, lyse cells with 0.2% Triton X-100
- Plate serial dilutions and count CFUs after incubation
- Calculate invasion rate: (CFU invaded / Original inoculum CFU) × 100
Genomic Analysis of Virulence Factors
- Annotate key virulence genes: prfA, plcA, hly, mpl, actA, plcB, inlA, inlB
- Identify presence/absence of pathogenicity islands: LIPI-1, LIPI-2, LIPI-3
- Compare gene organization and synteny in virulence-associated regions
- Perform phylogenetic analysis of virulence genes
Expected Results and Interpretation Pathogenic strains typically show higher adhesion and invasion rates in cellular assays [7]. Genomic analyses should reveal the presence of complete LIPI-1 in pathogenic strains, while non-pathogenic strains lack these key pathogenicity islands despite potentially sharing other virulence-associated genes [7]. Discrepancies between genomic predictions and phenotypic assays may indicate novel virulence mechanisms or regulation differences.
Future Directions in Bacterial Pathogen Genomics
Comparative genomics is evolving rapidly with technological advancements. The NIH Comparative Genomics Resource (CGR) aims to address emerging challenges in data quantity, quality assurance, annotation, and interoperability [1] [8]. As sequencing technologies continue to improve, comparative genomics will expand to include more diverse bacterial pathogens, uncover rare genetic variants, and integrate multi-omics data for a comprehensive understanding of pathogen biology.
The integration of machine learning approaches with comparative genomic data holds particular promise for predicting emerging pathogens, anticipating antibiotic resistance evolution, and identifying novel therapeutic targets. These advances will enhance our ability to respond to infectious disease threats and develop targeted interventions for improved human health.
Bacterial pathogens exhibit a remarkable capacity to colonize diverse hosts and environments through rapid genomic evolution. The primary mechanisms driving this adaptation are gene acquisition via horizontal gene transfer (HGT), gene loss through reductive evolution, and point mutations that fine-tune existing functions [9]. Understanding these processes is crucial for tracking pathogen emergence, predicting virulence, and developing targeted antimicrobial strategies. Comparative genomic studies of bacterial pathogens have revealed that these mechanisms operate differently across ecological niches, with human-associated pathogens often displaying distinct genomic signatures compared to their environmental or animal-associated counterparts [9].
This application note provides a structured framework for investigating these adaptive mechanisms, featuring standardized protocols for experimental evolution, comparative genomics, and functional validation. The integrated approaches outlined below enable researchers to decipher the genetic basis of host specialization, antibiotic resistance emergence, and pathogenicity island acquisition in diverse bacterial systems.
Key Mechanisms of Bacterial Adaptation
Gene Acquisition Through Horizontal Gene Transfer
Horizontal gene transfer enables bacteria to rapidly acquire novel traits through three primary mechanisms: transformation, transduction, and conjugation. This process facilitates the spread of virulence factors, antibiotic resistance genes, and metabolic pathway components across phylogenetic boundaries [10]. Pathogens frequently acquire genomic islands, plasmids, and phage elements that confer immediate selective advantages in new environments.
Research demonstrates that human-associated bacteria, particularly those from the phylum Pseudomonadota, extensively utilize gene acquisition strategies [9]. These organisms show significantly higher frequencies of carbohydrate-active enzyme genes and virulence factors related to immune modulation and adhesion, indicating targeted adaptation to human host environments. The genomic plasticity afforded by HGT enables rapid niche specialization and contributes to the emergence of novel pathogenic variants.
Gene Loss as an Adaptive Strategy
Contrary to traditional views that gene loss is necessarily deleterious, bacteria frequently undergo reductive evolution as an adaptive strategy [9]. This process involves the selective loss of non-essential genes that are redundant or costly in stable environments, allowing resource reallocation to more critical functions.
Mycoplasma genitalium exemplifies this strategy, having undergone extensive genome reduction including the loss of genes involved in amino acid biosynthesis and carbohydrate metabolism [9]. This streamlining enables the bacterium to maintain a parasitic relationship with its host while minimizing metabolic overhead. Comparative genomic analyses reveal that Actinomycetota and certain Bacillota lineages commonly employ genome reduction as an adaptive mechanism during host specialization [9].
Genomic and Metabolic Rearrangements
Beyond discrete gene gains and losses, bacteria undergo substantial genomic rearrangements and metabolic network rewiring during adaptation. These changes include promoter mutations that alter expression patterns, gene duplications that enable functional diversification, and integration of mobile genetic elements that bring new regulatory contexts to existing genes.
Experimental evolution studies with Escherichia coli have demonstrated that long-term adaptation to stable environments produces predictable patterns of genomic evolution, including parallel mutations in global regulators that coordinate metabolic priorities [11]. These regulatory changes often precede structural changes to enzyme-coding sequences, indicating hierarchical adaptation strategies.
Quantitative Analysis of Adaptive Signatures
Table 1: Niche-Specific Genomic Features in Bacterial Pathogens
| Ecological Niche | Enriched Genetic Elements | Primary Adaptive Mechanism | Example Phyla |
|---|---|---|---|
| Human-Associated | Carbohydrate-active enzymes, immune modulation factors, adhesion virulence factors | Gene acquisition through HGT | Pseudomonadota |
| Clinical Settings | Antibiotic resistance genes (particularly fluoroquinolone resistance), efflux pumps | Plasmid-mediated HGT | Multiple phyla |
| Animal Hosts | Reservoirs of resistance genes, host-specific virulence factors | Both HGT and gene loss | Bacillota, Actinomycetota |
| Environmental | Transcriptional regulators, metabolic pathway genes, stress response elements | Gene loss/reductive evolution | Bacillota, Actinomycetota |
Table 2: Detection Methods for Horizontal Gene Transfer Events
| Method Category | Specific Techniques | Primary Applications | Limitations |
|---|---|---|---|
| Sequence Composition-Based | GC content deviation, codon usage bias, k-mer analysis | Initial screening of genomes for putative HGT | Limited detection of ancient transfers |
| Phylogenomic Approaches | Reconciliation of gene and species trees, anomalous phylogenetic patterns | Detecting HGT across deep evolutionary timescales | Computationally intensive |
| Mobile Genetic Element Focused | PlasmidFinder, MobileElementFinder, phage identification tools | Identifying vehicles of recent HGT | May miss chromosomal integrations |
| Experimental Validation | Laboratory evolution with sequencing, functional assays | Confirming adaptive benefit of HGT | May not reflect natural conditions |
Protocols for Studying Adaptation Mechanisms
Protocol: Experimental Evolution to Study Phage Adaptation to New Hosts
This protocol, adapted from Luzon-Hidalgo et al., provides a framework for investigating viral adaptation to novel hosts, with principles applicable to bacterial systems [12].
Research Reagent Solutions
Table 3: Essential Research Reagents for Experimental Evolution
| Reagent/Resource | Specifications | Function in Protocol |
|---|---|---|
| Bacterial Strains | DHB3 (araD139 Δ(ara-leu)7697 ΔlacX74 galE galK rpsL phoR Δ(phoA)PvuII ΔmalF3 thi) | Propagation strain for phage amplification |
| Engineered Host | FA41 cells (thioredoxin minus) cured of F' factor, lysogenized with T7 RNA polymerase | Novel host presenting evolutionary challenge |
| Growth Media | LB broth and LB agar | Standard microbial cultivation |
| Antibiotics | Appropriate selection markers (varies by plasmid system) | Maintenance of engineered genetic elements |
| Plasmids | pET30a(+) derivative with thioredoxin genes under T7 promoter | Expression of alternative proviral factors |
| Phage Stock | Bacteriophage T7 (NCBI reference: NC_001604.1) | Evolving viral entity |
Procedure
I. Phage Amplification and Titer Determination
Bacterial culture preparation: Inoculate 375 μL of an overnight E. coli culture into 15 mL fresh LB broth in a 50 mL tube (1:40 dilution). Incubate with shaking at 37°C until OD₆₀₀ reaches 0.5 (approximately 3-4 hours) [12].
Phage infection: Add 100 μL of phage suspension to 10 mL of the grown bacterial culture. Allow infection to proceed with shaking at 37°C for 4-5 hours until complete lysis is observed.
Phage stock purification: Aliquot bacterial lysate into 1.5 mL tubes and centrifuge at 15,871 × g for 5 minutes at 4°C. Transfer supernatants to new tubes and repeat centrifugation. Pool all supernatents to create a homogeneous amplified phage stock. Store in small aliquots at -20°C to avoid freeze-thaw cycles [12].
Titer determination via plaque assay: Prepare serial dilutions of phage stock in LB broth. Mix 100 μL of each dilution with 100 μL of fresh bacterial culture and 3 mL of molten soft agar (0.5% agar). Pour over pre-warmed LB agar plates and allow to solidify. Incubate overnight at 37°C and count plaque-forming units (pfu) the next day [12].
II. Experimental Evolution Cycles
Initial propagation: Infect the engineered host (containing alternative thioredoxin) with the amplified wild-type phage stock at appropriate multiplicity of infection.
Recovery of evolved variants: Harvest phage progeny after complete lysis or sufficient incubation period (typically 4-24 hours). Purify through centrifugation as described above.
Serial passage: Use progeny from each successful infection to initiate subsequent infection rounds in the novel host. Monitor infection efficiency through plaque assays at regular intervals [12].
Phenotypic characterization: Compare lysis profiles of evolved phages against ancestral strain through one-step growth curves and efficiency of plating assays.
III Genomic Analysis of Adaptations
DNA extraction: Extract genomic DNA from evolved phage suspensions using commercial kits with modifications for viral DNA.
Next-generation sequencing: Prepare libraries and sequence using Illumina platforms (2 × 150 bp paired-end recommended).
Variant identification: Map sequences to reference genome, identify mutations, and validate through Sanger sequencing.
Functional validation: Introduce identified mutations into ancestral background through site-directed mutagenesis to confirm adaptive role.
Protocol: Comparative Genomic Analysis of Bacterial Adaptation
This protocol outlines a bioinformatics workflow for identifying adaptive signatures across bacterial genomes from different ecological niches [9].
Genome Dataset Collection and Curation
Data acquisition: Obtain bacterial genome sequences from public repositories (e.g., NCBI, gcPathogen). Curate metadata to include isolation source, host information, and collection date.
Quality control: Implement stringent filtering criteria including: assembly level (prefer chromosome/scaffold over contig), N50 ≥ 50,000 bp, CheckM completeness ≥ 95%, contamination < 5% [9].
Niche categorization: Annotate genomes with ecological niche labels (human, animal, environment) based on isolation source and host information.
Redundancy reduction: Calculate genomic distances using Mash and perform clustering (e.g., Markov clustering) to remove genomes with distances ≤ 0.01, ensuring non-redundant dataset [9].
Phylogenetic and Population Structure Analysis
Marker gene extraction: Identify 31 universal single-copy genes from each genome using AMPHORA2 [9].
Sequence alignment: Perform multiple sequence alignment for each marker gene using Muscle v5.1.
Phylogenetic reconstruction: Concatenate alignments and construct maximum likelihood tree using FastTree v2.1.11. Visualize through iTOL.
Population clustering: Convert phylogenetic tree to distance matrix and perform k-medoids clustering using silhouette coefficient to determine optimal cluster number [9].
Functional Annotation and Comparative Analysis
Gene prediction: Predict open reading frames using Prokka v1.14.6.
Functional categorization: Map ORFs to Cluster of Orthologous Groups (COG) database using RPS-BLAST (e-value threshold 0.01, minimum coverage 70%).
Specialized annotation:
- Carbohydrate-active enzymes: Annotate using dbCAN2 and HMMER (hmm_eval 1e-5) against CAZy database [9].
- Virulence factors: Query VFDB using Abricate v1.0.1.
- Antibiotic resistance genes: Annotate using CARD database with Abricate or AMRFinderPlus.
Pan-genome analysis: Calculate core and accessory genome using Roary v3.11.2 (≥95% amino acid identity, core gene defined as present in ≥99% isolates).
Association testing: Identify genes significantly associated with specific niches using Scoary with phylogenetic correction.
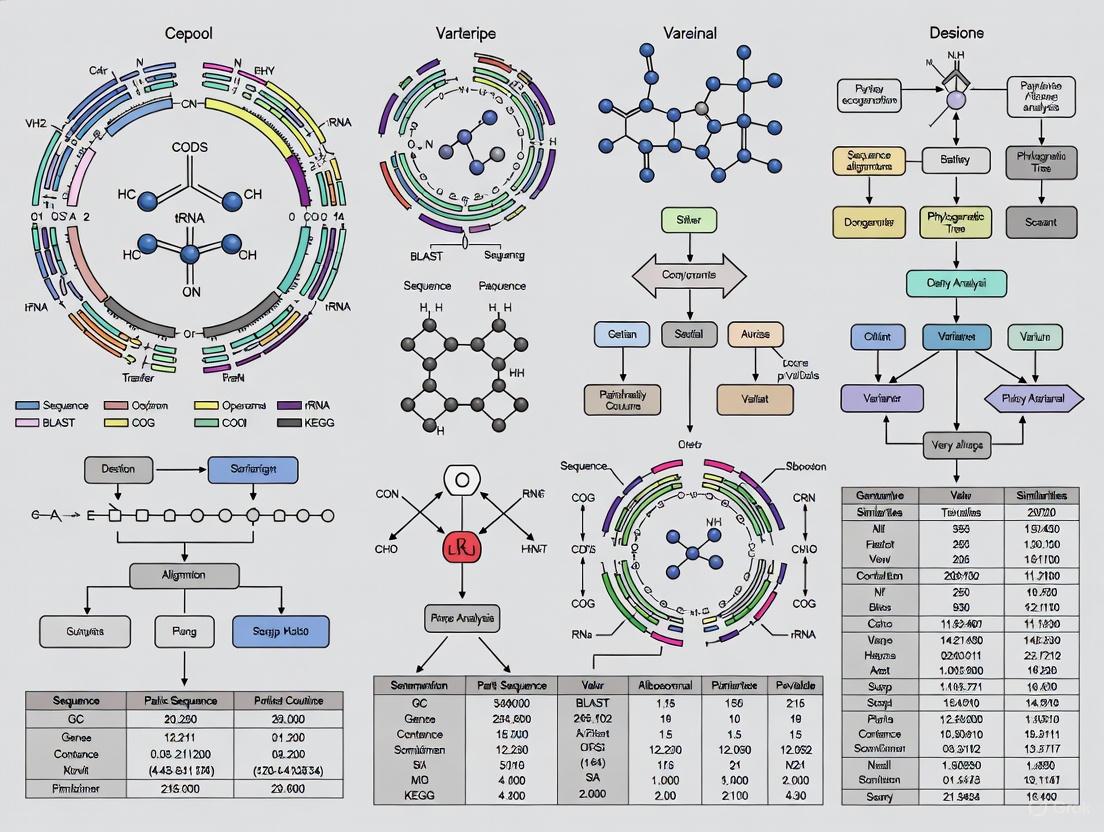
Workflow Visualization
Experimental and Computational Workflow for Studying Bacterial Adaptation
The integrated experimental and computational approaches detailed in this application note provide a comprehensive framework for investigating bacterial adaptation mechanisms. By combining controlled evolution experiments with large-scale comparative genomics, researchers can decipher the genetic basis of host specialization, antibiotic resistance emergence, and niche adaptation in bacterial pathogens.
These protocols have direct applications in public health surveillance, antimicrobial stewardship, and drug development. Identifying niche-specific genetic signatures enables proactive monitoring of zoonotic threats, while understanding adaptation mechanisms informs strategies to counter resistance development. The continued refinement of these methodologies will enhance our predictive capabilities in bacterial evolution and pathogen emergence.
Pan-genome analysis represents a transformative approach in microbial genomics that moves beyond the limitations of single reference genomes to encompass the complete repertoire of genes within a bacterial species. Originally introduced by Tettelin et al. in 2005 during genomic studies of Streptococcus agalactiae, the pan-genome concept has revolutionized how researchers conceptualize bacterial diversity and evolution [13] [14]. For bacterial pathogens, this approach is particularly valuable as it enables systematic investigation of genomic elements underlying virulence, host adaptation, antibiotic resistance, and other clinically relevant traits. The pan-genome is partitioned into distinct components: the core genome (genes shared by all isolates), the dispensable or accessory genome (genes present in some but not all isolates), and strain-specific genes (unique to individual isolates) [14] [15]. This classification provides a powerful framework for understanding the genetic basis of pathogenicity and ecological adaptation.
The importance of pan-genome analysis in bacterial pathogen research stems from its ability to capture the extensive genomic plasticity that characterizes many pathogenic species. Horizontal gene transfer, recombination, and genomic rearrangements contribute significantly to the accessory genome, often encoding functions related to host-pathogen interactions, niche adaptation, and antimicrobial resistance [16] [9]. Recent studies have demonstrated that pathogenic bacteria frequently utilize gene acquisition and loss as evolutionary strategies to adapt to specific host environments and selective pressures, such as antibiotic exposure [9]. For instance, comparative genomic analyses of Pseudomonas aeruginosa isolates from different ecological niches have revealed distinctive genomic signatures associated with human pathogenesis versus environmental survival [9]. By providing a comprehensive view of species-wide genetic diversity, pan-genome analysis enables researchers to identify virulence determinants, track transmission pathways, understand outbreak dynamics, and develop novel therapeutic targets against problematic pathogens.
Computational Methods and Workflows
Pan-Genome Construction Strategies
The construction of a bacterial pan-genome typically employs one of three primary computational approaches, each with distinct advantages and limitations. The reference-based mapping approach aligns sequencing reads from multiple isolates to a high-quality reference genome, identifying presence-absence variations (PAVs) and single nucleotide polymorphisms (SNPs). While computationally efficient, this method is inherently biased toward the reference and may miss novel sequences not present in the reference genome [17] [13]. The de novo assembly approach involves independently assembling complete genomes for multiple isolates followed by comparative analysis to identify core and accessory elements. This method provides more comprehensive variant detection, including structural variations (SVs) in repetitive regions, but demands substantial computational resources and expertise [17] [15]. The graph-based pan-genome approach represents genomic sequences as nodes in a graph structure, with edges connecting overlapping or homologous regions. This method excels at capturing complex structural variations and naturally represents sequence diversity, though graph construction and traversal can be computationally intensive, especially for large datasets [17] [13].
For bacterial pathogens, the choice of construction method depends on research objectives, dataset scale, and computational resources. Reference-based approaches may suffice for closely related isolates of clinical interest, while de novo or graph-based methods are preferable for capturing the full genomic diversity of heterogeneous pathogen populations. A systematic evaluation of available tools indicates that different pipelines vary significantly in their performance characteristics. PGAP2, for instance, employs a fine-grained feature analysis within constrained regions to rapidly and accurately identify orthologous and paralogous genes, demonstrating superior precision and robustness compared to other tools when processing large-scale pan-genome data [16].
Ortholog Identification and Gene Classification
Accurate identification of orthologous genes is fundamental to pan-genome analysis, as errors at this stage propagate through downstream analyses. Most pipelines employ sequence similarity searches (e.g., BLAST, DIAMOND) followed by clustering algorithms (e.g., OrthoFinder, Panaroo) to group homologous genes into orthologous clusters [16] [14]. PGAP2 implements a sophisticated approach that organizes data into gene identity and gene synteny networks, then applies a dual-level regional restriction strategy to refine orthologous gene inference while minimizing computational complexity [16]. This method evaluates gene clusters using three criteria: gene diversity, gene connectivity, and the bidirectional best hit (BBH) criterion for duplicate genes within the same strain [16].
Following ortholog identification, genes are classified into categories based on their distribution patterns across the analyzed genomes. The standard classification system includes core genes (present in all isolates, typically encoding essential cellular functions), soft-core genes (present in ≥95% of isolates), shell genes (present in 15-95% of isolates), and cloud genes (present in <15% of isolates, often strain-specific) [14] [15]. Some classification systems also include private genes that are unique to a single isolate [14]. These categories provide insights into evolutionary conservation and functional specialization within bacterial populations.
Table 1: Standard Gene Categories in Bacterial Pan-Genome Analysis
| Category | Presence Threshold | Typical Functional Enrichment | Evolutionary Characteristics |
|---|---|---|---|
| Core Genes | 100% of isolates | Primary metabolism, DNA replication, transcription, translation | Evolutionarily conserved, vertical inheritance |
| Soft-Core Genes | ≥95% of isolates | Metabolic flexibility, regulatory functions | Highly conserved with minor population-specific variation |
| Shell Genes | 15-95% of isolates | Environmental sensing, niche adaptation, antimicrobial resistance | Subject to frequent gain/loss, often linked to mobile elements |
| Cloud Genes | <15% of isolates | Phage-related functions, hypothetical proteins | Recently acquired, strain-specific, potentially transient |
| Private Genes | Single isolate | Horizontal acquisitions, strain-specific adaptations | Recently acquired, may represent annotation artifacts |
Workflow Visualization
The following diagram illustrates a generalized computational workflow for bacterial pan-genome analysis, integrating the key steps from data preparation through downstream applications:
Application Notes for Bacterial Pathogen Research
Protocol 1: Comparative Genomic Analysis of Pathogen Populations
Objective: To identify genomic features associated with host adaptation and virulence in bacterial pathogens across different ecological niches.
Materials and Reagents:
- High-quality genome assemblies for multiple bacterial isolates (minimum 10-15 recommended)
- High-performance computing infrastructure with sufficient memory and storage
- Bioinformatic software tools (see Table 2)
Methodology:
- Dataset Curation and Quality Control: Collect genome sequences with comprehensive metadata including isolation source, host information, geographical location, and collection date. Implement stringent quality control measures including CheckM evaluation (completeness ≥95%, contamination <5%) and removal of highly similar strains (genomic distance ≤0.01) to reduce redundancy [9].
- Pan-Genome Construction: Utilize PGAP2 or similar pipelines that accept multiple input formats (GFF3, GBFF, FASTA). PGAP2 automatically selects a representative genome based on gene similarity and identifies outliers using average nucleotide identity (ANI) thresholds and unique gene counts [16].
- Functional Annotation: Annotate protein-coding genes using Prokka or similar tools. Map predicted open reading frames to functional databases including COG (cellular functions), dbCAN2 (carbohydrate-active enzymes), VFDB (virulence factors), and CARD (antibiotic resistance genes) using sequence similarity searches with appropriate e-value thresholds (e.g., 0.01) and coverage filters [9].
- Statistical Analysis: Calculate pan-genome characteristics including core/accessory proportions and gene presence-absence frequencies. Perform enrichment analysis using Fisher's exact tests or hypergeometric tests to identify functions overrepresented in specific phylogenetic clades or ecological niches. Apply machine learning algorithms (e.g., random forests) to identify genomic features predictive of host specificity or clinical outcomes [9].
Expected Outcomes: This protocol enables identification of niche-specific genomic signatures, including enrichment of virulence factors in clinical isolates, antibiotic resistance genes in hospital-associated strains, and metabolic adaptations in environmental populations. A recent study applying this approach to 4,366 bacterial pathogens revealed that human-associated Pseudomonadota exhibited higher frequencies of carbohydrate-active enzyme genes and immune evasion factors, while environmental isolates showed greater enrichment of metabolic and transcriptional regulatory genes [9].
Protocol 2: Identification of Antimicrobial Resistance and Virulence Determinants
Objective: To characterize the distribution and genetic context of antimicrobial resistance (AMR) genes and virulence factors across pathogen populations.
Materials and Reagents:
- Bacterial genomes with associated antimicrobial susceptibility profiles
- Reference databases: CARD, VFDB, NCBI AMRFinderPlus
- Visualization tools: Phandango, BRIG, Proksee
Methodology:
- Gene Detection: Identify AMR genes and virulence factors using a combination of sequence similarity (BLAST, DIAMOND) and hidden Markov model (HMM) approaches against specialized databases. For comprehensive AMR annotation, use tools like RGI (Resistance Gene Identifier) with the CARD database.
- Contextual Analysis: Examine genomic neighborhoods of identified AMR/virulence genes to determine their association with mobile genetic elements (plasmids, transposons, integrons) using tools like MobileElementFinder.
- Association Testing: Correlate gene presence-absence patterns with metadata on antibiotic resistance phenotypes, host specificity, or clinical manifestations using statistical tests (e.g., Fisher's exact test) and phylogenetic methods to account for population structure.
- Visualization: Generate circular genome comparisons to visualize the distribution and genomic context of AMR/virulence genes across multiple isolates.
Expected Outcomes: This protocol facilitates tracking of mobile resistance elements across pathogen populations, identification of emerging resistance threats, and discovery of novel virulence mechanisms. Application to clinical Streptococcus suis isolates has revealed extensive variation in virulence gene content associated with differential disease outcomes [16].
Table 2: Essential Computational Tools for Bacterial Pan-Genome Analysis
| Tool Category | Specific Tools | Primary Function | Application Notes |
|---|---|---|---|
| Genome Assembly | Hifiasm, Unicycler, SPAdes | De novo genome assembly from sequencing reads | Critical for generating high-quality inputs; long-read technologies improve contiguity |
| Annotation | Prokka, Bakta, RAST | Structural and functional gene annotation | Standardized annotation essential for comparative analyses |
| Ortholog Identification | OrthoFinder, Roary, Panaroo, PGAP2 | Homology detection and orthologous group clustering | PGAP2 shows superior accuracy for large datasets [16] |
| Variant Analysis | Snippy, Breseq, SVcaller | SNP and structural variant detection | Important for understanding microevolution within species |
| Functional Analysis | eggNOG-mapper, COG, dbCAN2 | Functional annotation and enrichment | Links genomic variation to biological processes |
| Specialized Databases | VFDB, CARD, dbCAN | Pathogen-specific functional annotation | Essential for virulence and resistance profiling |
| Visualization | Phandango, ITOL, PanX | Interactive visualization of pan-genomes | Facilitates exploration and interpretation of results |
Research Reagent Solutions
Successful pan-genome analysis requires both computational tools and carefully curated biological materials. The following table outlines essential research reagents and resources for comprehensive pan-genome studies of bacterial pathogens:
Table 3: Essential Research Reagents and Resources for Bacterial Pan-Genome Analysis
| Reagent/Resource | Specifications | Function in Pan-Genome Analysis | Quality Control Considerations |
|---|---|---|---|
| Bacterial Isolates | Diverse ecological/geographical origins; comprehensive metadata | Represents species genetic diversity; enables correlation of genomic features with phenotype | Purity verification; contamination screening; accurate source documentation |
| DNA Extraction Kits | High-molecular-weight DNA suitable for long-read sequencing | Input material for high-quality genome assemblies | Quantification (fluorometric); integrity assessment (pulse-field gel electrophoresis) |
| Sequencing Platforms | Illumina (coverage), PacBio HiFi/Nanopore (contiguity) | Generates raw data for assembly and variant detection | Appropriate coverage depth (typically 50-100x for Illumina, 20-30x for long reads) |
| Reference Genomes | High-quality, complete assemblies with annotation | Basis for reference-based approaches; functional inference | Assessment of completeness (BUSCO), continuity (N50), annotation quality |
| Functional Databases | COG, KEGG, VFDB, CARD, dbCAN | Functional annotation of gene clusters | Regular updates; careful curation to minimize false annotations |
| Computational Infrastructure | High-performance computing cluster with ample storage | Data processing, analysis, and storage | Sufficient RAM for large assemblies; backup systems for data preservation |
Data Interpretation and Analytical Considerations
Statistical Framework and Quantitative Parameters
Pan-genome analysis generates complex datasets that require appropriate statistical frameworks for robust interpretation. A key initial consideration is determining whether the pan-genome is "open" or "closed" using Heaps' law, which models the relationship between newly sequenced genomes and novel gene discovery [15]. The mathematical formulation follows the power-law function: $n = kN^α$, where $n$ represents the total number of unique genes identified after sequencing $N$ genomes, $k$ is a constant reflecting vocabulary growth rate, and $α$ indicates pan-genome openness [15]. An $α$ value >1 typically suggests an open pan-genome where new genes continue to be discovered with additional sequencing, while $α$ <1 indicates a closed pan-genome where sequencing additional isolates yields diminishing returns in novel gene discovery.
PGAP2 introduces four quantitative parameters derived from inter- and intra-cluster distances that enable detailed characterization of homology clusters [16]. These metrics facilitate more nuanced interpretations of pan-genome dynamics beyond simple presence-absence counts. For phylogenetic analysis, maximum likelihood trees constructed from concatenated alignments of universal single-copy genes provide robust evolutionary frameworks for interpreting the distribution of accessory genes [9]. Population genetic statistics such as nucleotide diversity (π) and fixation indices (FST) can further illuminate population structure and selection pressures acting on different genomic compartments [9].
Technical Challenges and Limitations
Despite methodological advances, bacterial pan-genome analysis still faces several technical challenges. The quality of input genomes significantly impacts results, with fragmented assemblies or incomplete annotations leading to inaccurate gene presence-absence calls [15]. Highly repetitive regions, mobile genetic elements, and recent gene duplications present particular difficulties for orthology detection algorithms [16]. For accessory genes with patchy distributions, distinguishing genuine biological absence from assembly or annotation artifacts remains challenging; integration with transcriptomic data can help validate functionally expressed genes [15].
Computational resource requirements can be substantial, particularly for graph-based approaches analyzing hundreds or thousands of genomes [17]. The choice of clustering thresholds significantly impacts gene categorization, yet optimal settings vary across bacterial taxa due to differences in evolutionary rates and genome dynamics [14]. Pan-genome analyses are also sensitive to sampling bias, where overrepresentation of certain lineages (e.g., clinical isolates versus environmental strains) can skew estimates of core and accessory genome sizes [9]. Careful study design incorporating phylogenetically diverse isolates with comprehensive metadata collection helps mitigate these limitations and enables more biologically meaningful interpretations.
Pan-genome analysis has emerged as an indispensable framework for comparative genomics of bacterial pathogens, providing unprecedented insights into their evolutionary dynamics, adaptive mechanisms, and pathogenic potential. The protocols and methodologies outlined in this article equip researchers with standardized approaches for constructing and analyzing pan-genomes to address diverse microbiological questions. As sequencing technologies continue to advance and computational methods become more sophisticated, pan-genome approaches will play an increasingly central role in tracking the emergence and spread of antimicrobial resistance, identifying novel therapeutic targets, informing vaccine design, and ultimately improving our ability to combat infectious diseases. The integration of pan-genomics with functional studies, population genomics, and epidemiological data represents a promising frontier for understanding the genetic basis of pathogenicity and developing novel interventions against problematic pathogens.
Bovine mastitis, an inflammatory condition of the mammary gland, presents a substantial economic burden to the global dairy industry, with annual losses estimated between USD 19.7 and 32 billion [18]. Staphylococcus aureus and Escherichia coli represent two of the most significant bacterial pathogens responsible for clinical and subclinical mastitis cases worldwide. This application note explores the genomic diversity of these pathogens through the lens of comparative genomic analysis, providing researchers with standardized protocols and analytical frameworks to investigate mastitis pathogenesis, transmission dynamics, and antimicrobial resistance patterns. The insights derived from such analyses are crucial for developing targeted interventions and improving bovine health management practices in dairy production systems.
Genomic Profiles of Major Mastitis Pathogens
1Staphylococcus aureusGenomic Epidemiology
Staphylococcus aureus demonstrates significant genomic plasticity with distinct clonal complexes (CCs) dominating bovine mastitis cases across different geographical regions. Comparative genomic studies reveal specific adaptations in bovine-associated lineages.
Table 1: Global Distribution of S. aureus Clonal Complexes in Bovine Mastitis
| Clonal Complex | Geographical Distribution | Associated Mastitis Type | Key Virulence Factors | Antimicrobial Resistance Profile |
|---|---|---|---|---|
| CC151 [19] | Widespread (29.3% European isolates) [19] | Subclinical and Clinical [19] | lukM-lukF', Various superantigens [19] | Limited AMR genes [19] |
| CC97 [20] [19] | Prevalent in India and Europe (19.6%) [20] [19] | Subclinical and Clinical [19] | Moderate lukM-lukF' carriage (30%) [19] | blaZ (30%) [19] |
| CC479 [19] | Regional (11.6% European isolates) [19] | Associated with Clinical Mastitis (OR 3.62) [19] | lukM-lukF', SaPI vWFbp, Superantigens [19] | Limited AMR genes [19] |
| CC398 [19] | Poland and Spain [19] | Subclinical and Clinical [19] | Lacks key virulence factors [19] | High blaZ, tetM, mecA carriage [19] |
| CC8 [20] | India and Europe [20] [19] | Subclinical and Clinical [19] | Variable [19] | Variable [19] |
2Escherichia coliGenomic Epidemiology
Mammary pathogenic E. coli (MPEC) strains display a distinct phylogenetic distribution compared to human pathogenic variants, with specific genetic loci associated with adaptation to the bovine mammary environment.
Table 2: Characteristics of Mastitis-Associated Escherichia coli (MPEC)
| Characteristic | Profile | Significance |
|---|---|---|
| Phylogroup Distribution [21] [22] | Primarily Phylogroup A and B1 [21] [22] | Contrasts with human extraintestinal pathogenic E. coli (ExPEC) which often belong to groups B2 and D [21] |
| Virulence Gene Carriage [21] | Few recognized virulence genes from other pathogenic pathovars [21] | Suggests niche-specific adaptation factors rather than conventional virulence genes |
| MPEC-Specific Loci [22] | ycdU-ymdE genes, phenylacetic acid degradation pathway, ferric citrate uptake system [22] | Identified through pan-genomic analysis as core to MPEC but dispensable in other E. coli [22] |
| Phylogenetic Diversity [22] | Significantly reduced compared to general phylogroup A population (p = 0.00015) [22] | Indicates selective enrichment of specific lineages capable of causing mastitis [22] |
Experimental Protocols for Genomic Analysis
Whole Genome Sequencing and Assembly Protocol
Objective: Obtain high-quality genome sequences for comparative genomic analysis of mastitis pathogens.
Materials:
- Bacterial isolates from clinical or subclinical mastitis milk samples
- DNeasy Blood and Tissue Kit (Qiagen) or equivalent [23] [20]
- Illumina sequencing platform (HiSeq, NextSeq) [23] [20]
- Computational resources with at least 16GB RAM
Procedure:
DNA Extraction
- Grow bacterial isolates overnight in appropriate medium (e.g., BHI broth for S. aureus)
- Extract genomic DNA using commercial kits following manufacturer's protocol
- Assess DNA quality and quantity using spectrophotometry (e.g., Nanodrop) and fluorometry (e.g., Qubit)
- Ensure DNA integrity by agarose gel electrophoresis
Library Preparation and Sequencing
- Fragment DNA to ~500bp using acoustic shearing or enzymatic fragmentation
- Prepare sequencing libraries using Illumina-compatible library preparation kits
- Perform quality control on libraries using Bioanalyzer or TapeStation
- Sequence on Illumina platform to achieve minimum 50x coverage (2×150bp paired-end recommended)
Genome Assembly and Annotation
Troubleshooting Tips:
- Low coverage: Check DNA quality and optimize fragmentation
- Poor assembly: Increase sequencing depth or employ hybrid assembly approaches
- Contamination: Screen for non-target DNA using 16S rRNA analysis
Comparative Genomic Analysis Protocol
Objective: Identify variations in gene content, phylogenetic relationships, and virulence determinants among mastitis isolates.
Materials:
- Assembled and annotated genome sequences
- Reference genomes (e.g., S. aureus strain K5 for SNP calling) [20]
- Computational resources with Linux environment and appropriate software
Procedure:
Pan-Genome Analysis
Multilocus Sequence Typing (MLST)
Virulence and Resistance Gene Profiling
Single Nucleotide Polymorphism (SNP) Analysis
Expected Outcomes:
- Pan-genome statistics (core, accessory, and unique gene counts)
- Phylogenetic relationships and population structure
- Virulence and resistance gene profiles associated with specific lineages
- Identification of genetic markers for mastitis-associated clones
Visualization of Genomic Analysis Workflow
Genetic Basis of Mastitis Pathogenesis
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Mastitis Pathogen Genomics
| Reagent/Resource | Function | Example/Specification |
|---|---|---|
| DNA Extraction Kit [23] [20] | High-quality genomic DNA isolation | DNeasy Blood and Tissue Kit (Qiagen) or equivalent |
| Library Prep Kit [23] | Sequencing library preparation | Illumina DNA Prep kits or equivalent |
| Sequencing Platform [23] [20] | Whole genome sequencing | Illumina HiSeq/NextSeq for short-read; PacBio/Oxford Nanopore for long-read |
| Assembly Software [23] [20] | Genome assembly from sequencing reads | SPAdes v3.11.1+ for Illumina data |
| Annotation Tools [23] [20] | Gene prediction and functional annotation | PROKKA, RAST |
| Typing Databases [20] | Strain classification and epidemiology | PubMedST for MLST analysis |
| Specialized Databases [23] [20] | Virulence and resistance gene identification | CARD (AMR), VFDB (Virulence Factors) |
| Phylogenetic Tools [23] [20] | Evolutionary relationship inference | kSNP v.3 (SNP-based), Roary (gene presence/absence) |
Discussion and Research Implications
The comparative genomic analysis of bovine mastitis pathogens reveals distinct evolutionary strategies employed by S. aureus and E. coli to colonize the bovine mammary gland. S. aureus exhibits a clonal population structure with specific CCs enriched in virulence factors that promote immune evasion and persistence, such as the ruminant-specific leukocidin LukMF' [19] [18]. In contrast, MPEC strains are characterized not by conventional virulence factors but by niche-specific adaptations including specialized iron acquisition systems and metabolic pathways [21] [22].
From a diagnostic perspective, the identification of CC-specific markers in S. aureus and MPEC-specific loci in E. coli enables development of rapid molecular tests to identify high-risk strains. For instance, the detection of CC479 S. aureus, which is strongly associated with clinical mastitis (OR 3.62) [19], could inform targeted intervention strategies. Similarly, the ferric citrate uptake system in MPEC represents a potential therapeutic target for novel interventions.
The regional variation in dominant clones, with CC97 prevalent in Indian isolates [20] and CC151 widespread in Europe [19], highlights the importance of geographic factors in strain distribution and the necessity for region-specific control strategies. Furthermore, the emergence of antimicrobial resistance in certain lineages, particularly the high prevalence of tetracycline resistance (tetM) and methicillin resistance (mecA) in CC398 [19], underscores the need for continuous genomic surveillance to monitor the spread of resistant clones.
These genomic insights facilitate a more precise approach to mastitis management through improved diagnostics, targeted therapies, and evidence-based control measures, ultimately reducing the economic impact of this disease while promoting antimicrobial stewardship in dairy production systems.
Regional Variations and Host-Specific Adaptations in Pathogen Populations
Understanding the genetic mechanisms behind regional variations and host-specific adaptations is a fundamental objective in bacterial pathogen research. Pathogens exhibit a remarkable capacity to evolve distinct genomic features in response to selective pressures imposed by different ecological niches and host organisms [9]. Comparative genomic analyses have revealed that bacterial pathogens employ diverse adaptive strategies, including gene acquisition through horizontal gene transfer and reductive evolution through gene loss, to specialize for survival in specific environments [9] [25]. The significance of this research is framed within the One Health approach, which recognizes the complex interdependencies connecting human, animal, and environmental health [9].
Large-scale genomic studies demonstrate that human-associated bacteria, particularly from the phylum Pseudomonadota, frequently acquire genes encoding carbohydrate-active enzymes and virulence factors related to immune modulation and adhesion, indicating a pattern of co-evolution with the human host [9] [25]. In contrast, environmental isolates often show enrichment in genes for metabolic versatility and transcriptional regulation, while clinical settings select for elevated numbers of antibiotic resistance genes [9]. This Application Note provides a structured genomic framework, detailed protocols, and analytical tools to investigate these critical adaptive mechanisms, enabling researchers to decipher the molecular basis of pathogen evolution and transmission dynamics.
Key Genomic Findings on Niche Adaptation
Comparative analysis of 4,366 high-quality bacterial genomes has quantified significant genomic differences across ecological niches. The table below summarizes the key adaptive signatures identified in major bacterial phyla from different sources [9].
Table 1: Niche-Specific Genomic Adaptations Across Bacterial Phyla
| Ecological Niche | Primary Adaptive Strategy | Enriched Gene Categories | Representative Pathogens |
|---|---|---|---|
| Human Host | Gene acquisition | Carbohydrate-active enzymes (CAZymes), virulence factors (immune modulation, adhesion) | Pseudomonas aeruginosa, Escherichia coli [9] [25] |
| Animal Host | Gene acquisition & reservoir function | Virulence factors, antibiotic resistance genes | Staphylococcus aureus (livestock-associated) [9] |
| Clinical Environment | Gene acquisition (antibiotic resistance) | Fluoroquinolone resistance genes, other AMR determinants | Multidrug-resistant P. aeruginosa [9] [26] |
| Natural Environment | Genome reduction & metabolic diversification | Metabolic pathways, transcriptional regulation | Vibrio parahaemolyticus environmental ecotypes [9] |
Further analysis at the species level reveals specific genetic changes driving host preference. Studies on Pseudomonas aeruginosa epidemic clones have identified a transcriptional signature of 624 genes positively associated and 514 genes inversely associated with an affinity for causing cystic fibrosis (CF) infections [26]. A key finding is the role of the stringent response modulator DksA1, whose expression is linked to enhanced intracellular survival within macrophages, a trait critical for persistence in CF patients [26]. This highlights how specific regulatory genes can underpin host-specific adaptation and virulence.
Application Notes: Experimental Framework for Analyzing Host Adaptation
Core Computational and Genomic Workflow
A robust experimental framework for analyzing host adaptation involves a sequential process from genome collection to functional validation. The following workflow outlines the key stages for identifying and characterizing niche-specific signature genes.
Figure 1: A unified workflow for the comparative genomic analysis of host adaptation.
Protocol: Comparative Genomic Analysis for Identifying Host-Specific Adaptations
Objective: To identify niche-associated signature genes and genomic adaptations in bacterial pathogens from different hosts and environments.
Materials and Reagents:
- High-quality bacterial genome sequences
- High-performance computing (HPC) cluster or server
- Bioinformatic software suites (detailed in Section 5.0)
Procedure:
Genome Dataset Curation and Quality Control
- Source genome metadata from public databases (e.g., gcPathogen) [9].
- Apply stringent quality filters: retain genomes with assembly N50 ≥ 50,000 bp, CheckM completeness ≥ 95%, and contamination < 5% [9] [25].
- Annotate each genome with an ecological niche label ("human," "animal," "environment") based on isolation source metadata [9].
- Remove redundant genomes by calculating genomic distances with Mash and performing clustering (e.g., remove genomes with distance ≤ 0.01) to obtain a non-redundant dataset [9].
Phylogenetic Reconstruction and Population Clustering
- Identify 31 universal single-copy genes from each genome using AMPHORA2 [9].
- Perform multiple sequence alignment for each marker gene using Muscle v5.1 [9].
- Concatenate alignments and construct a maximum likelihood phylogenetic tree using FastTree v2.1.11 [9].
- Convert the phylogenetic tree into an evolutionary distance matrix and perform k-medoids clustering (e.g., using the
pamfunction in R) to define population clusters for downstream comparative analysis [9].
Functional Annotation and Enrichment Analysis
- Predict Open Reading Frames (ORFs) using Prokka v1.14.6 [9] [25].
- Annotate gene functions by mapping ORFs to the following databases:
- COG Database: Use RPS-BLAST (e-value threshold 0.01, minimum coverage 70%) for functional categorization [9].
- CAZy Database: Use dbCAN2 (HMMER tool, hmm_eval 1e-5) to annotate carbohydrate-active enzyme genes [9].
- Virulence Factors: Use ABRicate v1.0.1 with the Virulence Factor Database (VFDB) to identify virulence genes [9] [25].
- Antibiotic Resistance: Use ABRicate with the CARD database to identify antimicrobial resistance genes [9].
- Perform enrichment analysis (e.g., Fisher's exact test) to identify COG categories, virulence factors, and resistance genes significantly overrepresented in specific ecological niches [9].
Identification of Host-Specific Signature Genes
Application Notes: Investigating Intrinsic Host Preference and Transmission
Core Workflow for Analyzing Epidemic Clone Behavior
Understanding why certain epidemic clones exhibit a strong preference for a specific host requires moving beyond genomics to transcriptomics and phenotypic assays. The process below details the key steps for this functional investigation.
Figure 2: A functional analysis workflow for intrinsic host preference mechanisms.
Protocol: Functional Characterization of Host Preference Mechanisms
Objective: To determine the molecular basis for the intrinsic preference of epidemic bacterial clones for specific host types (e.g., Cystic Fibrosis vs. non-CF patients).
Materials and Reagents:
- Representative bacterial isolates from defined epidemic clones (e.g., high-CF-affinity ST27 vs. low-affinity ST235)
- Wild-type and CF (e.g., F508del homozygous) isogenic macrophage cell lines
- Cell culture materials and invasion media
- Zebrafish model for in vivo infection studies
- Materials for genetic manipulation (e.g., knockout plasmids)
Procedure:
Transcriptomic Profiling of Epidemic Clones
- Culture representative isolates from epidemic clones with known host preferences under standardized conditions.
- Extract total RNA and perform RNA-Seq analysis.
- Identify differentially expressed genes between clones with high and low affinity for a specific host (e.g., CF) using a negative binomial generalized linear model (Wald test, FDR = 0.05) [26].
Phenotypic Screening Using Macrophage Survival Assay
- Differentiate human THP-1 cells into macrophages.
- Infect macrophages with bacterial isolates at a defined Multiplicity of Infection (MOI).
- After a set period of incubation, lyse the macrophages and plate the lysates on agar to enumerate intracellular bacteria.
- Compare the intracellular survival and replication rates of isolates from high- and low-affinity clones [26].
Genetic Validation of Key Regulatory Genes
- Select a candidate gene identified from transcriptomic analysis (e.g., dksA1).
- Construct a knockout mutant (e.g., ΔdksA1,2 double knockout) in a wild-type background (e.g., PAO1) [26].
- Complement the mutant by reintroducing the wild-type gene on a plasmid.
- Repeat the macrophage survival assay with the wild-type, knockout, and complemented strains to confirm the gene's role in intracellular survival, particularly in CF macrophage models [26].
In Vivo Validation in Animal Models
- Use a zebrafish model with morpholino knockdown of the cftr gene to simulate a CF-like environment.
- Inject wild-type and mutant bacterial strains intravenously and monitor host survival and bacterial burden over time to validate findings from in vitro models [26].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Computational Tools for Comparative Genomics
| Item Name | Function/Application | Specific Example/Version |
|---|---|---|
| Prokka | Rapid annotation of bacterial genomes [9]. | v1.14.6 |
| dbCAN2 | Annotation of carbohydrate-active enzymes in genomes [9]. | HMMER tool (hmm_eval 1e-5) |
| VFDB | Database for identifying virulence factors [9]. | Used with ABRicate v1.0.1 |
| CARD | Database for predicting antibiotic resistance genes [9]. | Used with ABRicate v1.0.1 |
| Scoary | Pan-genome genome-wide association study (GWAS) tool [9]. | Used to identify niche-associated genes |
| Panaroo | Graph-based pangenome clustering and analysis [26]. | Used to define core/accessory genome |
| Support Vector Machine (SVM) | Machine learning model for pathogenicity classification [9] [27]. | L1-norm regularization for feature selection |
| THP-1 Cell Line | Human monocyte cell line, differentiated into macrophages for infection assays [26]. | Wild-type and CF (F508del) isogenic lines |
| Zebrafish Model | In vivo model for studying host-pathogen interactions and virulence [26]. | cftr morpholino knockdown |
From Sequence to Insight: Advanced Workflows and Biomedical Applications
High-quality genome curation represents a critical foundation for comparative genomic analyses of bacterial pathogens, enabling researchers to decipher the genetic underpinnings of virulence, antimicrobial resistance, and host adaptation. The process transforms raw sequence data into biologically meaningful information through systematic annotation, validation, and functional classification. Within bacterial pathogen research, meticulous curation is particularly vital as it directly impacts the identification of therapeutic targets, understanding of transmission dynamics, and development of diagnostic tools. Current genomic resources have evolved significantly to support these investigations, with international databases maintaining standardized information on millions of microbial sequences [28]. The establishment of consistent curation standards ensures that data remains interoperable across platforms, reproducible across studies, and biologically accurate for downstream analyses, ultimately strengthening the reliability of scientific findings in infectious disease research.
The burgeoning volume of genomic data from advanced sequencing technologies presents both unprecedented opportunities and substantial challenges for pathogen genomics. As noted in a comprehensive analysis of 4,366 bacterial pathogen genomes, rigorous quality control and standardized annotation pipelines are essential for meaningful comparative studies [9]. The integration of curated metadata regarding isolation source, host information, and collection date further enhances the utility of these genomic resources for tracking disease outbreaks and understanding pathogen evolution. This application note details the contemporary standards, databases, and methodological frameworks that underpin high-quality genome curation, with specific emphasis on applications in bacterial pathogen research.
A diverse ecosystem of databases supports the storage, retrieval, and analysis of curated bacterial genomic data. These resources vary in scope, specialization, and data access mechanisms, each contributing unique elements to the pathogen genomics research landscape. Understanding their respective strengths and appropriate use cases is fundamental for effective genomic investigation.
Major Primary Data Repositories include the International Nucleotide Sequence Database Collaboration (INSDC) members, which provide comprehensive archival services for raw sequence data and genome assemblies. GenBank at NCBI, the European Nucleotide Archive (EMBL-EBI), and the DNA Data Bank of Japan (DDBJ) exchange data daily to ensure global coverage [28]. These repositories accept submissions with minimal curation barriers but apply standardized annotation pipelines to enhance consistency. Specialized resources like the NIH Genetic Testing Registry (GTR) and ClinVar focus specifically on clinically relevant variants, providing structured evidence frameworks for interpreting pathogenicity [29]. ClinVar has recently been updated to support classifications of both germline and somatic variants, enhancing its utility for bacterial pathogen research that differentiates between inherited characteristics and acquired mutations [28].
Value-Added and Specialized Databases apply additional layers of curation, often integrating multiple data types or focusing on specific research domains. RefSeq provides non-redundant reference sequences that leverage both computational and expert curation to produce high-quality genomic, transcript, and protein references [28]. The Clinical Genome Resource (ClinGen), an NIH-funded initiative, offers structured frameworks for evaluating gene-disease relationships and variant pathogenicity through expert panels [30]. For metagenomic-assembled genomes (MAGs), resources like MAGdb provide curated collections of high-quality MAGs with standardized metadata, specifically focusing on genomes meeting minimum information standards [31]. The database contains 99,672 high-quality MAGs with manually curated metadata from clinical, environmental, and animal sources, providing a valuable resource for discovering novel microbial lineages and understanding their ecological roles [31].
Table 1: Major Genomic Databases for Bacterial Pathogen Research
| Database | Primary Focus | Key Features | Data Volume (2025) |
|---|---|---|---|
| GenBank | Nucleotide sequences | INSDC member, daily data exchange with ENA and DDBJ | 34 trillion base pairs, 4.7 billion sequences, 581,000 species [28] |
| RefSeq | Reference sequences | Expert curation, non-redundant, integrated with NCBI tools | Spanning tree of life [28] |
| ClinVar | Human variants | Clinical significance, supporting evidence, germline/somatic classifications | >3 million variants from >2800 organizations [28] |
| PubChem | Chemical compounds | Bioactivity data, substance-compound-bioassay relationships | 119 million compounds, 322 million substances [28] |
| MAGdb | Metagenome-assembled genomes | Quality-controlled MAGs, standardized metadata | 99,672 high-quality MAGs from 13,702 samples [31] |
Quality Control Standards and Metrics
Implementing rigorous quality control measures is paramount for ensuring the reliability of genomic data in bacterial pathogen research. The field has established standardized metrics and thresholds that differentiate high-quality genomes from those requiring additional refinement or exclusion from certain analyses.
Completeness and Contamination Assessments represent foundational quality metrics, particularly crucial for genomes derived from metagenomic assemblies or draft sequences. The Minimum Information about a Metagenome-Assembled Genome (MIMAG) standard defines high-quality MAGs as those exceeding 90% completeness while maintaining less than 5% contamination [31]. These metrics are typically assessed using conserved single-copy gene sets specific to taxonomic groups. For example, in the MAGdb repository, HMAGs (high-quality MAGs) exhibit a mean completeness of 96.84% (±2.81%) and a mean contamination rate of 1.02% (±1.09%), with genome sizes ranging from 0.52 to 12.26 Mb [31]. The relationship between sequencing depth and quality outcomes demonstrates that increased read counts generally improve both completeness and the number of recovered MAGs, though this relationship varies across sample types, with human gut and animal-derived samples showing different patterns than environmental samples [31].
Assembly Quality Metrics provide additional dimensions for evaluating genome curation outcomes. The N50 statistic, which represents the contig length at which 50% of the total assembly length is contained in contigs of equal or greater size, helps researchers assess assembly continuity. While no universal threshold exists, values exceeding 50,000 bp are often considered favorable for bacterial genomes [9]. Additionally, the presence of expected genomic features—such as complete rRNA operons, tRNAs, and conserved genomic synteny—provides biological validation of assembly quality. In comparative studies of bacterial pathogens, implementing stringent quality control procedures including CheckM evaluation with completeness ≥95% and contamination <5%, followed by genomic distance clustering (Mash distance ≤0.01), ensures a non-redundant, high-quality genome collection [9].
Table 2: Quality Control Standards for Bacterial Genome Curation
| Quality Dimension | Metric | High-Quality Standard | Assessment Tool |
|---|---|---|---|
| Completeness | Single-copy conserved genes | >90% (MIMAG standard) | CheckM, BUSCO |
| Contamination | Marker gene multiplicity | <5% (MIMAG standard) | CheckM |
| Assembly continuity | N50 statistic | ≥50,000 bp | Assembly metrics |
| Sequence quality | Q score | ≥Q30 | FastQC |
| Taxonomic validation | Taxonomic classification | Consistent with expected lineage | Kraken, GTDB-Tk |
| Gene space completeness | Universal single-copy orthologs | >95% | BUSCO |
Experimental Protocols for Genome Curation
Genome Assembly and Quality Control Protocol
DNA Extraction and Sequencing: Begin with high-molecular-weight DNA extraction using the CTAB method or commercial kits suitable for long-read sequencing. Assess DNA quality and integrity using a Qubit Fluorometer and NanoDrop Spectrophotometer, ensuring A260/A280 ratios of 1.8-2.0 [7]. Prepare sequencing libraries using the TruSeq DNA Sample Preparation Kit for Illumina platforms or the Template Prep Kit for Pacific Biosciences systems. Perform sequencing on both Illumina NovaSeq (2×150-bp paired-end reads) and Pacific Biosciences platforms to generate hybrid data for optimal assembly [7].
Data Preprocessing and Assembly: Remove adapter contamination and filter low-quality reads using AdapterRemoval and SOAPec (k-mer sizes of 17) [7]. Assemble filtered reads using multiple approaches: SPAdes and A5-miseq for Illumina data, and Flye and Unicycler with default settings for PacBio data [7]. Integrate all assembled results to generate a complete sequence, then rectify the genome assembly using Pilon software to correct base errors and fill gaps [7].
Quality Assessment: Evaluate assembly quality using CheckM with thresholds of ≥95% completeness and <5% contamination for inclusion in downstream analyses [9]. Calculate genomic distances using Mash and perform clustering through Markov clustering, removing bacterial genomes with genomic distances ≤0.01 to ensure non-redundancy [9]. Validate taxonomic classification by comparing assigned taxonomy with phylogenetic placement based on universal single-copy genes.
Genome Curation Workflow
Genome Annotation and Functional Analysis Protocol
Structural Annotation: Predict open reading frames (ORFs) using Prokka v1.14.6 or GeneMarkS v4.32 [9] [7]. Identify tRNA genes with tRNAscan-SE and rRNA genes using Barrnap [7]. Detect non-coding RNAs by comparison with the Rfam database, and identify CRISPR arrays using CRISPR finder [7].
Functional Annotation: Perform hierarchical annotation using multiple databases. Conduct BLAST searches against the Nonredundant Protein Database and Swiss-Prot with an e-value threshold of 1e-5 [7]. Map ORFs to the Cluster of Orthologous Groups (COG) database using RPS-BLAST with an e-value threshold of 0.01 and minimum coverage of 70% [9]. Annotate carbohydrate-active enzymes using dbCAN2 to map ORFs to the CAZy database, filtering with hmm_eval 1e-5 and retaining only HMMER annotations [9].
Pathogenicity Assessment: Identify virulence factors using the Virulence Factor Database (VFDB) and antimicrobial resistance genes via the Comprehensive Antibiotic Resistance Database (CARD) [9]. Annotate pathogenicity islands using IslandViewer 4 and prophages with PhiSpy [7]. For comparative genomic analyses, employ pan-genome analysis approaches using tools such as Roary, and identify orthologous groups for phylogenetic reconstruction [5].
Integration and Curation: Manually review automated annotations for key pathogenicity factors, confirming functional predictions through domain architecture analysis and literature review. Submit curated genomes to public repositories following domain-specific standards, ensuring complete metadata annotation including isolation source, host information, and antimicrobial resistance profiles.
Computational Tools and Databases: The field of bacterial genome curation relies on a sophisticated ecosystem of computational resources for annotation, analysis, and data retrieval. The National Center for Biotechnology Information (NCBI) provides an extensive suite of databases including GenBank, RefSeq, and ClinVar, which collectively offer curated genomic information and standardized annotation [28] [29]. Specialized functional databases like the Cluster of Orthologous Groups (COG) and the Carbohydrate-Active Enzymes Database (CAZy) enable prediction of gene function and metabolic capabilities [9]. For quality assessment, tools such as CheckM and BUSCO provide essential metrics for evaluating assembly completeness and contamination, while GTDB-Tk offers standardized taxonomic classification [31].
Laboratory and Bioinformatics Reagents: Wet laboratory components of genome curation depend on high-quality molecular biology reagents and sequencing platforms. DNA extraction typically employs the CTAB method or commercial kits specifically validated for microbial genomics [7]. Library preparation utilizes standardized kits such as the TruSeq DNA Sample Preparation Kit for Illumina platforms or the Template Prep Kit for Pacific Biosciences systems [7]. For functional validation of curated genomic information, cell culture reagents including Dulbecco's Modified Eagle Medium (DMEM) supplemented with fetal bovine serum (FBS) enable cell adhesion and invasion assays using models like Caco-2 and RAW264.7 cells [7].
Table 3: Essential Research Reagents and Resources for Genome Curation
| Category | Resource/Reagent | Specific Application | Key Features |
|---|---|---|---|
| Sequencing Platforms | Illumina NovaSeq | Short-read sequencing | 2×150-bp paired-end reads [7] |
| Pacific Biosciences | Long-read sequencing | Improved assembly continuity [7] | |
| DNA Extraction | CTAB method | High-molecular-weight DNA | Suitable for long-read sequencing [7] |
| Library Preparation | TruSeq DNA Kit | Illumina sequencing | Compatible with NovaSeq platform [7] |
| Template Prep Kit | PacBio sequencing | Optimized for SMRT sequencing [7] | |
| Functional Annotation | COG database | Functional categorization | RPS-BLAST with e-value 0.01 [9] |
| CAZy database | Carbohydrate-active enzymes | HMMER with hmm_eval 1e-5 [9] | |
| Quality Control | CheckM | Completeness/contamination | ≥95% completeness, <5% contamination [9] |
| Mash | Genomic distance calculation | Distance ≤0.01 for non-redundancy [9] |
High-quality genome curation provides the essential foundation for robust comparative analyses of bacterial pathogens, enabling discoveries in virulence mechanisms, host adaptation, and antimicrobial resistance. The standards, databases, and protocols outlined in this application note represent current best practices in the field, emphasizing rigorous quality control, comprehensive functional annotation, and adherence to international data standards. As genomic technologies continue to evolve, maintaining these curation standards will be crucial for ensuring data interoperability and biological accuracy. The integration of automated pipelines with expert manual curation remains the gold standard for producing reference-quality genomes that drive meaningful research outcomes in bacterial pathogenesis and therapeutic development.
Bioinformatic Pipelines for Virulence and Resistance Gene Annotation (VFDB, CARD)
In the field of bacterial comparative genomics, the identification of virulence factors (VFs) and antimicrobial resistance (AMR) genes is fundamental to understanding pathogenicity and developing treatment strategies. Two cornerstone resources for these analyses are the Virulence Factor Database (VFDB) and the Comprehensive Antibiotic Resistance Database (CARD). These databases, along with their associated analytical tools, provide researchers with curated knowledge and computational methods to annotate and interpret key genomic elements in bacterial pathogens.
The Comprehensive Antibiotic Resistance Database (CARD) is a rigorously curated bioinformatic database containing resistance genes, their products, and associated phenotypes, organized using the Antibiotic Resistance Ontology (ARO) [32]. As of its latest version, CARD contains 8,582 Ontology Terms, 6,442 Reference Sequences, 4,480 SNPs, and 6,480 AMR Detection Models [32]. The database also includes the Resistance Gene Identifier (RGI) software, which can predict resistomes from protein or nucleotide data based on homology and SNP models [33]. Analyses can be performed via a web portal with a 20 Mb limit, or via command-line tools for larger datasets.
The Virulence Factor Database (VFDB) has recently been expanded to VFDB 2.0, which consists of 62,332 nonredundant orthologues and alleles of VFGs identified using species-specific average nucleotide identity from 18,521 complete bacterial genomes [34]. This expansion has enabled the development of the MetaVF toolkit, which facilitates precise identification of pathobiont-carried VFGs at the species level from metagenomic data [34]. The VFDB has also recently integrated data on 902 anti-virulence compounds across 17 superclasses, bridging the knowledge between virulence factors and potential therapeutic interventions [35].
Table 1: Core Database Statistics and Features
| Database | Version | Core Content | Key Features | Associated Tools |
|---|---|---|---|---|
| CARD | Latest | 6,442 Reference Sequences; 4,480 SNPs; 6,480 AMR Detection Models | Antibiotic Resistance Ontology (ARO); Strict curation criteria | RGI (web & command line); CARD:BLAST |
| VFDB | 2.0 (2024) | 62,332 VFG sequences; 135 bacterial species; 3,527 VFG types | Anti-virulence compound data; Pathogen-VF associations | MetaVF toolkit; PathoFact compatibility |
| VFDB Anti-Virulence | 2024 | 902 compounds; 17 superclasses | Compound-target pathogen associations; Clinical development stages | Integrated compound browsing |
Protocol: Comprehensive Genome Annotation for Virulence and Resistance Profiling
Sample Preparation and Data Quality Control
Begin with high-quality genomic DNA extracted from bacterial isolates or metagenomic samples. For whole-genome sequencing, use platforms such as Illumina, PacBio, or Oxford Nanopore, ensuring sufficient coverage (typically >30x for isolates). For assembled genomes, assess quality using metrics from tools like QUAST—prefer contig N50 >20,000 bp for optimal ORF prediction in subsequent steps [33].
For the example protocol below, we assume the use of Klebsiella pneumoniae isolates, a genomically diverse pathogen of significant clinical relevance [36]. Filter genomes with excessive fragmentation (>250 contigs) or abnormal length (outside 4.9-6.4 Mbp for K. pneumoniae) to avoid low-quality data and contamination [36].
Annotation of Antimicrobial Resistance Genes with RGI
Principle: The Resistance Gene Identifier (RGI) predicts AMR genes based on homology to curated reference sequences and SNP models in CARD.
Procedure:
- Input Preparation: Prepare your input data as an assembled genome in FASTA format (contigs) or a protein sequence file.
- Tool Selection: Access RGI through the CARD web portal for small datasets (<20 Mb) or install the command-line version for larger analyses [33].
- Parameter Configuration:
- For complete genomes, plasmids, or high-quality assemblies (contigs >20,000 bp), select the "complete genomes" option to exclude partial gene predictions.
- For low-quality assemblies, metagenomic merged reads, or small contigs/plasmids (<20,000 bp), select the "low quality/coverage" option to include prediction of partial genes [33].
- Use Strict significance criteria, which are based on CARD-curated bitscore cut-offs, to minimize false positives.
- Execution: Run the analysis. For nucleotide sequences, RGI will automatically perform ORF calling using Prodigal before conducting homolog detection with DIAMOND [33].
- Output Interpretation: The output will list identified AMR genes, their predicted functions, and the type of match (Perfect, Strict, etc.). Use the "ARO" terms to connect genes to specific antibiotics and resistance mechanisms.
Annotation of Virulence Factors with MetaVF
Principle: The MetaVF toolkit accurately identifies virulence factor genes (VFGs) from metagenomic data or assembled genomes by aligning sequences to the expanded VFDB 2.0 and filtering with a tested sequence identity (TSI) threshold.
Procedure:
- Input Preparation: Provide clean metagenomic reads, assembled contigs, or metagenome-assembled genomes (MAGs) in FASTA format.
- Alignment: Map reads or perform nucleotide BLAST against the VFDB 2.0 alignment dataset [34].
- Filtering: Filter the mapped reads using the 90% Tested Sequence Identity (TSI) threshold. This threshold was determined to achieve a True Discovery Rate (TDR) >97% and a very low False Discovery Rate (FDR) of <4.000767e-05% based on benchmarking with artificial datasets [34].
- Annotation and Normalization: Annotate the filtered hits using the VFDB 2.0 annotation dataset, which includes information on bacterial host taxonomy, mobility, and VF categories. Normalize abundance using transcripts per million (TPM) by accounting for gene length and sequencing depth [34].
- Output Analysis: The final report includes VFG diversity, abundance, coverage, and predictions about their mobility (e.g., plasmid-borne). This helps identify pathobiont strains carrying key virulence factors.
Workflow Visualization
The following diagram illustrates the integrated protocol for simultaneous analysis of AMR genes and virulence factors:
Performance Comparison of Annotation Tools
Benchmarking Results and Interpretation
A comparative assessment of annotation tools reveals significant differences in their performance for predicting AMR phenotypes. When building "minimal models" using only known resistance markers to predict binary resistance phenotypes in Klebsiella pneumoniae, the choice of annotation tool and database substantially impacts predictive accuracy [36].
Table 2: Tool Performance in AMR Gene Annotation for K. pneumoniae
| Annotation Tool | Primary Database | Key Strengths | Considerations for K. pneumoniae |
|---|---|---|---|
| RGI | CARD | Rigorous curation; SNP models; Strict bitscore cut-offs | High specificity; web and command-line options [33] [36] |
| AMRFinderPlus | Custom (NCBI) | Detects genes and point mutations; comprehensive | Includes species-specific mutations [36] |
| Kleborate | Species-specific | Tailored for K. pneumoniae; concise gene matching | Less spurious hits for this species [36] |
| ResFinder/PointFinder | Custom | Includes species-specific point mutations | Specialized for AMR genotype-phenotype linking [36] |
| Abricate | Multiple (incl. CARD) | Supports multiple databases; rapid | Cannot detect point mutations; less comprehensive [36] |
| PathoFact | Integrated | Predicts VFs, toxins, and AMR; contextualizes with MGEs | High accuracy (0.921 VFs; 0.979 AMR) and specificity [37] |
| MetaVF | VFDB 2.0 | High sensitivity/precision; species-level VFG assignment | Superior performance for virulence factors [34] |
Critical Performance Insights:
- Minimal Model Performance: The performance of predictive models (e.g., Elastic Net, XGBoost) built using annotations from these tools varies significantly across different antibiotics [36]. This highlights "knowledge gaps" where known AMR mechanisms do not fully explain observed resistance, particularly in bacteria with open pangenomes like K. pneumoniae.
- Tool Selection Guidance: For clinical or surveillance studies aiming for high specificity in AMR gene detection, RGI with its strict cut-offs is recommended. For research aiming to discover novel associations or working with diverse metagenomic samples, PathoFact or MetaVF provide more comprehensive profiling, including mobility context.
Successful annotation of virulence and resistance genes requires a collection of specific databases, software tools, and computational resources.
Table 3: Essential Research Reagents and Resources
| Resource Name | Type | Primary Function | Access/Installation |
|---|---|---|---|
| CARD Database | Database | Curated AMR gene reference; ontology | https://card.mcmaster.ca/ [32] |
| VFDB 2.0 | Database | Expanded virulence factor gene reference | https://github.com/Wanting-Dong/MetaVF_toolkit [34] |
| RGI Software | Analysis Tool | Predicts AMR genes from sequence data | Web interface or command-line from CARD [33] |
| MetaVF Toolkit | Analysis Tool | Profiles VFGs from metagenomes | Download from GitHub repository [34] |
| PathoFact | Analysis Tool | Predicts VFs, toxins, and AMR genes; contextualizes with MGEs | https://pathofact.lcsb.uni.lu [37] |
| Prodigal | Software | ORF prediction from nucleotide sequences | Bundled with RGI; available separately [33] [37] |
| Kleborate | Analysis Tool | Species-specific typing and AMR/VF annotation for Klebsiella | https://github.com/katholt/Kleborate [36] |
Advanced Analysis: Integrating Annotations for Predictive Modeling
From Annotations to Predictive Models
The binary presence/absence matrix of annotated AMR genes ((X_{p×n} ∈ {0,1}), where (p) is samples and (n) is unique AMR features) serves as the input for machine learning models predicting resistance phenotypes [36]. This "minimal model" approach efficiently identifies antibiotics where known mechanisms sufficiently explain resistance versus those requiring discovery of novel mechanisms.
Sample Protocol: Building a Minimal Model for K. pneumoniae
- Feature Matrix Construction: Use a tool like RGI or AMRFinderPlus to annotate a collection of K. pneumoniae genomes with known resistance phenotypes. Format the results into a binary matrix where 1 indicates the presence of an AMR gene/variant and 0 indicates its absence.
- Model Training: Employ machine learning algorithms such as Elastic Net (logistic regression with L1/L2 regularization) or XGBoost to build classifiers. These models are chosen for their interpretability and ability to handle correlated features [36].
- Performance Evaluation: Assess model performance using metrics like AUC-ROC. Poor performance for a specific antibiotic indicates that the known genetic markers used as features are insufficient to predict the phenotype, highlighting a knowledge gap [36].
- Interpretation: Analyze feature importance scores from the model to identify which specific AMR genes (e.g., variants of blaCTX-M, blaKPC) are the strongest drivers of resistance predictions for different drug classes.
Integrative Analysis Workflow
The following diagram outlines the advanced workflow for integrating annotations into predictive models and comparative genomic insights:
Machine Learning and Phylogenetics in Identifying Niche-Specific Signatures
In the field of comparative genomic analysis of bacterial pathogens, understanding the genetic determinants that enable specific lifestyles—such as host preference, environmental resilience, and pathogenic potential—is paramount. The convergence of machine learning (ML) with phylogenetic methods has created a powerful paradigm for deciphering these niche-specific signatures from genomic data. This approach moves beyond traditional phylogenetic analysis, which can lack resolution for highly similar pathogens, by leveraging computational models to identify complex, multi-gene patterns associated with ecological specialization [38]. For researchers and drug development professionals, these signatures provide a rational basis for developing narrow-spectrum antimicrobials that target specific pathogens while minimizing disruption to beneficial microbiota and slowing the emergence of resistance [39]. This protocol details the application of integrated ML-phylogenetic frameworks to identify and validate niche-specific genetic signatures in bacterial pathogens.
Key Concepts and Terminology
- Niche-Specific Signature: A distinctive pattern in genomic, protein, or metabolic data that is consistently associated with a particular ecological habitat or physiological location (e.g., host stomach, aquatic environment) [40] [39].
- Pangenome: The entire set of genes found across all strains of a species or a group of species, comprising the "core" genome (shared by all) and the "accessory" genome (present in a subset) [38].
- Pan-GWAS (Pangenome-Wide Association Study): A method that correlates the presence or absence of accessory genes from a pangenome with specific phenotypic traits, such as zoonotic potential or niche preference [38].
- Mutational Spectrum: The characteristic pattern of single base substitutions accumulated in a genome, which can be influenced by niche-specific mutagens or DNA repair defects [40].
- Phylogenetic Framework: An evolutionary tree that represents the evolutionary relationships among taxa, used to correct for shared ancestry when identifying signatures and to understand trait evolution [41] [42].
Experimental Protocols
Protocol 1: Predicting Continuous Phenotypes from Genomic Composition
This protocol is adapted from studies predicting bacterial optimal growth temperature (OGT) from protein domain frequencies and can be adapted for other continuous niche-related traits [41].
1. Objective: To train a machine learning model that predicts a continuous niche-specific phenotype (e.g., optimal growth temperature) from genomic compositional data.
2. Materials and Data Requirements:
- Genome Sequences: A set of bacterial genomes with known and varied values for the target phenotype.
- Phenotype Data: Experimentally determined values for the target trait (e.g., OGT from the TEMPURA database) [41].
- Feature Annotation Pipeline: Software for annotating genomic features (e.g.,
pfam_scan.plfor protein domains against the Pfam database) [41]. - Machine Learning Environment: A computing environment with ML libraries (e.g., R
randomForest, Pythonscikit-learn).
3. Step-by-Step Workflow:
Step 1: Data Curation and Feature Extraction
- Obtain genome sequences and matched phenotype data for a diverse set of bacterial strains.
- Annotate each genome for the chosen genomic features (e.g., protein domains, k-mers, gene presence/absence).
- Construct a numerical feature matrix where rows represent genomes and columns represent the frequency or presence of each annotated feature.
Step 2: Model Training and Selection
- Partition the dataset into a training set (e.g., 75%) and a held-out test set (e.g., 25%).
- Train and compare multiple regression algorithms (e.g., Random Forest, Support Vector Regression, XGBoost) on the training set using 10-fold cross-validation.
- Select the best-performing model based on cross-validation metrics (e.g., R², root mean squared error).
Step 3: Model Evaluation and Interpretation
- Evaluate the final model's performance on the independent test set. Report Pearson's correlation coefficient (r), coefficient of determination (R²), and the percentage of predictions within a specific error margin (e.g., ±10°C for OGT) [41].
- Perform feature importance analysis (e.g., using Gini importance in Random Forest) to identify the top genomic features most strongly associated with the phenotype for downstream biological validation.
Protocol 2: Identifying Zoonotic Potential via Pan-GWAS and Classification ML
This protocol is based on a study that assessed the zoonotic potential of Brucella species from different host origins [38].
1. Objective: To identify gene sets associated with a binary niche-specific trait (e.g., zoonotic potential) and build a classifier to predict this trait in novel strains.
2. Materials and Data Requirements:
- Strain Collection: Whole-genome sequences for a large number of closely related bacterial strains, annotated with host origin and known zoonotic status.
- Pangenome Construction Tool: Software such as Roary or Panaroo.
- GWAS/ML Platform: Computational resources for pan-GWAS and machine learning (e.g., R for statistical testing, Python with
scikit-learnfor ML).
3. Step-by-Step Workflow:
Step 1: Pangenome Construction and Annotation
- Generate a pangenome from the input genomes, categorizing genes into core, accessory, and unique sets.
- Functionally annotate the genes using databases like COG (Clusters of Orthologous Genes).
Step 2: Pan-GWAS for Signature Discovery
- Define a binary phenotype (e.g., high vs. low zoonotic potential) based on experimental data or literature.
- Perform a pan-GWAS to test for significant associations between the presence/absence of accessory genes and the binary phenotype. Use phylogenetic correction to account for population structure.
- Extract a list of significantly associated genes as the candidate niche-specific signature.
Step 3: Machine Learning Classifier Construction
- Use the presence/absence pattern of the candidate signature genes as features for a classification ML model.
- Train and evaluate multiple classifiers (e.g., Support Vector Machine, Random Forest) to predict the phenotypic class.
- Select the best model based on accuracy, precision, and recall on a test set. The model can then be used to score the zoonotic potential of uncharacterized strains.
Table 1: Example ML Model Performance for Predicting Zoonotic Potential (adapted from [38])
| Machine Learning Algorithm | Reported Accuracy | Key Strengths |
|---|---|---|
| Support Vector Machine (SVM) | High (Selected as optimal) | Effective in high-dimensional spaces |
| Random Forest (RF) | High | Robust to overfitting, provides feature importance |
| Decision Trees (DTC) | Comparative metrics | Model interpretability |
| K-Nearest Neighbors (KNN) | Comparative metrics | Simple, instance-based learning |
| Multilayer Perceptron (MLP) | Comparative metrics | Can model non-linear relationships |
Protocol 3: Decoding Niche-Associated Mutational Spectra
This protocol leverages the concept that mutational patterns can serve as a historical record of a bacterium's environmental exposures and internal repair mechanisms [40].
1. Objective: To reconstruct and deconvolute mutational spectra from bacterial genome alignments to infer past niche occupancy.
2. Materials and Data Requirements:
- Genomic Alignments: High-quality whole-genome sequence alignments for multiple strains within a phylogenetic clade.
- Phylogenetic Trees: A rooted phylogenetic tree for the strains under study.
- Bioinformatic Tool: Specialized software like MutTui for reconstructing mutational spectra [40].
3. Step-by-Step Workflow:
Step 1: Mutational Spectrum Reconstruction
- Input a genome alignment and corresponding phylogenetic tree into MutTui.
- The software reconstructs the historical substitutions that occurred on each branch of the tree, generating a single base substitution (SBS) mutational spectrum for each clade.
Step 2: Signature Extraction and Decomposition
- Use non-negative matrix factorization (NMF) to decompose the collection of SBS spectra from multiple clades into a set of fundamental "mutational signatures."
- Correlate these extracted signatures with known defects in DNA repair (e.g., from hypermutator lineages) or known mutagenic processes.
Step 3: Niche Association and Inference
- Statistically compare the activities of different mutational signatures between clades known to replicate in different niches (e.g., gut vs. soil).
- Identify signatures that are significantly enriched in a specific niche. These niche-associated mutational signatures can then be used to infer the primary replication niche for bacterial clades of unknown ecology.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools and Databases for Identifying Niche-Specific Signatures
| Tool/Resource Name | Type | Primary Function in Analysis | Example Use Case |
|---|---|---|---|
| Pfam Database [41] | Protein Family Database | Provides hidden Markov models (HMMs) for annotating protein domains in genomic sequences. | Used as input features for predicting Optimal Growth Temperature. |
| Roary [38] | Pangenome Construction Tool | Rapidly constructs the pangenome from annotated genome sequences. | Generating the gene presence/absence matrix for Pan-GWAS in Brucella. |
| MutTui [40] | Bioinformatics Tool | Reconstructs mutational spectra from genome alignments and phylogenetic trees. | Identifying niche-associated mutational signatures in diverse bacterial pathogens. |
| Reconstructor [39] | Genome-Scale Model Tool | Automates the generation of genome-scale metabolic network reconstructions (GENREs). | Building the PATHGENN collection to identify niche-specific metabolic phenotypes. |
| Random Forest [41] | Machine Learning Algorithm | A versatile ensemble learning method used for both regression and classification tasks. | Achieving high predictive accuracy (R² = 0.853) for bacterial optimal growth temperature. |
| Support Vector Machine (SVM) [38] | Machine Learning Algorithm | A powerful classifier effective in high-dimensional spaces, useful for binary classification. | Building the final model to predict the zoonotic potential of Brucella strains with high accuracy. |
| Non-Negative Matrix Factorization (NMF) [40] | Computational Method | Decomposes a complex dataset into recognizable, additive component signatures. | Deconvoluting composite mutational spectra into individual, biologically relevant signatures. |
Data Presentation and Analysis
The following table summarizes quantitative results from key studies that successfully applied these protocols to identify niche-specific signatures.
Table 3: Summary of Representative Studies Applying ML and Phylogenetics for Niche Signature Identification
| Study Focus | Key Genomic Feature Used | ML Model Employed | Performance Outcome | Identified Niche-Associated Signatures |
|---|---|---|---|---|
| Bacterial Optimal Growth Temperature (OGT) [41] | Protein domain frequencies | Random Forest (Regression) | R² = 0.853 on test set; 82.4% of predictions within ±10°C error. | Positive OGT correlation: Domains related to polyamine metabolism, tRNA methyltransferases, CRISPR-Cas. Negative OGT correlation: Domains involved in redox homeostasis, transport. |
| Zoonotic Potential of Brucella [38] | Accessory genes from pangenome | Support Vector Machine (SVM) | High prediction accuracy for zoonotic potential across strains. | 268 genes associated with zoonotic potential; host origin (e.g., domestic pig vs. wild boar) was a key determinant. |
| Niche-Specific Metabolic Targets [39] | Genome-scale metabolic models (GENREs) | Flux Balance Analysis (FBA) | Identification of uniquely essential genes; validation via growth inhibition assays. | Stomach pathogens: Unique essentiality of gene thyX (encodes an alternative thymidylate synthase). |
| Niche-Associated Mutational Spectra [40] | Single Base Substitution (SBS) patterns | Non-negative Matrix Factorization (NMF) | Extraction of 24 distinct bacterial mutational signatures (Bacteria_SBS1-24). | Signatures specific to the gastrointestinal niche, and others associated with defects in DNA repair genes (e.g., mutY, mutT, ung). |
The escalating crisis of antimicrobial resistance (AMR) among bacterial pathogens has necessitated the exploration of alternatives to conventional antibiotics. Antimicrobial peptides (AMPs) represent a promising class of molecules, serving as a first-line defense within the innate immune systems of most organisms [43] [44]. These peptides are typically short, cationic, and amphiphilic, enabling them to interact with and disrupt microbial membranes, a mechanism that reduces the likelihood of resistance development compared to traditional antibiotics [43] [45]. The field of comparative genomic analysis provides a powerful framework for discovering novel AMPs and understanding their role in host-pathogen interactions. By analyzing the genetic repertoires of bacterial pathogens, researchers can identify conserved core genomes essential for basic survival and accessory genes that confer niche-specific adaptations, including resistance and virulence factors [5] [9] [6]. This application note details how comparative genomics can be systematically leveraged to discover and characterize novel AMPs with therapeutic potential.
Table 1: Key Characteristics of Antimicrobial Peptides
| Feature | Description | Significance |
|---|---|---|
| Length | Typically 10-60 amino acid residues [44] | Small size facilitates synthesis and modification. |
| Net Charge | Often cationic (positively charged) [43] | Promotes electrostatic interaction with negatively charged microbial membranes. |
| Structure | Frequently form amphiphilic α-helices or β-sheets [43] | Enables insertion and disruption of lipid bilayers. |
| Mechanism of Action | Membrane permeabilization, membrane depolarization, intracellular targets [45] | Leads to rapid bactericidal activity and low propensity for resistance. |
| Spectrum of Activity | Broad-spectrum activity against bacteria, fungi, viruses, and parasites [44] | Potential as multi-target antimicrobial agents. |
Computational Workflow for AMP Discovery
The integration of comparative genomics and artificial intelligence has created a high-throughput pipeline for mining and generating novel AMP candidates. This workflow begins with the identification of potential AMP-encoding genes within genomic datasets and can be extended to the de novo design of optimized peptides.
Pan-Genome Analysis for AMP Gene Identification
The first step involves constructing a bacterial pan-genome—the entire set of genes from all strains of a species—to understand the genetic diversity and identify potential AMPs within the dispensable genome that may contribute to niche adaptation [46]. This is achieved through:
- Genome Collection & Curation: Assembling high-quality, non-redundant genome sequences of the target bacterial pathogens from databases, annotated with ecological niche information (e.g., human, animal, environment) [9].
- Pan-Genome Construction: Using computational tools to partition the gene repertoire into the core genome (genes shared by all strains) and the accessory genome (genes present in a subset of strains) [5] [46].
- Identification of AMP Precursors: Screening the accessory genome for sequences encoding small, cationic peptides that are potential AMP precursors.
AI-Driven Mining and Generation of AMPs
Recent advances have employed large language models (LLMs) specifically trained on protein sequences to revolutionize AMP discovery [45]. A sequential pipeline can be assembled using specialized sub-models:
- AMPSorter: A classifier fine-tuned to distinguish AMPs from non-AMPs with high accuracy (AUC=0.99) [45].
- BioToxiPept: A classifier designed to identify peptide cytotoxicity, reducing the risk of hemolytic activity in candidates [45].
- AMPGenix: A generative model that creates novel, functional AMP sequences de novo based on learned principles from known AMPs [45].
The following diagram illustrates this integrated computational workflow:
Experimental Validation of AMP Activity
Candidate AMPs identified through computational pipelines must undergo rigorous in vitro and in vivo validation to confirm their efficacy and safety.
In Vitro Antimicrobial Susceptibility Testing
Objective: To determine the minimum inhibitory concentration (MIC) of novel AMPs against a panel of multidrug-resistant bacterial pathogens. Protocol:
- Bacterial Strains: Utilize reference strains and clinically isolated multidrug-resistant (MDR) pathogens, such as carbapenem-resistant Acinetobacter baumannii (CRAB) and methicillin-resistant Staphylococcus aureus (MRSA) [45].
- Peptide Preparation: Reconstitute synthetic AMPs in sterile, apyrogenic water or diluted buffer. Prepare twofold serial dilutions in an appropriate broth (e.g., Mueller-Hinton Broth).
- Broth Microdilution Assay: Inoculate each well of a 96-well plate containing the peptide dilutions with a standardized bacterial suspension (~5 × 10^5 CFU/mL). Include growth control and sterility control wells.
- Incubation and MIC Determination: Incubate the plate at 37°C for 16-20 hours. The MIC is defined as the lowest peptide concentration that completely inhibits visible growth [45] [44].
Cytotoxicity and Hemolysis Assays
Objective: To evaluate the safety profile of AMPs by assessing their toxicity to mammalian cells. Protocol:
- Cell Lines: Culture mammalian cell lines (e.g., HEK-293 or HaCaT) and isolate human red blood cells (hRBCs) from fresh, heparinized blood.
- Treatment: Incubate cells with a range of AMP concentrations (e.g., 1-200 µg/mL) for several hours. Use PBS and 1% Triton X-100 as negative and positive controls for hRBCs, respectively.
- Viability Measurement:
- For adherent cells: Use MTT or AlamarBlue assays to measure metabolic activity.
- For hRBCs: Centrifuge the samples after incubation and measure the hemoglobin release in the supernatant by absorbance at 540 nm.
- Calculation: Calculate the percentage of hemolysis relative to the positive control. The therapeutic index is often reported as the ratio of the cytotoxic concentration (e.g., HC50) to the average MIC [45] [47].
Mechanism of Action Studies
Objective: To confirm that the AMP's primary mechanism involves membrane disruption. Protocol:
- Membrane Depolarization: Use a fluorescent dye, such as DiSC3(5), which is incorporated into the membranes of energized bacteria. Add the AMP and monitor the increase in fluorescence as the membrane potential is dissipated [45].
- Cytoplasmic Membrane Permeabilization: Employ dyes like SYTOX Green or propidium iodide, which are nucleic acid stains that cannot cross intact membranes. Add the dye and the AMP to a bacterial suspension, and measure the fluorescence increase as the dye enters cells with compromised membranes [43] [45].
- Visualization by Microscopy: Use scanning or transmission electron microscopy (SEM/TEM) to visualize the morphological changes in bacterial cells, such as pore formation, membrane blebbing, or cell lysis, following AMP treatment [43].
Table 2: Key Reagent Solutions for AMP Validation
| Research Reagent | Function / Application | Brief Explanation |
|---|---|---|
| Cation-adjusted Mueller-Hinton Broth (CAMHB) | In vitro susceptibility testing | Standardized growth medium for determining Minimum Inhibitory Concentration (MIC). |
| SYTOX Green / Propidium Iodide | Mechanism of action studies | Fluorescent dyes that stain nucleic acids only in cells with permeabilized membranes, indicating membrane disruption. |
| DiSC3(5) dye | Mechanism of action studies | A potentiometric dye used to measure membrane depolarization in real-time. |
| hRBCs (Human Red Blood Cells) | Hemolysis assay | Primary cells used to evaluate the hemolytic activity and selectivity of AMPs for bacterial vs. mammalian membranes. |
| MTT / AlamarBlue reagents | Cytotoxicity assay | Cell viability indicators that measure metabolic activity in mammalian cells after AMP exposure. |
In Vivo Efficacy and Resistance Development Assessment
Promising AMP candidates must be evaluated in biologically complex models to assess their therapeutic potential and propensity for resistance development.
In Vivo Efficacy in Animal Models
Objective: To evaluate the therapeutic efficacy of AMPs in a live infection model. Protocol (Mouse Thigh Infection Model):
- Infection Establishment: Render mice neutropenic via cyclophosphamide administration. Subsequently, inoculate the thigh muscle of each mouse with a standardized inoculum (e.g., ~10^6 CFU) of a target MDR pathogen like MRSA or CRAB [45].
- Treatment: Initiate therapy (e.g., 2 hours post-infection). Administer the AMP candidate via a relevant route (e.g., intraperitoneal or intravenous injection). Include control groups treated with a vehicle or a conventional antibiotic.
- Assessment: At a predetermined endpoint (e.g., 24 hours), euthanize the animals, harvest the infected thighs, and homogenize the tissue. Plate serial dilutions of the homogenate to quantify bacterial burden (CFU/thigh) [45].
Assessing Susceptibility to Resistance Development
Objective: To determine if bacteria develop resistance to novel AMPs less readily than to conventional antibiotics. Protocol (Serial Passage Assay):
- Initial Passage: Expose a bacterial culture to a sub-inhibitory concentration of the AMP (e.g., 0.5 x MIC) for 24 hours.
- Serial Passage: Inoculate fresh medium containing the same peptide concentration with bacteria from the previous passage. Repeat this process for multiple cycles (e.g., >20 passages).
- MIC Monitoring: Periodically (e.g., every 3-4 passages), determine the MIC of the AMP against the serially passaged population. A significant increase in MIC indicates the development of resistance [45].
- Control: Conduct a parallel experiment with a conventional antibiotic for comparison. Studies have shown that AMPs generated by AI models exhibit reduced susceptibility to resistance development in CRAB and MRSA compared to clinical antibiotics [45].
The following diagram summarizes the key stages of experimental validation:
The strategic integration of comparative genomics and generative artificial intelligence provides a powerful, rational framework for accelerating the discovery of novel Antimicrobial Peptides. This approach enables researchers to move beyond traditional screening methods to a targeted and predictive process of identifying and designing AMPs with potent activity against multidrug-resistant pathogens and a low propensity for resistance development. The structured application notes and protocols outlined herein—from pan-genome mining and AI-driven generation to rigorous in vitro and in vivo validation—offer a comprehensive roadmap for researchers and drug development professionals. This integrated methodology holds significant promise for expanding the therapeutic arsenal against the growing threat of antimicrobial resistance.
Precision medicine has revolutionized clinical trial design by moving away from traditional "one-size-fits-all" approaches toward patient-centered strategies that account for individual variability, particularly genetic differences [48]. This shift is particularly relevant in infectious disease research, where bacterial pathogens exhibit significant genomic heterogeneity that impacts treatment response. Master protocol frameworks—including basket and umbrella trials—provide efficient methodologies for evaluating multiple targeted therapies within a single overarching trial structure [49]. These innovative designs enable researchers to match specific therapies to bacterial genotypes, potentially accelerating the development of more effective treatments for resistant infections.
The completion of the Human Genome Project and advancements in next-generation sequencing technologies have fueled the development of precision medicine, allowing for the identification of genetic phenotypes that can be targeted by specific therapies [48]. While these trial designs originated and have been primarily applied in oncology, their principles are highly applicable to infectious diseases, where genetic markers of antibiotic resistance or virulence could similarly guide treatment selection [50] [49]. This application note explores the adaptation of basket and umbrella trial designs to the context of bacterial pathogen research and genotype-specific therapy development.
Basket Trial Design: Principles and Applications
Conceptual Framework and Definition
Basket trials are prospective clinical studies designed with the hypothesis that the presence of selected molecular features determines a patient's response to one or more targeted treatment strategies [51]. In the context of bacterial pathogens, this approach can be applied to target-specific therapies across multiple bacterial species that share common resistance mechanisms or virulence factors.
The core principle of basket trial design is that a patient's expectation of treatment benefit can be ascertained from accurate characterization of the pathogen's molecular profile, and that biomarker-guided treatment selection supersedes traditional clinical classification [51]. These trials are typically conducted within phase II settings, allowing drug developers to effectively evaluate and identify preliminary efficacy signals among clinical indications identified as promising in pre-clinical studies [51] [52].
Statistical Considerations and Design Variations
Basket trial analyses occur across a spectrum spanning independence to full statistical "exchangeability" [51]. At one extreme, trialists can ignore the possibility of heterogeneous benefit among patients exhibiting a common treatment target, enabling pooled analyses. At the opposite extreme, studies can evaluate treatment effectiveness for each subpopulation independently of evidence acquired from other patient subsets.
Innovative statistical methods have been developed to address the challenge of heterogeneity in treatment response across different baskets. These include:
- Bayesian hierarchical modeling: Allows for information borrowing across related subpopulations
- Multi-stage designs: Merge subtypes at interim analyses based on accumulating evidence
- Model averaging methods: Facilitate Bayesian inference with respect to all possible pairwise exchangeability relationships among studied subpopulations [51]
More recently, basket trial methodologies have been extended to include randomized, confirmatory designs and enrichment designs within platform trials, providing pathways for accelerated approval [51].
Table 1: Key Characteristics of Basket Trials in Precision Medicine
| Characteristic | Description | Application in Bacterial Pathogen Research |
|---|---|---|
| Primary Objective | Evaluate one targeted therapy across multiple diseases/pathogens sharing a common biomarker [49] [53] | Test antibiotic/antivirulence strategy across bacterial species with common resistance mechanism |
| Patient Population | Multiple diseases or pathogen types grouped by molecular alteration [48] [49] | Patients infected with different bacterial species sharing genetic resistance markers |
| Unifying Feature | Common predictive biomarker or genetic alteration [49] [53] | Shared genetic determinant of antibiotic resistance or virulence |
| Common Phase | Phase II (primarily exploratory) [51] [49] | Early clinical development for novel antimicrobial approaches |
| Typical Design | Often single-arm, non-randomized [49] | Single-arm studies comparing to historical controls |
| Sample Size | Median ~205 participants (IQR: 90-500) [49] | Adapted based on prevalence of target biomarker |
Figure 1: Basket Trial Design Framework for Bacterial Pathogens. This diagram illustrates the application of basket trial design to bacterial pathogen research, where multiple pathogen types sharing a common genetic marker (e.g., a specific antibiotic resistance gene) are treated with the same targeted therapeutic.
Umbrella Trial Design: Principles and Applications
Conceptual Framework and Definition
Umbrella trials represent a master protocol approach that evaluates multiple targeted therapies for a single disease condition, which is stratified into subgroups based on different molecular characteristics [48] [50]. In bacterial pathogen research, this design could be applied to a specific infection type (e.g., healthcare-associated pneumonia) stratified by different resistance mechanisms.
The umbrella trial framework recruits patients with a single condition and screens them to determine whether they belong to one of several pre-defined subgroups or modules [50]. These subgroups comprise different subtrials within the overarching master protocol. The design links specific subgroups with potential treatment allocations, which may include both control and experimental arms.
Design Variations and Methodological Considerations
Umbrella trials can be implemented in several variations, including:
- Non-randomized designs: Patients in each subgroup are automatically assigned to a linked experimental treatment
- Randomized designs: Patients in subgroups are assigned to either a linked experimental treatment or a linked control treatment
- Hybrid designs: Incorporate elements of both basket and platform trials [50]
The statistical complexities of umbrella trials include adaptive design elements, choice between Bayesian/frequentist decision rules, appropriate sample size calculation, information borrowing strategies, and error rate control [50]. These considerations vary depending on the specific variant of umbrella design and study-specific requirements.
Table 2: Key Characteristics of Umbrella Trials in Precision Medicine
| Characteristic | Description | Application in Bacterial Pathogen Research |
|---|---|---|
| Primary Objective | Evaluate multiple targeted therapies for a single disease stratified by biomarkers [50] [49] | Test multiple targeted therapies for a specific infection type stratified by resistance mechanisms |
| Patient Population | Single disease or infection type with molecular subtypes [48] [53] | Patients with a specific bacterial infection categorized by genetic profiles |
| Stratification Basis | Predictive biomarkers or molecular characteristics [50] [49] | Genetic determinants of antibiotic resistance, virulence factors, or strain types |
| Common Phase | Phase I/II (primarily early phase) [50] [49] | Early to mid-stage clinical development for targeted antimicrobials |
| Use of Randomization | More common than in basket trials (~44% of trials) [50] [49] | Randomized comparisons within genetic subtypes when feasible |
| Sample Size | Median ~346 participants (IQR: 252-565) [49] | Adapted based on prevalence of each genetic subtype |
Figure 2: Umbrella Trial Design Framework for Bacterial Pathogens. This diagram illustrates the application of umbrella trial design to bacterial pathogen research, where a single infection type is stratified by different genetic profiles, with each profile receiving a matched targeted therapeutic.
Comparative Analysis of Trial Designs
Methodological Comparison
Basket and umbrella trials represent complementary approaches within the master protocol framework, each with distinct advantages and limitations. Basket trials are essentially drug-centered, evaluating a single intervention across multiple diseases or pathogen types based on a common biomarker [48] [53]. In contrast, umbrella trials are disease-centered, investigating multiple interventions within a single disease or infection type stratified by different biomarkers [48] [50].
The number of master protocols has increased rapidly over the past decade, with basket trials being the most commonly implemented design [49] [52]. This growth reflects the increasing recognition of molecular heterogeneity within traditional disease classifications and the need for more efficient drug development pathways.
Practical Implementation Considerations
Table 3: Comparison of Basket and Umbrella Trial Designs
| Aspect | Basket Trial | Umbrella Trial |
|---|---|---|
| Primary Focus | One therapy for multiple diseases/pathogens with common biomarker [48] [53] | Multiple therapies for one disease/infection type with different biomarkers [48] [50] |
| Trial Phase | Primarily exploratory (Phase I/II) [49] | Primarily exploratory (Phase I/II) but more Phase III than basket trials [50] [49] |
| Randomization | Less common (~10% of trials) [49] | More common (~44% of trials) [50] [49] |
| Sample Size | Median: 205 participants [49] | Median: 346 participants [49] |
| Study Duration | Median: 22.3 months [49] | Median: 60.9 months [49] |
| Key Challenge | Heterogeneity of treatment effect across baskets [51] [52] | Statistical complexity, multiple comparisons [50] |
| Regulatory Precedent | Used for tumor-agnostic approvals [52] | Less commonly used for regulatory approval [50] |
Experimental Protocols for Genotype-Specific Therapy Trials
Pathogen Genotyping and Biomarker Identification Protocol
Objective: To identify and characterize genetic biomarkers in bacterial pathogens that predict response to targeted therapies.
Materials:
- Bacterial isolates from clinical specimens
- DNA extraction kits (e.g., QIAamp DNA Mini Kit)
- Next-generation sequencing platform (e.g., Illumina MiSeq)
- PCR reagents and thermocycler
- Bioinformatic analysis software
Procedure:
- Sample Collection and Processing: Collect clinical isolates from infected patients. Culture bacteria according to standard microbiological protocols.
- DNA Extraction: Extract genomic DNA using commercial kits following manufacturer's instructions. Quantify DNA concentration using fluorometric methods.
- Whole Genome Sequencing: Prepare sequencing libraries using compatible kit. Sequence on appropriate platform (minimum 50x coverage recommended).
- Variant Calling: Align sequencing reads to reference genome using BWA or Bowtie2. Identify genetic variants (SNPs, insertions/deletions) using GATK or similar tools.
- Resistance Gene Detection: Screen for known antibiotic resistance genes using curated databases (e.g., CARD, ResFinder).
- Biomarker Validation: Confirm putative biomarkers using targeted PCR and Sanger sequencing.
Quality Control:
- Include positive and negative controls in all experimental steps
- Verify DNA quality using gel electrophoresis or Bioanalyzer
- Replicate variant calls across different bioinformatic pipelines
Basket Trial Implementation Protocol for Multiple Bacterial Pathogens
Objective: To evaluate the efficacy of a targeted therapeutic across multiple bacterial species sharing a common genetic marker.
Trial Design:
- Phase II, open-label, single-arm basket trial
- Multiple baskets defined by bacterial species
- Common intervention across all baskets
Eligibility Criteria: Inclusion Criteria:
- Adults (≥18 years) with confirmed bacterial infection
- Bacterial isolate positive for target genetic marker
- Measurable disease by clinical or radiological criteria
- Adequate organ function
Exclusion Criteria:
- Polymicrobial infection with non-target pathogens
- Concomitant conditions precluding evaluation
- Hypersensitivity to study drug components
Treatment Protocol:
- Administer targeted therapeutic at predetermined dose
- Duration based on infection type and clinical response
- Supportive care per standard guidelines
Endpoint Assessment:
- Primary Endpoint: Clinical response at test-of-cure visit (7-14 days after treatment completion)
- Secondary Endpoints: Microbiological eradication, time to resolution of symptoms, safety and tolerability
Statistical Considerations:
- Each basket analyzed separately with potential for information borrowing
- Simon's two-stage design for futile baskets
- Bayesian hierarchical models for borrowing information across baskets
Umbrella Trial Implementation Protocol for Single Infection Type
Objective: To evaluate multiple targeted therapies for a specific bacterial infection type stratified by genetic profiles.
Trial Design:
- Phase II, randomized umbrella trial
- Multiple strata defined by genetic profiles
- Stratum-specific intervention assignments
Stratification and Randomization:
- Screen bacterial isolates for predefined genetic markers
- Assign to appropriate stratum based on genetic profile
- Randomize within each stratum to experimental therapy or control
- Use block randomization within strata to maintain balance
Treatment Protocols:
- Develop stratum-specific treatment protocols based on biomarker
- Control arm: Standard of care antibiotic therapy
- Experimental arms: Biomarker-matched targeted therapies
Endpoint Assessment:
- Primary Endpoint: Clinical response rate within each stratum
- Secondary Endpoints: Microbiological response, recurrence rate, safety
Statistical Considerations:
- Control family-wise error rate using hierarchical testing procedures
- Pre-specified rules for early stopping for futility or efficacy
- Sample size calculations based on stratum prevalence and effect size
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Genotype-Specific Therapy Trials
| Category | Specific Reagents/Materials | Function | Application Notes |
|---|---|---|---|
| Sample Processing | DNA extraction kits (e.g., QIAamp, DNeasy) | Isolation of high-quality genomic DNA from bacterial isolates | Critical step for downstream molecular analyses [54] |
| Molecular Detection | PCR reagents (primers, probes, polymerases) | Amplification and detection of specific genetic markers | Enables rapid screening for target biomarkers [54] |
| Sequencing | Next-generation sequencing kits | Comprehensive genomic characterization | Identifies known and novel genetic variants [48] |
| Bioinformatic Analysis | Analysis pipelines (GATK, BWA, Bowtie2) | Processing and interpretation of sequencing data | Essential for variant calling and annotation [55] |
| Culture Media | Selective and differential media | Bacterial isolation and phenotypic characterization | Supports correlation of genotype with phenotype |
| Reference Materials | Characterized bacterial strain collections | Quality control and assay validation | Ensures reproducibility across laboratories |
Basket and umbrella trial designs represent powerful methodological approaches for advancing genotype-specific therapies in bacterial pathogen research. These master protocols offer efficient frameworks for evaluating targeted treatments in biomarker-defined patient populations, potentially accelerating the development of precision medicine approaches for infectious diseases.
The successful implementation of these trial designs requires careful consideration of statistical approaches, particularly for addressing heterogeneity across baskets in basket trials and multiple comparisons in umbrella trials [51] [50]. Furthermore, the integration of advanced genomic technologies and bioinformatic analyses is essential for accurate biomarker identification and patient stratification [55].
As these innovative trial designs continue to evolve, their application beyond oncology to infectious diseases holds promise for addressing the growing challenge of antimicrobial resistance and improving patient outcomes through genotype-directed therapy.
Navigating Analytical Challenges: Data Quality, Contamination, and Integration
Addressing Genome Assembly and Annotation Inconsistencies
Inconsistencies in genome assembly and annotation present significant challenges in comparative genomic studies of bacterial pathogens, potentially leading to flawed biological interpretations and hindering drug development efforts. These inconsistencies arise from multiple sources, including the choice of bioinformatics tools, the quality of sequencing data, and the inherent complexity of microbial genomes [56] [57]. For bacterial pathogens, reliable genome data is crucial for understanding pathogenicity, tracking outbreaks, and identifying targets for novel antimicrobials [58]. This application note outlines standardized protocols and analytical frameworks to address these critical issues, providing researchers with methodologies to enhance the reliability and reproducibility of their genomic analyses. We integrate quantitative comparisons of tools and detailed experimental protocols to establish best practices for generating high-quality bacterial genome resources with proper data provenance.
Quantitative Assessment of Tool Performance
1Assembly and Annotation Tool Variability
The selection of computational tools significantly impacts both genome assembly continuity and annotation accuracy. Table 1 summarizes performance metrics for commonly used assemblers and annotators, highlighting key trade-offs.
Table 1: Comparative Performance of Genome Assemblers and Annotation Tools
| Tool Category | Tool Name | Key Features/Methodology | Reported Performance/Issues |
|---|---|---|---|
| Genome Assembler | SPAdes | De Bruijn graph-based; widely used for bacterial genomes [57] | Foundational algorithm; performance affected by genomic repeats [57] |
| Genome Assembler | Unicycler | SPAdes-based; hybrid assembler for short and long reads [57] | Provides lower number of contigs and higher NG50 compared to Flye; reduces misassemblies [59] [57] |
| Genome Assembler | Shovill | SPAdes-based; optimizes assembly runtimes [57] | Faster runtimes compared to standard SPAdes [57] |
| Prokaryotic Annotator | RAST | Web-based subsystem technology [59] [56] | Annotated >60,000 genomes; ~2.1% error rate, often in short CDS (<150 nt) like transposases [59] [56] |
| Prokaryotic Annotator | PROKKA | Stand-alone; rapid annotation [56] | ~0.9% error rate; faster but less comprehensive than RAST [59] |
| Prokaryotic Annotator | PGAP | NCBI's stand-alone pipeline; homology & ab initio [56] | Used for NCBI's prokaryotic genome annotation [56] |
| Specialized Annotator | AMRFinderPlus | Identifies AMR genes and mutations [36] | More comprehensive coverage compared to tools like Abricate [36] |
| Specialized Annotator | Kleborate | Species-specific for K. pneumoniae [36] | Yields more concise and less spurious gene matching [36] |
2Impacts of Database and Metadata Incompleteness
Inconsistencies extend beyond tool algorithms to encompass database completeness and metadata quality. A comparative genomics study of 1,113 authenticated bacterial genomes revealed significant issues in public repositories like NCBI's RefSeq, including problems with "assembly type" (not available for all assemblies), "sequencing technology" (missing or unknown for ~40% of assemblies), and "assembly method" (missing for ~40% of assemblies) [58]. These metadata gaps severely compromise data provenance and reproducibility [58].
For Antimicrobial Resistance (AMR) annotation, different databases (CARD, ResFinder, ARDB) exhibit varying completeness due to different curation rules and focuses [36]. This variability directly impacts phenotypic prediction; minimal machine learning models built from known AMR markers show that predictive performance is insufficient for several antibiotics, indicating critical knowledge gaps where novel resistance mechanisms remain undiscovered [36].
Standardized Protocols for Robust Genomic Analysis
1Integrated Workflow for Genome Assembly and Annotation
The following workflow integrates best practices for generating high-quality bacterial genome assemblies and annotations, crucial for reliable comparative genomics of pathogens.
Diagram 1: Integrated workflow for bacterial genome assembly and annotation. QC, quality control; ONT, Oxford Nanopore Technologies; BUSCO, Benchmarking Universal Single-Copy Orthologs; LAI, LTR Assembly Index.
2Protocol 1: Hybrid Genome Assembly for Bacterial Pathogens
Principle: Combine the high accuracy of short-read Illumina data with the long-range connectivity of Oxford Nanopore Technologies (ONT) reads to produce complete, high-fidelity bacterial genome assemblies [58].
Experimental Procedures:
- DNA Extraction: Extract High-Molecular-Weight (HMW) genomic DNA from a pure bacterial culture using a protocol that minimizes shearing (e.g., using magnetic bead-based cleanups) [58].
- Library Preparation and Sequencing:
- Illumina: Prepare a sequencing library with an insert size of 350-550 bp. Sequence on an Illumina platform (e.g., NovaSeq) to achieve a minimum coverage of 100x. This provides high base-level accuracy [58].
- Oxford Nanopore: Prepare a library using a ligation kit (e.g., LSK114). Sequence on a PromethION or MinION flow cell to achieve a minimum coverage of 60x. This provides long reads for resolving repeats and structural variants [58].
- Quality Control of Reads:
- Illumina: Use
fastp[57] to remove adapters and low-quality bases. - Nanopore: Use
NanoPlotto assess read length distribution (N50 > 20 kbp is desirable) and mean quality score. - Purity Check: Taxonomically classify reads from both platforms using
Kraken2or the One Codex platform to confirm the absence of contaminating sequences [58].
- Illumina: Use
- Hybrid De Novo Assembly: Perform assembly using
Unicycler(v0.5.0), which is specifically designed for hybrid read sets. Use default parameters, which optimally integrate short and long reads to produce a consensus assembly [59] [58] [57]. - Assembly Quality Assessment: Evaluate the resulting assembly using multiple metrics [60]:
- Contiguity: Calculate N50/NG50 and L50/LG50 statistics.
- Completeness: Run
BUSCO(v3.0.2) with thebacteria_odb10dataset. A score >95% is indicative of a high-quality assembly [61] [60]. - Repeat Space Completeness: Calculate the LTR Assembly Index (LAI) using
LTR_retriever(v2.8.2). An LAI > 20 suggests a high-quality, reference-grade assembly [61] [60]. - Base-level Accuracy: Assess quality value (QV) and k-mer completeness with
Merqury[61].
3Protocol 2: Structural and Functional Genome Annotation
Principle: Identify the coordinates and functional attributes of genomic features (genes, non-coding RNAs) using a combination of ab initio prediction and homology-based methods to maximize accuracy [56].
Experimental Procedures:
- Structural Annotation of Genes:
- Input: The final assembled genome in FASTA format from Protocol 1.
- Tool Execution: Run
PROKKA(v1.14.6) for a rapid, standardized annotation. PROKKA integrates several tools (e.g.,Prodigalfor CDS prediction,Aragornfor tRNAs,Infernalfor rRNAs) and is highly efficient for bacterial genomes [56]. - Alternative for Comprehensive Annotation: For more thorough annotation, especially for research-critical pathogens, use the NCBI's
PGAPpipeline, which combines homology-based and ab initio methods [56].
- Functional Annotation:
- Core Function: PROKKA and PGAP automatically assign putative functions by searching predicted proteins against curated databases like SwissProt and Pfam [56].
- Specialized Annotation (AMR): Identify antimicrobial resistance genes using
AMRFinderPlus(v3.10.14), which includes both resistance genes and point mutations, providing more comprehensive coverage than many other tools [36]. - Species-Specific Typing: For high-resolution strain typing, perform core genome MultiLocus Sequence Typing (cgMLST) using the
chewBBACAtool (v3.1.2) with a relevant schema from PubMLST [57].
- Annotation Curation and Validation:
- Manual Inspection: Manually review annotations for genes shorter than 150 bp, particularly transposases, mobile elements, and hypothetical proteins, as these are prone to mis-annotation [59]. Use a genome browser like Artemis for visualization.
- Transcriptomic Evidence: If available, align RNA-Seq reads to the genome using
HISAT2and visualize the alignments to validate gene models and identify potential missed genes [56].
Table 2: Key Research Reagents and Computational Tools for Genomic Analysis
| Category | Item/Reagent | Function/Application | Key Considerations |
|---|---|---|---|
| Wet-Lab Reagents | HMW-gDNA Extraction Kit | Isolate long, intact genomic DNA for long-read sequencing. | Minimize shearing; assess integrity via pulse-field gel electrophoresis. |
| Illumina DNA Prep Kit | Prepare sequencing libraries for short-read, high-accuracy platforms. | Standard for high-coverage, base-accurate data. | |
| Oxford Nanopore Ligation Kit | Prepare libraries for long-read sequencing on Nanopore devices. | Critical for resolving repetitive regions and genome structure. | |
| Reference Materials | ATCC Standard Reference Genomes (ASRGs) | Authenticated, high-quality genome references with full data provenance. | Mitigates risks of using mislabeled or low-quality public references [58]. |
| PubMLST cgMLST Schemas | Defined sets of core genes for standardized bacterial typing. | Essential for reproducible outbreak investigation and population genetics [57]. | |
| Software & Databases | Unicycler | Hybrid genome assembler. | Recommended over SPAdes or Shovill for hybrid datasets for superior contiguity [59] [57]. |
| PROKKA & PGAP | Prokaryotic genome annotation pipelines. | PROKKA for speed; PGAP for comprehensiveness and NCBI compatibility [56]. | |
| AMRFinderPlus & CARD | AMR gene/mutation identification and reference database. | More comprehensive than alternatives like Abricate; includes point mutations [36]. | |
| GenomeQC | Integrated tool for assembly and annotation quality assessment. | Calculates BUSCO, LAI, N50, and checks for contamination in one pipeline [60]. |
Annotation Curation and Data Provenance
Even with the best automated pipelines, manual curation remains essential. Studies reveal that approximately 2.1% and 0.9% of coding sequences annotated by RAST and PROKKA, respectively, may be erroneous, with errors frequently associated with short genes (<150 nt) such as transposases and hypothetical proteins [59]. A dedicated curation step involving manual inspection of these specific gene categories is highly recommended.
Furthermore, ensuring robust data provenance—a complete record of the journey from biological sample to final genome assembly—is critical for microbial genomics. Research indicates that a significant portion of assemblies in public databases like RefSeq lack vital metadata on sequencing technology, assembly method, and, most importantly, traceability to an authenticated source material [58]. The following workflow and practices ensure data integrity and reproducibility.
Diagram 2: Critical data provenance pathway for traceable and authentic genome data.
Adhering to this pathway mitigates the risks identified in studies of public databases, where widespread discrepancies in assembly quality, genetic variability, and metadata completeness have been observed [58]. For reliable comparative genomics, establishing and documenting this chain of custody from the original biological material to the final annotated genome is as important as the computational analysis itself.
Managing Metagenome-Assembled Genomes (MAGs) and Unculturable Pathogens
The genomic study of bacterial pathogens has been fundamentally transformed by culture-independent techniques, which are crucial for analyzing the vast majority of microorganisms that resist laboratory cultivation [62] [63]. Metagenome-assembled genomes (MAGs) represent reconstructed genomes from complex microbial communities, enabling researchers to access the genetic blueprint of unculturable pathogens and the broader microbial dark matter [62] [64]. Within comparative genomic analyses of bacterial pathogens, MAGs provide an indispensable tool for discovering novel virulence factors, antibiotic resistance mechanisms, and evolutionary pathways across diverse ecological niches [9]. This protocol details integrated methodologies for generating high-quality MAGs, cultivating challenging pathogens, and leveraging these resources for comparative genomic investigations with direct implications for drug development and public health.
Metagenome-Assembled Genomes: Generation and Quality Control
Workflow for MAG Generation and Validation
The process of obtaining MAGs from environmental or host-associated samples involves multiple critical steps, from sample preservation to genome refinement, each requiring stringent quality control measures to ensure biological relevance [62] [65].
MAG Quality Standards and Interpretation
Table 1: Quality Assessment Categories for Metagenome-Assembled Genomes
| Quality Category | Completeness | Contamination | Quality Implications for Comparative Genomics |
|---|---|---|---|
| High-quality draft | >90% | <5% | Suitable for detailed phylogenetic analysis and metabolic reconstruction [64] |
| Medium-quality draft | ≥50% | <10% | Useful for presence/absence analysis of specific virulence or resistance genes [64] |
| Low-quality draft | <50% | <10% | Limited to single-gene surveys or marker-based analyses [64] |
| Not recommended | Any | ≥10% | Excluded from publication; requires further refinement [65] |
Biological validation of MAGs remains challenging. MAGs are considered "hypothetical" (HMAGs) when no reference genome exists for comparison, and gain credibility as "conserved hypothetical" (CHMAGs) when identical populations are identified in independent studies [64]. Confirmation is strongest when MAGs align with isolate genomes from unrelated sources with ≥97% average nucleotide identity and ≥90% coverage [64].
Cultivation Techniques for Unculturable Pathogens
Advanced Cultivation Methodologies
Despite advances in sequencing, axenic cultures remain essential for characterizing phenotypic traits, validating metabolic predictions, and providing reference genomes [66]. Several innovative approaches have successfully targeted previously unculturable pathogens.
Table 2: Cultivation Methods for Unculturable Bacterial Pathogens
| Method | Principle | Application Example | Success Rate | Key Considerations |
|---|---|---|---|---|
| High-throughput dilution-to-extinction | Serial dilution in low-nutrient media to isolate slow-growing oligotrophs | Isolation of abundant freshwater lineages (e.g., Planktophila, Fontibacterium) [66] | 627 axenic strains from 14 lakes; representing up to 72% of genera in original samples [66] | Requires defined media mimicking natural conditions; 6-8 week incubation [66] |
| Diffusion-based encapsulation | Semi-permeable capsules allow nutrient/waste exchange while protecting cells | Magnetic PDMS spheres enable growth in native environments (soil, seawater) [67] | ~50,000 cells/nanoliter from 5 starting cells; concentrated cultures [67] | Enables chemical testing and cell interaction studies; magnetic recovery [67] |
| Co-culture approaches | Leveraging microbial dependencies (nutrient sharing, detoxification) | Growth of auxotrophic microbes requiring metabolites from helper strains [66] | Essential for microorganisms with multiple auxotrophies [66] | Requires identification of synergistic partners; complex community modeling |
Integrating Cultivation with Metagenomic Insights
Genomic data from MAGs can guide cultivation strategies through "reverse genomics," where predicted metabolic requirements inform media composition [66]. This cyclic process of genomic prediction followed by cultivation validation significantly enhances the recovery of novel pathogens.
Comparative Genomic Analysis Framework
Analytical Workflow for Pathogen Genomics
The integration of MAGs and cultured genomes enables comprehensive comparative analyses of bacterial pathogens across different ecological niches and hosts.
Table 3: Essential Bioinformatics Databases for Comparative Pathogen Analysis
| Database | Primary Function | Application in Pathogen Genomics | Access Platform |
|---|---|---|---|
| COG Database | Protein functional classification | Identifying conserved core genes and niche-specific adaptations [9] | RPS-BLAST with e-value <0.01, coverage >70% [9] |
| VFDB (Virulence Factor Database) | Catalog of bacterial virulence factors | Characterizing pathogenicity mechanisms across strains [9] | VirulenceFinder (≥90% coverage, ≥95% identity) [68] |
| CARD (Comprehensive Antibiotic Resistance Database) | Antibiotic resistance ontology | Profiling resistance gene distribution and emergence [9] | BLAST-based alignment with threshold filtering [9] |
| CAZy (Carbohydrate-Active Enzymes) | Glycoside hydrolases and related enzymes | Understanding host-microbe interactions and nutrient acquisition [9] | dbCAN2 (HMMER with e-value <1e-5) [9] |
| GTDB (Genome Taxonomy Database) | Standardized microbial taxonomy | Phylogenetic placement of novel MAGs and isolates [66] [64] | GTDB-tk for automated classification [64] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents and Computational Tools for MAG and Pathogen Studies
| Reagent/Tool | Category | Specific Function | Application Notes |
|---|---|---|---|
| Nucleic acid preservation buffers | Sample Collection | Stabilize community DNA/RNA during storage/transport | RNAlater, OMNIgene.GUT for host-associated samples; critical for integrity [62] |
| Defined artificial media | Cultivation | Mimic natural nutrient conditions for oligotrophs | med2/med3 (1.1-1.3 mg DOC/L); MM-med for methylotrophs [66] |
| Magnetic PDMS capsules | Advanced Cultivation | Semi-permeable growth chambers for in situ cultivation | 6,000 spheres/min; iron oxide enables magnetic retrieval [67] |
| CheckM | Quality Control | Assess MAG completeness/contamination using marker genes | Standard for MAG quality evaluation pre-publication [64] [65] |
| MetaWRAP/Anvi'o | Bioinformatics | Binning refinement and visualization of MAGs | Interactive interface for manual curation of automated bins [64] [65] |
| Scoary | Comparative Genomics | Identify pan-genome associations with phenotypes | Machine learning enhancement for adaptive gene detection [9] |
The integrated application of MAG generation, advanced cultivation techniques, and comparative genomic analysis provides a powerful framework for elucidating the biology of unculturable bacterial pathogens. The protocols outlined herein enable researchers to bridge the gap between genomic potential and phenotypic expression, facilitating the discovery of novel therapeutic targets and resistance mechanisms. As these methodologies continue to evolve, they will undoubtedly expand our understanding of pathogen evolution and host adaptation, ultimately informing new strategies for combating infectious diseases in an era of increasing antimicrobial resistance.
The rise of whole-genome sequencing (WGS) has revolutionized the surveillance and study of bacterial pathogens, enabling high-resolution analysis for outbreak investigation, antimicrobial resistance (AMR) tracking, and molecular epidemiology [69]. The One Health perspective, which integrates human, animal, and environmental health, requires not only interdisciplinary cooperation but also standardized methods for communicating and archiving data [70]. A core challenge, however, lies in ensuring that the genomic data and associated metadata generated by diverse laboratories and projects are interoperable—that they can be seamlessly integrated, exchanged, and analyzed across different resources and computational tools. Without such interoperability, even the largest genomic datasets can become isolated in silos, limiting their utility for public health and research. This application note outlines the best practices, protocols, and key resources for ensuring data interoperability in comparative genomic analyses of bacterial pathogens.
The Need for Standardization in Pathogen Genomics
The value of genomic data is magnified when it can be compared across studies, time, and geographical boundaries. Inconsistent data description, analysis, and storage methods pose a significant risk of creating data silos, even within the same pathogen surveillance community [70]. The FAIR principles (Findable, Accessible, Interoperable, and Re-usable) provide a guiding framework for maximizing data utility. Interoperability, a key component, allows different systems to use and build upon the data for various purposes, such as:
- Outbreak Detection: Identifying and tracking the spread of bacterial strains.
- Antibiotic Resistance Monitoring: Surveillance of AMR genes across human, animal, and environmental isolates.
- Comparative Genomics: Investigating the genetic basis of host adaptation, virulence, and other phenotypic traits [9] [71].
Centralized, open-access databases and adherence to community standards are foundational to achieving these goals.
Several international resources provide the infrastructure for storing and analyzing pathogen genomic data. Adhering to their data standards is the first critical step toward interoperability.
Table 1: Key Public Resources for Pathogen Genomic Data
| Resource Name | Primary Function | Key Features & Supported Data | Data Submission Standards |
|---|---|---|---|
| NCBI Pathogen Detection [70] | Integrated analysis platform | Real-time phylogenetic clustering; AMR, virulence, and stress gene screening; houses data from >32 pathogens. | WGS data; standardized metadata templates; specific QC thresholds (e.g., for sequence quality). |
| International Nucleotide Sequence Database Collaboration (INSDC) [70] | Core archival database | Synchronizes data daily across NCBI, EMBL-EBI, and DDBJ; forms the foundation for many other tools. | Raw sequence reads (FASTQ) and/or assembled genomes (FASTA). |
| EnteroBase [72] | Curated database and analysis platform | cgMLST genotyping; hierarchical clustering; AMR genotype analysis for specific genera; user-friendly visualization tools (e.g., bubble plots). | WGS data and associated metadata; supports direct upload or integration via NCBI SRA. |
The Role of Metadata
High-quality, standardized metadata is as crucial as the sequence data itself for enabling meaningful comparisons. Inconsistent or incomplete metadata severely hampers the ability to integrate datasets. Key metadata attributes for interoperability include:
- Isolation source (e.g., human, animal, food, environment) [70] [9]
- Date and location of isolation
- Laboratory and methodological data (e.g., sequencing platform, assembly method)
Protocols for Ensuring Data Interoperability
The following protocols provide a practical roadmap for generating and submitting genomic data that is interoperable from the start.
Protocol: Whole-Genome Sequencing and DNA Preparation
This protocol is adapted from a beginner-friendly method for obtaining WGS data from a range of bacteria, including Gram-positive, Gram-negative, and acid-fast species [73].
I. Materials (Research Reagent Solutions)
- Lysozyme: For bacterial cell lysis.
- DNeasy Blood and Tissue Kit (Qiagen) or High Pure PCR Template Preparation Kit (Roche): For genomic DNA extraction and purification.
- Qubit dsDNA HS Assay Kit (Invitrogen): For accurate DNA quantification.
- Nextera XT Library Preparation Kit (Illumina): For DNA library preparation.
- Agencourt AMPure XP beads (Beckman Coulter): For library purification.
II. Method
- DNA Extraction:
- Pellet 200 µl of a liquid bacterial culture by centrifuging at 8000 g for 8 minutes.
- Resuspend the pellet in 600 µl phosphate-buffered saline (PBS).
- Add 30 µl lysozyme (50 mg/ml), vortex, and incubate at 37°C for 1 hour.
- Follow the manufacturer's protocol for the DNeasy Blood and Tissue Kit to extract DNA.
- Elute DNA in 100 µl volume and treat with 2 µl RNase (100 mg/ml); incubate at room temperature for 1 hour.
- Further purify the DNA using the High Pure PCR Template Preparation Kit, eluting in 50 µl of pre-heated elution buffer. Critical Step: Contaminant-free, high-molecular-weight DNA with a 260/280 nm absorbance ratio of 1.8–2.0 is essential for high-quality sequencing [73].
DNA Quantification:
- Quantify the purified DNA using the Qubit dsDNA HS Assay Kit according to the manufacturer's instructions.
- Adjust the DNA concentration of each sample to 0.2 ng/µl using distilled water. Critical Step: An accurate DNA concentration is crucial for successful library preparation [73].
Library Preparation and Sequencing:
- Use the Nextera XT Library Preparation Kit for tagmentation and PCR amplification, following the kit's protocol.
- Perform library quantification and normalization.
- Sequence the library on an Illumina MiSeq or similar platform using a v2 (300-cycle) reagent kit.
The following workflow diagram summarizes the key steps in this WGS protocol:
Protocol: Data Submission to Public Repositories
Submitting data to public repositories like NCBI is a critical step for ensuring data accessibility and interoperability [70].
I. Prerequisites
- WGS data in FASTQ format.
- A complete and standardized metadata table.
II. Method
- Sequence Quality Control (QC):
- Assess the quality of your WGS data using tools like FastQC.
- Follow community standards for WGS quality. The GenomeTrakr Best Practices recommend specific QC thresholds, such as a minimum coverage depth and completeness, which can be models for other projects [70].
Metadata Curation:
Data Submission:
- Submit raw sequence data (FASTQ files) to the NCBI Sequence Read Archive (SRA).
- Associate the SRA accession with your isolate in the NCBI Pathogen Detection database, providing the curated metadata.
- Update and curate your public data as needed to keep it current within the database [70].
Downstream Analysis and Integration Tools
Once data is submitted to a central repository, a variety of tools can leverage this interoperable data for specialized analyses.
Table 2: Selected Platforms for Analyzing Interoperable Genomic Data
| Platform / Tool | Analysis Type | Application in Comparative Genomics |
|---|---|---|
| EnteroBase [72] | cgMLST, Hierarchical Clustering | Population genetics; outbreak investigation; AMR genotype visualization across large datasets. |
| NextStrain [70] | Phylogenetics, Visualization | Real-time tracking of pathogen evolution and spread. |
| IRIDA [70] | Genomic Epidemiology | Platform for managing, analyzing, and sharing genomic data in public health labs. |
| NCBI Pathogen Detection [70] | Automated Phylogenetics, AMR Screening | Real-time identification of emerging clusters and resistance threats. |
| GWAS & Machine Learning [9] | Comparative Genomics, Gene-Trait Association | Identifying genetic variants and signature genes associated with host adaptation or virulence. |
The integration between these tools and central databases is key. For instance, the relationship between data sources, analysis platforms, and end-users can be visualized as follows:
Case Study: Comparative Genomics for Host Adaptation
A 2025 comparative genomic study exemplifies the power of interoperable data. The research analyzed 4,366 high-quality bacterial genomes from human, animal, and environmental sources to identify niche-specific adaptations [9].
Methods:
- Genomes were annotated using COG, dbCAN, VFDB, and CARD databases for functional, virulence, and AMR profiling.
- Phylogenetic analysis was performed using 31 universal single-copy genes.
- Machine learning and genome-wide association studies (GWAS) were used to identify host-specific signature genes.
Key Findings:
- Human-associated bacteria (e.g., Pseudomonadota) had more virulence factors and carbohydrate-active enzyme genes.
- Environmental bacteria showed enrichment in metabolic and transcriptional regulation genes.
- Clinical isolates carried a higher burden of fluoroquinolone resistance genes.
- The gene
hypBwas identified as a potential human host-specific signature gene, possibly regulating metabolism and immune adaptation.
This study highlights how standardized, interoperable data from diverse sources enables the discovery of fundamental genetic mechanisms underlying pathogen evolution and transmission.
Optimizing Feature Selection for Machine Learning Models in Genomics
In the era of big data genomics, feature selection has emerged as a critical preprocessing step for building robust machine learning (ML) models, particularly in comparative genomic studies of bacterial pathogens. The extraordinary volume and dimensionality of genomic data—where features (e.g., genes, single-nucleotide polymorphisms) often vastly outnumber samples—create significant analytical challenges collectively known as the "curse of dimensionality" [74] [75]. Effective feature selection mitigates this problem by identifying and retaining the most informative genomic features while discarding irrelevant or redundant ones, thus improving model performance, computational efficiency, and interpretability [75] [76].
For bacterial pathogen research, feature selection enables researchers to pinpoint specific genetic elements underlying critical phenotypes such as host adaptation, antibiotic resistance, and virulence mechanisms [9] [25]. By reducing the feature space to biologically relevant candidates, feature selection transforms unstructured genomic data into tractable datasets capable of generating testable hypotheses about pathogen behavior and evolution [77]. This protocol provides a comprehensive framework for optimizing feature selection strategies specifically tailored for microbial genomics applications, with practical guidance applicable across diverse research scenarios.
Feature Selection Methodologies: A Comparative Framework
Feature selection techniques generally fall into three primary categories—filter, wrapper, and embedded methods—each with distinct mechanisms, advantages, and limitations [74] [76]. Understanding these methodological differences is essential for selecting appropriate approaches for specific research questions in bacterial genomics.
Table 1: Categories of Feature Selection Methods in Genomics
| Method Type | Mechanism | Advantages | Disadvantages | Common Algorithms |
|---|---|---|---|---|
| Filter Methods | Selects features based on statistical measures independent of ML model | Fast computation; Scalable to high-dimensional data; Less prone to overfitting | Ignores feature dependencies; May select redundant features; Model-agnostic | Differential expression analysis [76]; Chi-square test [75]; Mutual information [74] |
| Wrapper Methods | Uses ML model performance as evaluation criterion for feature subsets | Captures feature interactions; Model-specific selection; Generally high performance | Computationally intensive; Risk of overfitting; Slower with large feature spaces | Recursive Feature Elimination [78]; Genetic Algorithms [76]; Forward/Backward Selection [76] |
| Embedded Methods | Performs feature selection as part of model construction process | Balances performance and computation; Model-specific selection; Considers feature interactions | Algorithm-dependent; Less generic than filter methods | LASSO regression [76]; Random Forest importance [77] [78]; Tree-based methods [76] |
Beyond these core categories, hybrid approaches that combine multiple methodologies are increasingly common in genomic studies [74] [76]. Ensemble feature selection methods aggregate results from multiple base selectors to improve stability and generalizability, while integrative methods incorporate external biological knowledge to guide feature selection [76]. These advanced approaches are particularly valuable when analyzing complex microbial genomic datasets where biological interpretation is paramount.
Experimental Protocols for Genomic Feature Selection
Protocol 1: Comparative Genomics Workflow for Identifying Lifestyle-Associated Genes
Objective: To identify bacterial genes associated with specific ecological niches or lifestyles (e.g., pathogenicity) using a comparative genomics approach with integrated feature selection.
Materials and Reagents:
- Hardware: High-performance computing cluster with minimum 16 cores, 64GB RAM
- Software: bacLIFE workflow [77], Prokka [9], MMseqs2 [77], R or Python with scikit-learn
- Data: Assembled bacterial genomes in FASTA format with associated metadata
Procedure:
- Data Curation and Quality Control
- Collect genome assemblies from public repositories or sequencing projects
- Perform rigorous quality assessment using CheckM or similar tools: retain genomes with ≥95% completeness and <5% contamination [9] [25]
- Annotate ecological niches (e.g., human pathogen, animal pathogen, environmental) based on isolation source metadata [9]
Genome Annotation and Gene Clustering
Feature Selection and Machine Learning
- Train a Random Forest classifier using gene cluster presence-absence matrix to predict lifestyle categories
- Apply feature importance scoring (e.g., Gini importance or permutation importance) to identify predictive gene clusters
- Select top-ranked features based on importance scores and statistical significance
- Validate selected features through cross-validation and independent test sets
Experimental Validation
- Select candidate genes for functional validation using site-directed mutagenesis
- Conduct phenotypic assays (e.g., plant infection models for phytopathogens) to confirm role in lifestyle adaptation [77]
- Confirm true lifestyle-associated genes (LAGs) through statistical analysis of phenotypic differences
Troubleshooting Tips:
- If model performance is poor, ensure adequate sample size per lifestyle category (minimum 50 genomes per category recommended)
- If feature selection identifies too many candidates, increase stringency of importance thresholds or incorporate additional biological filters
- Address phylogenetic confounding by including evolutionary relationships as covariates in the model
Protocol 2: Dimensionality Reduction for Single-Cell Genomic Integration
Objective: To optimize feature selection for single-cell RNA sequencing data integration and reference mapping, enabling effective comparison across bacterial populations.
Materials and Reagents:
- Hardware: Computing workstation with 32GB+ RAM
- Software: Scanpy [79], Scikit-learn [79], Single-cell variational inference (scVI) [79]
- Data: Single-cell RNA sequencing count matrices with batch information
Procedure:
- Data Preprocessing
- Load and quality control scRNA-seq data using Scanpy
- Filter cells with low counts (<1000 genes detected) and genes detected in few cells (<10 cells)
- Normalize counts per cell and log-transform
Feature Selection Implementation
- Apply highly variable gene selection using the Scanpy implementation of Seurat algorithm [79]
- Test alternative selection methods: batch-aware feature selection, lineage-specific selection, or stable gene selection
- Select optimal number of features (typically 2,000-5,000) based on preliminary integration performance
Data Integration and Benchmarking
- Integrate datasets using scVI or similar integration method with selected features
- Evaluate integration quality using multiple metrics: batch correction (Batch PCR), biological conservation (isolated label F1), and query mapping (cell distance) [79]
- Compare performance across feature selection methods using standardized benchmarking pipeline
Downstream Analysis
- Project query datasets onto reference atlas using selected features
- Transfer cell-type labels and identify novel cell states
- Perform differential expression analysis within integrated space
Troubleshooting Tips:
- If integration fails to preserve biological variation, reduce the number of selected features or try lineage-specific selection
- If batch effects persist, implement batch-aware feature selection methods
- For large datasets, subset features initially then expand based on performance
Visualization of Feature Selection Workflows
Workflow for Comparative Genomic Analysis
Figure 1: Comparative genomics workflow for identifying lifestyle-associated genes in bacterial pathogens, integrating feature selection with experimental validation [9] [77].
Feature Selection Method Classification
Figure 2: Taxonomy of feature selection methods applicable to genomic studies, showing primary categories with example algorithms [74] [75] [76].
Table 2: Key Research Reagents and Computational Tools for Genomic Feature Selection
| Category | Item | Specifications | Application/Function |
|---|---|---|---|
| Bioinformatics Databases | VFDB (Virulence Factor Database) | Version: Current release | Annotation of virulence factors in bacterial genomes [9] [25] |
| CARD (Comprehensive Antibiotic Resistance Database) | Version: Current release | Identification of antibiotic resistance genes [9] [25] | |
| COG (Cluster of Orthologous Groups) | e-value: 0.01, Coverage: 70% | Functional categorization of gene products [9] [25] | |
| CAZy (Carbohydrate-Active Enzymes) | HMMER e-value: 1e-5 | Annotation of carbohydrate-active enzymes [9] | |
| Computational Tools | bacLIFE workflow | Version: GitHub latest | Comparative genomics and lifestyle-associated gene prediction [77] |
| Scikit-learn | Version: ≥1.0 | Machine learning and feature selection implementation [79] [80] | |
| Scanpy | Version: ≥1.9 | Single-cell data analysis and highly variable gene selection [79] | |
| Prokka | Version: 1.14.6 | Rapid prokaryotic genome annotation [9] | |
| ML Algorithms | Random Forest | Default parameters initially | Classification and feature importance ranking [77] [78] |
| LASSO Regression | Alpha optimized via cross-validation | Sarse feature selection for regression tasks [76] | |
| Recursive Feature Elimination | Step size: 10% of features | Wrapper feature selection with various estimators [78] |
Performance Benchmarking and Best Practices
Recent benchmarking studies provide critical insights for selecting appropriate feature selection methods in genomic applications. For single-cell RNA sequencing data integration, highly variable gene selection consistently outperforms random feature selection, with 2,000 features typically representing an optimal balance between information content and dimensionality [79]. For microbial metabarcoding datasets, Random Forest models often perform robustly even without additional feature selection, though Recursive Feature Elimination can provide modest improvements for specific tasks [78].
Table 3: Performance Comparison of Feature Selection Methods Across Genomic Data Types
| Data Type | Optimal Method | Performance Metrics | Key Considerations |
|---|---|---|---|
| Comparative Genomics (Bacterial Pathogens) | Random Forest with importance thresholding | AUC: 0.85-0.95 for lifestyle prediction [77] | Gene clustering at appropriate identity threshold critical [77] |
| Single-cell RNA-seq | Highly variable genes (Scanpy/Seurat) | Batch correction: >0.7 Batch PCR; Biological conservation: >0.8 isolated label F1 [79] | Number of features (2,000-5,000) impacts performance [79] |
| Microbial Metabarcoding | Random Forest without feature selection | Regression tasks: R² >0.6; Classification: AUC >0.8 [78] | Ensemble models robust to high dimensionality [78] |
| GWAS/SNP Data | Embedded methods (LASSO, Elastic Net) | Phenotype prediction accuracy: 65-80% [75] | Linkage disequilibrium creates feature redundancy [75] |
When implementing feature selection for bacterial genomic studies, consider these evidence-based recommendations:
Dataset-Specific Optimization: The optimal feature selection approach depends on dataset characteristics including sample size, feature dimensionality, and biological question [78]. Conduct preliminary benchmarking with subsetted data before committing to a full analysis pipeline.
Biological Interpretation: Prioritize methods that generate interpretable feature importance scores when biological insight is the primary goal [77] [80]. Random Forest variable importance and LASSO coefficients provide transparent feature rankings.
Computational Efficiency: For large-scale genomic datasets (>1,000 samples), filter methods or embedded methods generally offer better scalability than wrapper approaches [74] [76].
Validation Strategy: Always validate selected features through cross-validation, independent test sets, and when possible, experimental confirmation [77]. This is particularly critical when feature selection guides downstream biological investigations.
Optimized feature selection is fundamental to extracting meaningful biological insights from complex genomic datasets of bacterial pathogens. By implementing the protocols and guidelines presented herein, researchers can significantly enhance their ability to identify genetic determinants of clinically and ecologically relevant phenotypes. The integration of computational feature selection with experimental validation, as exemplified by the bacLIFE workflow, represents a powerful paradigm for advancing our understanding of bacterial adaptation and evolution. As genomic datasets continue to grow in size and complexity, refined feature selection strategies will remain essential for translating sequence data into biological knowledge with implications for infectious disease management, antibiotic development, and public health interventions.
Best Practices for Integrating Genomic and Clinical Metadata
The comparative genomic analysis of bacterial pathogens has been revolutionized by high-throughput sequencing technologies, generating unprecedented amounts of genomic data. However, the full potential of this genomic information remains limited without robust integration with clinical patient metadata—demographic, epidemiological, and outcome data that provides essential clinical context [81] [82]. This integration is crucial for understanding pathogen transmission dynamics, virulence mechanisms, and the relationship between genetic variation and clinical disease presentation [9] [25].
Despite its importance, significant challenges impede effective metadata integration, including disparities in data collection practices, lack of standardization, and complex legal and privacy frameworks governing clinical data [81] [83]. This article outlines established best practices and detailed protocols for successfully integrating genomic and clinical metadata, with a specific focus on applications in bacterial pathogen research.
Core Principles and Challenges
The Critical Role of Metadata Integrity
Metadata serves as the foundational layer that makes genomic data interpretable and reusable. In biomedical research, metadata integrity is a fundamental determinant of research credibility, supporting the reliability and reproducibility of data-driven findings [83]. The FAIR Guiding Principles (Findable, Accessible, Interoperable, and Reusable) provide a framework for managing metadata, emphasizing that metadata must be richly described with accurate and relevant attributes to enable reuse by other researchers [83].
Common challenges in metadata management include:
- Inconsistent data collection: Variable practices across institutions and research groups lead to incompatible datasets [81] [84]
- Limited metadata completeness: GenBank records contain only 21.6% of host metadata on average, severely limiting their utility for analyses requiring clinical correlation [82]
- Semantic misalignment: Differences in terminology and coding systems create barriers to interoperability [84]
Special Considerations for Bacterial Pathogen Research
Comparative genomics of bacterial pathogens presents unique metadata requirements. Research has revealed that bacterial pathogens employ distinct genomic adaptation strategies based on their ecological niches—human, animal, or environmental [9] [25]. Human-associated bacteria from the phylum Pseudomonadota exhibit higher detection rates of virulence factors related to immune modulation, while environmental isolates show greater enrichment in metabolic genes [25]. These findings highlight the necessity of collecting detailed information about isolation source, host characteristics, and environmental context to properly interpret genomic variations.
Table 1: Essential Metadata Categories for Bacterial Pathogen Research
| Category | Specific Elements | Research Significance |
|---|---|---|
| Sample Context | Isolation source (clinical, environmental, animal), collection date, geographic location | Enables analysis of spatiotemporal patterns and ecological adaptations [9] [25] |
| Host Information | Host species, age, sex, immune status, comorbidities | Facilitates understanding of host-pathogen interactions and risk stratification [82] [25] |
| Clinical Data | Disease outcome, severity metrics, treatment regimen, antimicrobial resistance | Allows correlation of genomic features with clinical manifestations [81] [82] |
| Genomic Processing | Sequencing platform, assembly method, annotation pipeline, quality metrics | Ensures reproducibility and interoperability of genomic analyses [85] |
Methodological Framework
Metadata Collection and Management Protocol
Protocol 1: Creating Comprehensive Metadata Schemas
- Define core metadata elements based on research objectives and community standards
- Implement structured data dictionaries that explicitly define each field, acceptable values, and formatting rules
- Ensure compatibility with relevant ontologies such as SNOMED CT for clinical terms [82] [84]
- Establish data validation rules to maintain consistency and quality at the point of entry [85]
Best Practice: Create tidy data structures where every column represents a variable, every row represents an observation, and every cell contains a single value [85]. Avoid storing data in formats that may corrupt content (e.g., Excel files that may convert gene names to dates) [85].
Protocol 2: Ensuring FAIR Compliance
- Assign persistent identifiers to both genomic data and associated metadata
- Use standardized communication protocols for data retrieval
- Employ formal knowledge representation languages for metadata structure
- Provide rich provenance information describing the origin and processing history of data [83]
Data Integration Workflows
The integration of genomic and clinical metadata can be accomplished through multiple computational approaches, depending on available data and research goals.
Protocol 3: Data-Driven Integration Using K-Nearest Neighbors (KNN)
This method connects existing databases that share common variables but lack direct linkage [81].
- Prepare initial dataset: Must contain at least time (YY-MM-DD format) and incidence columns, plus additional variables as available [81]
- Provide learning dataset: Contains a shared variable (X) present in both datasets and an additional variable (Y) to be added to the initial dataset [81]
- Apply KNN classification: The algorithm learns the relationship between X and Y in the learning dataset [81]
- Predict missing values: Implement the trained KNN model to predict realistic values for the Y variable in the initial dataset based on X variable values [81]
- Validate integration: Compare a subset of predicted values with actual values (if available) to assess integration quality
Protocol 4: Random Simulation for Missing Data
When learning datasets are unavailable, random simulation provides an alternative approach [81].
- Define new categorical variables: Specify variable name and all possible levels (e.g., vaccination status with levels: unvaccinated, first dose, second dose) [81]
- Set proportional distribution: Assign appropriate proportions for each level based on research scenario requirements [81]
- Generate simulated values: Randomly assign values to samples according to specified proportions
- Adjust relative risks: Modify proportions of variable levels within specific patient groups based on levels of other variables to meet scenario objectives [81]
Table 2: Metadata Integration Methods Comparison
| Method | Requirements | Applications | Limitations |
|---|---|---|---|
| Data-Driven Simulation (KNN) [81] | Learning dataset with shared variable and target variable | Integrating datasets with partial overlap; Adding demographic or clinical variables to genomic datasets | Dependent on quality and representativeness of learning dataset |
| Random Simulation [81] | Variable definition and proportional distribution | Scenario planning; Training exercises; Sensitivity analysis | May not capture complex real-world correlations |
| Relative Risk Adjustment [81] | Existing integrated dataset; Target relative risk values | Creating specific training scenarios; Modeling intervention effects | Requires initial integrated dataset |
| Multimodal AI Integration [86] | Diverse data types (genomic, clinical, imaging); Substantial computational resources | Complex pattern recognition; Predictive modeling; Personalized treatment strategies | Computationally intensive; Requires large, curated datasets |
Implementation Tools and Quality Control
Computational Tools and Platforms
Several specialized tools facilitate the integration of genomic and clinical metadata:
- PANDEM-2 Simulator: An R package and Shiny application that enables realistic linking of pathogen molecular data with patient contextual metadata for training and research purposes [81]
- Health Metadata Catalogs (HMDCs): Decentralized systems that enhance discoverability, usability, and management of distributed datasets while ensuring legally compliant access [87]
- Transformers and Graph Neural Networks: Advanced AI approaches that effectively integrate heterogeneous data types, including clinical notes, genomic data, and imaging information [86]
Protocol 5: Quality Control and Validation
- Implement automated metadata checks: Use computational tools to identify formatting inconsistencies, missing values, and outlier entries [83]
- Conduct manual validation: Perform targeted manual review of metadata entries, particularly for critical variables
- Assess integration quality: Compare distributions of integrated variables against expected values from source datasets
- Verify data integrity: Ensure integrated datasets maintain biological and clinical plausibility through expert review
The Researcher's Toolkit
Table 3: Essential Research Reagent Solutions for Genomic-Clinical Integration
| Tool/Resource | Function | Application Context |
|---|---|---|
| R Statistical Environment [81] | Data manipulation, statistical analysis, and visualization | Primary platform for data integration and analysis |
| Pandem2simulator R Package [81] | Multi-parametric simulation linking genomic and clinical data | Creating realistic training scenarios and analytical datasets |
| dbCAN2 [9] [25] | Annotation of carbohydrate-active enzyme genes | Functional characterization of bacterial genomes |
| VFDB (Virulence Factor Database) [9] [25] | Identification of bacterial virulence genes | Assessing pathogenic potential of bacterial isolates |
| CARD (Comprehensive Antibiotic Resistance Database) [9] [25] | Annotation of antibiotic resistance genes | Predicting antimicrobial resistance profiles |
| ABRicate [25] | Mass screening of genomic sequences for resistance and virulence genes | Rapid characterization of bacterial pathogen genomes |
| Nextclade [82] | Clade assignment, quality control, and mutation identification | Phylogenetic analysis and genomic surveillance |
| IQ-TREE [82] | Phylogenetic reconstruction with model selection | Evolutionary analysis of pathogen genomes |
| CheckM [9] [25] | Assessment of genome completeness and contamination | Quality control of genome assemblies |
| Prokka [25] | Rapid annotation of prokaryotic genomes | Functional annotation of bacterial sequences |
Advanced Applications and Future Directions
Emerging Methodologies
Multimodal Artificial Intelligence represents the cutting edge of genomic-clinical data integration. Transformer-based models and Graph Neural Networks (GNNs) show particular promise for capturing complex relationships between diverse data types [86]. These approaches can explicitly model non-Euclidean relationships in healthcare data, potentially identifying novel associations between genetic markers and clinical outcomes [86].
Protocol 6: Implementing Graph Neural Networks for Metadata Integration
- Represent data as graphs: Structure heterogeneous data points (genomic variants, clinical features, patient demographics) as nodes in a graph [86]
- Define edge relationships: Establish connections based on biological relationships, clinical associations, or temporal sequences [86]
- Apply convolutional operations: Adapt GNN architectures to aggregate feature information from neighboring nodes [86]
- Train model parameters: Optimize for specific predictive tasks such as virulence prediction or treatment outcome forecasting [86]
- Validate model performance: Assess generalizability across different pathogen types and clinical settings [86]
Case Study: SARS-CoV-2 Metadata Enhancement
A recent framework for strengthening pathogen genomics using SARS-CoV-2 demonstrates the value of metadata enrichment [82]. Researchers systematically extracted patient metadata from scientific literature and integrated it with genomic sequences from GenBank, enabling analyses that revealed associations between viral mutations and patient clinical outcomes [82]. This approach facilitated the identification of how immune status and comorbidities influence within-host viral evolution—findings that would not have been possible with genomic data alone [82].
The integration of genomic and clinical metadata represents a critical frontier in bacterial pathogen research. By implementing robust methodologies for metadata collection, standardization, and integration, researchers can unlock deeper insights into host-pathogen interactions, transmission dynamics, and the genetic basis of clinical outcomes. The protocols and frameworks outlined here provide a practical foundation for enhancing genomic studies with essential clinical context, ultimately advancing both scientific understanding and public health response to bacterial pathogens.
As the field evolves, emerging technologies—particularly multimodal AI and federated data ecosystems—promise to further overcome current limitations in data integration. By adhering to established best practices while embracing innovative approaches, researchers can maximize the value of both genomic and clinical data assets, accelerating progress in combating infectious diseases.
Benchmarks and Case Studies: Validating Genomic Predictions Across Pathogens
Framework for Validating Predicted Virulence and Resistance Genes
Within the field of comparative genomic analysis of bacterial pathogens, the initial in silico identification of virulence and antimicrobial resistance genes is only the first step. The true challenge lies in the rigorous biological validation of these computational predictions to confirm their functional role in pathogenesis and resistance. This framework provides detailed application notes and protocols for confirming the activity of predicted genes, bridging the gap between genomic data and biological significance for researchers, scientists, and drug development professionals. The integration of these validation techniques is crucial for advancing our understanding of host-pathogen interactions and for developing novel therapeutic strategies to combat multidrug-resistant infections.
Experimental Protocols for Validation
Genomic DNA Extraction and Whole-Genome Sequencing
Principle: High-quality genomic DNA is essential for all downstream genomic analyses, including sequencing and validation experiments. This protocol ensures the isolation of pure, intact DNA suitable for next-generation sequencing platforms [88] [89].
Reagents and Equipment:
- Wizard Genomic DNA purification kit (Promega) or equivalent [88]
- DNeasy UltraClean Microbial Kit (Qiagen) or Maxwell RSC Blood DNA extraction kit [90] [91]
- Luria-Bertani broth (Carl Roth GmbH) or modified Agarose Medium (m-AAM) with antibiotics [88] [90]
- Qubit Fluorometer (Life Technologies) or NanoDrop Spectrophotometer (ThermoFisher) [88] [90]
- Incubator for microbial culture (30°C-37°C, microaerophilic conditions when necessary) [88]
Procedure:
- Inoculate bacterial strains into appropriate liquid media (e.g., Luria-Bertani broth, m-AAM) and incubate overnight at optimal growth temperature (varies by species, typically 30°C-37°C) under appropriate atmospheric conditions [88].
- Harvest bacterial cells by centrifugation at 5,000 × g for 10 minutes.
- Purify genomic DNA using commercial kits according to manufacturer's instructions [88] [90].
- Determine DNA concentration and purity using fluorometric or spectrophotometric methods [88] [90].
- Assess DNA quality by agarose gel electrophoresis to confirm high molecular weight and absence of degradation.
- For long-term storage, preserve DNA at -20°C [88].
Quality Control:
- DNA purity: A260/A280 ratio of ~1.8-2.0
- Minimum concentration: >20 ng/μL for sequencing applications
- High molecular weight without RNA contamination
Bioinformatic Identification of Target Genes
Principle: Computational pipelines enable comprehensive screening of bacterial genomes for virulence and resistance genes through comparison with curated databases [9] [92] [35].
Reagents and Software:
- ABRicate tool (v1.0.1) for resistance and virulence gene screening [90] [92] [89]
- AMRFinderPlus (v3.10+) for comprehensive resistance gene identification [90]
- Virulence Factor Database (VFDB) for virulence-associated genes [9] [35]
- Comprehensive Antibiotic Resistance Database (CARD) [9] [92]
- ResFinder for acquired resistance genes [90] [89]
- Prokka (v1.14.5+) for genome annotation [9] [90] [89]
- Quality control tools: FastQC (v0.11.7), CheckM (v1.0.18), QUAST (v5.0.2+) [90] [89]
Procedure:
- Perform quality control on raw sequencing reads using FastQC [90].
- Assemble genomes de novo using SPAdes (v3.15+) or similar assemblers [90].
- Assess assembly quality with QUAST and CheckM (completeness ≥95%, contamination <5%) [9] [89].
- Annotate assembled genomes using Prokka to identify open reading frames [9] [89].
- Screen for virulence genes using ABRicate with VFDB [90] [92] [89].
- Identify antimicrobial resistance genes using ABRicate with CARD, ResFinder, and/or AMRFinderPlus [90] [92] [89].
- Confirm positive hits based on coverage (>70%) and identity thresholds (typically >90%) [9].
Phenotypic Antimicrobial Susceptibility Testing
Principle: Broth microdilution methods provide quantitative measurements of bacterial susceptibility to antimicrobial agents, allowing correlation between genotypic predictions and phenotypic expression [93].
Reagents and Equipment:
- Cation-adjusted Mueller-Hinton broth
- Antibiotic stock solutions of known potency
- Sterile 96-well microtiter plates
- Automated inoculation systems (e.g., VITEK2) or manual multichannel pipettes [91]
- Spectrophotometer or plate reader
Procedure:
- Prepare antibiotic working solutions in cation-adjusted Mueller-Hinton broth following CLSI guidelines.
- Dispense serial dilutions of antibiotics into 96-well microtiter plates.
- Adjust bacterial inoculum to 0.5 McFarland standard (~1.5 × 10^8 CFU/mL) in sterile saline.
- Further dilute inoculum in broth to achieve final concentration of approximately 5 × 10^5 CFU/mL per well.
- Incubate plates at 35°C ± 2°C for 16-20 hours.
- Determine Minimum Inhibitory Concentration (MIC) as the lowest antibiotic concentration completely inhibiting visible growth.
- Interpret results according to CLSI or EUCAST breakpoints.
Quality Control:
- Include appropriate reference strains with known MIC values
- Monitor incubation conditions and inoculum purity
- Document all procedures for regulatory compliance
PCR Confirmation of Identified Genes
Principle: Polymerase chain reaction provides specific amplification and detection of predicted virulence and resistance genes, confirming their physical presence in the bacterial genome [88].
Reagents and Equipment:
- Taq DNA polymerase with reaction buffer
- Deoxynucleotide triphosphates (dNTPs)
- Sequence-specific primers (typically 18-25 nucleotides)
- Thermal cycler
- Agarose gel electrophoresis equipment
- DNA molecular weight markers
Procedure:
- Design primers flanking the target gene sequence with melting temperatures of 55-65°C.
- Prepare PCR reaction mix containing: 1× reaction buffer, 1.5-2.5 mM MgCl2, 200 μM each dNTP, 0.2-0.5 μM each primer, 0.5-1 U Taq polymerase, and 10-100 ng template DNA.
- Perform amplification using optimized thermal cycling conditions:
- Initial denaturation: 95°C for 3-5 minutes
- 30-35 cycles of: 95°C for 30 seconds, primer-specific annealing temperature (50-65°C) for 30 seconds, 72°C for 1 minute per kb
- Final extension: 72°C for 5-7 minutes
- Analyze PCR products by agarose gel electrophoresis (1.5-2.0%) with appropriate DNA size markers.
- Visualize amplified fragments under UV light after ethidium bromide or SYBR Safe staining.
Troubleshooting:
- Optimize annealing temperature for specific primer pairs
- Adjust MgCl2 concentration if non-specific amplification occurs
- Include positive and negative controls in each run
Data Presentation and Analysis
Quantitative Comparison of Virulence and Resistance Genes
Table 1: Distribution of virulence genes across different ecological niches based on comparative genomic analysis of 4,366 bacterial genomes [9]
| Virulence Factor Category | Human-Associated Bacteria (%) | Animal-Associated Bacteria (%) | Environmental Bacteria (%) | Clinical Isolates (%) |
|---|---|---|---|---|
| Immune Evasion Factors | 78.3 | 45.2 | 12.6 | 85.7 |
| Adhesion Proteins | 82.5 | 51.8 | 18.9 | 88.3 |
| Toxin Genes | 65.7 | 58.3 | 22.4 | 79.2 |
| Secretion Systems | 71.9 | 48.6 | 35.2 | 83.5 |
| Biofilm Formation | 75.4 | 42.7 | 28.5 | 91.6 |
Table 2: Prevalence of antimicrobial resistance genes in different bacterial populations [9] [90] [93]
| Resistance Mechanism | Human Isolates (%) | Animal Isolates (%) | Environmental Isolates (%) | MDR Prevalence (%) |
|---|---|---|---|---|
| β-lactamase Genes | 68.5 | 55.3 | 32.7 | 92.1 |
| Fluoroquinolone Resistance | 45.2 | 38.7 | 18.9 | 87.6 |
| Aminoglycoside Resistance | 52.8 | 47.5 | 25.3 | 78.9 |
| Tetracycline Resistance | 58.3 | 62.1 | 41.6 | 72.4 |
| Multidrug Efflux Pumps | 75.6 | 58.9 | 35.8 | 94.3 |
Table 3: Essential research reagents and databases for virulence and resistance gene validation
| Research Reagent/Database | Primary Function | Application Context |
|---|---|---|
| VFDB (Virulence Factor Database) | Comprehensive repository of bacterial virulence factors | Annotation and identification of virulence genes in genomic data [9] [35] |
| CARD (Comprehensive Antibiotic Resistance Database) | Curated collection of resistance genes, mechanisms, and targets | Prediction of antibiotic resistance profiles from genomic data [9] [90] [92] |
| ABRicate | Screening tool for antimicrobial resistance and virulence genes | Rapid annotation of resistance and virulence genes in assembled genomes [92] [89] |
| ResFinder | Identification of acquired antimicrobial resistance genes | Detection of horizontally acquired resistance mechanisms [90] [89] |
| CheckM | Quality assessment of microbial genomes | Evaluation of genome completeness and contamination [9] [89] |
| AMRFinderPlus | Comprehensive identification of resistance genes | Detection of resistance mechanisms including point mutations [90] |
Workflow Visualization
Integrated Validation Framework
Genomic Validation Workflow
Bioinformatics Analysis Pipeline
Bioinformatics Analysis Pipeline
Discussion and Technical Notes
Implementation Considerations
The validation framework presented here integrates multiple complementary approaches to confirm the functional significance of predicted virulence and resistance genes. Successful implementation requires careful consideration of several technical aspects. For genomic analyses, quality thresholds are critical; genome assemblies should demonstrate ≥95% completeness with <5% contamination as evaluated by CheckM [9] [89]. For gene identification, coverage thresholds of ≥70% and identity thresholds of ≥90% provide optimal balance between sensitivity and specificity when using databases such as VFDB and CARD [9].
Recent advances in comparative genomics have revealed that bacterial adaptive strategies differ significantly across ecological niches. Human-associated pathogens, particularly those from the phylum Pseudomonadota, demonstrate higher prevalence of carbohydrate-active enzyme genes and virulence factors related to immune modulation and adhesion, reflecting co-evolution with human hosts [9]. In contrast, environmental isolates show greater enrichment of metabolic and transcriptional regulation genes. These niche-specific patterns should inform the selection of appropriate reference strains and positive controls for validation experiments.
Troubleshooting Common Challenges
Discrepancies between genotypic predictions and phenotypic results may arise from several sources. Undetected point mutations in regulatory regions can affect gene expression without altering coding sequences. When phenotypic resistance is observed without corresponding genetic determinants, investigate efflux pump activity (e.g., through efflux pump inhibitors) or novel resistance mechanisms [94]. For virulence genes, consider potential epigenetic regulation or condition-dependent expression that may not be detected under standard laboratory conditions.
PCR validation failures despite positive bioinformatic predictions warrant verification of primer specificity and assessment of potential sequence variations in primer binding sites. Additionally, consider that some virulence genes may be present in genomic islands or plasmids that are difficult to assemble from short-read sequencing data [95]. In such cases, long-read sequencing technologies (e.g., Oxford Nanopore) can provide improved resolution of mobile genetic elements and repetitive regions [91].
Emerging Applications in Drug Development
The validated genetic determinants of virulence and resistance provide valuable targets for novel therapeutic approaches. Anti-virulence strategies represent a promising alternative to conventional antibiotics, with the VFDB currently cataloging 902 anti-virulence compounds across 17 superclasses [35]. These compounds target diverse virulence mechanisms including adhesion, biofilm formation, quorum sensing, and toxin production. The integration of validation data with compound screening efforts accelerates the identification of lead compounds with specific anti-virulence activity.
For antimicrobial resistance, validated genetic markers enable the development of rapid molecular diagnostics that can detect resistance mechanisms directly from clinical specimens, potentially reducing the time to appropriate therapy from days to hours [91]. This is particularly valuable for tracking the dissemination of high-risk clones, such as Staphylococcus epidermidis CC2 in musculoskeletal infections or emerging sequence types of Klebsiella pneumoniae [93] [91].
Cross-species transmission of zoonotic pathogens represents a significant global public health threat, accounting for approximately 60% of emerging infectious diseases [96]. Suidae (pig family), for example, are critical intermediate hosts in viral spillover events due to their widespread distribution and close contact with humans [97]. Comparative genomics provides a powerful framework to dissect the genetic determinants enabling host switching, integrating viral characteristics, host factors, and environmental variables [98]. This protocol outlines a data-driven approach for assessing cross-species transmission risk, emphasizing bacterial pathogens within the One Health context. The methodologies include predictive modeling, genomic analysis, and experimental workflows to identify high-risk pathogens and inform targeted interventions.
Key Quantitative Data on Zoonotic Transmission Risks
Analysis of historical and genomic data reveals critical factors influencing cross-species transmission. The table below summarizes predictive modeling performance and risk factors derived from studies on Suidae-associated viruses, which are relevant to bacterial pathogen research frameworks.
Table 1: Performance Metrics of Predictive Models for Cross-Species Transmission
| Model | Sensitivity | Specificity | Accuracy | Balanced Accuracy | AUC |
|---|---|---|---|---|---|
| Logistic Regression (LR) | 0.681 | 0.717 | 0.716 | 0.699 | 0.699 |
| Boosted Regression Trees (BRT) | 0.653 | 0.807 | 0.803 | 0.730 | 0.804 |
| Decision Tree (DT) | 0.702 | 0.744 | 0.743 | 0.723 | 0.723 |
| Random Forest (RF) | 0.319 | 0.960 | 0.946 | 0.640 | 0.640 |
| Support Vector Machine (SVM) | 0.722 | 0.747 | 0.747 | 0.735 | 0.735 |
Source: Adapted from analysis of human-Suidae viruses (1882–2022) [97].
Table 2: Top Predictors of Cross-Species Transmission Risk
| Predictor | Relative Influence (%) | Role in Transmission |
|---|---|---|
| Host–human phylogenetic distance | 28.50 | Closer genetic proximity increases spillover propensity. |
| Viral genome size | 18.55 | Larger genomes may enhance adaptive capacity in new hosts. |
| Rural human population density | 11.29 | Higher density elevates human–animal interaction opportunities. |
| Annual precipitation | 9.72 | Climate conditions affect pathogen persistence and spread. |
| Artificial surface coverage | 9.65 | Land-use changes disrupt ecosystems and promote spillover. |
Source: Boosted Regression Trees analysis of zoonotic viruses [97].
Experimental Protocols for Cross-Species Analysis
Protocol 1: Predictive Modeling of Transmission Risk
Objective: Identify high-risk pathogens using integrated genomic and ecological data. Workflow:
- Data Collection:
- Pathogen genomic data from NCBI Virus Database [97].
- Host phylogenetic data from TimeTree.
- Environmental variables (e.g., precipitation, artificial surfaces) from WorldClim and FAOSTAT.
- Feature Integration:
- Annotate viral attributes (genome size, envelope presence, replication site).
- Calculate host–human phylogenetic divergence times.
- Model Training:
- Use Boosted Regression Trees (BRT) with a learning rate of 0.01, tree complexity of 3, and 10-fold cross-validation.
- Optimize hyperparameters via grid search.
- Validation:
- Assess performance using AUC, sensitivity, and specificity.
- Apply to unknown pathogens (e.g., Porcine circovirus 3 showed >90% risk) [97].
Protocol 2: Comparative Genomics for Genetic Determinants
Objective: Identify genetic elements facilitating host switching in bacterial pathogens. Workflow:
- Genome Sequencing:
- Use next-generation sequencing (NGS) for high-throughput data generation [96].
- Orthology Mapping:
- Map genes via ENSEMBL for one-to-one orthologs [99].
- Variant Analysis:
- Identify mutations in receptor-binding domains and virulence factors.
- Compare genomes across hosts to detect adaptive changes [98].
- Functional Annotation:
- Use ViralZone and ICTV Master Species List for standardized taxonomy [97].
Protocol 3: Cross-Species Single-Cell Transcriptomic Integration
Objective: Compare cellular responses to pathogens across species. Workflow:
- Single-Cell RNA Sequencing (scRNA-seq):
- Profile cells from multiple species (e.g., mouse, human, opossum) [100].
- Data Integration:
- Cross-Species Prediction:
- Train models on one species to predict gene expression in another.
- Validation:
- Use Adjusted Rand Index (ARI) to evaluate annotation transfer accuracy [99].
Visualization of Workflows
Below are DOT scripts for generating diagrams of the experimental protocols. Each diagram uses the specified color palette (#4285F4, #EA4335, #FBBC05, #34A853, #FFFFFF, #F1F3F4, #202124, #5F6368).
Diagram 1: Predictive Modeling Workflow
Title: Predictive Modeling Pipeline
Diagram 2: Comparative Genomics Analysis
Title: Comparative Genomics Workflow
Diagram 3: Single-Cell Cross-Species Integration
Title: Single-Cell Integration Pipeline
Research Reagent Solutions
Table 3: Essential Reagents and Tools for Cross-Species Analysis
| Reagent/Tool | Function | Example Use Case |
|---|---|---|
| NCBI Virus Database | Provides genomic data on zoonotic pathogens | Data collection for predictive modeling [97] |
| ENSEMBL Orthology Mapping | Maps gene homologs across species | Comparative genomics of bacterial pathogens [99] |
| Boosted Regression Trees (BRT) | Predicts cross-species transmission risk | Risk assessment for emerging pathogens [97] |
| Icebear Neural Network | Decomposes species-specific effects in scRNA-seq | Cross-species gene expression prediction [100] |
| Next-Generation Sequencing (NGS) | High-throughput genome sequencing | Pathogen genomic characterization [96] |
| SeuratV4/scANVI | Integrates single-cell data across species | Cell-type matching and annotation transfer [99] |
Integrating predictive modeling, comparative genomics, and single-cell transcriptomics provides a robust framework for analyzing cross-species transmission of bacterial pathogens. Standardized protocols and reagent solutions enable researchers to identify high-risk pathogens, dissect genetic determinants of host switching, and inform One Health interventions [97] [98] [96]. Future work should expand genomic databases and incorporate artificial intelligence for real-time risk assessment.
Wohlfahrtiimonas chitiniclastica is an emerging zoonotic pathogen belonging to the class Gammaproteobacteria [101]. First isolated from the larvae of the parasitic fly Wohlfahrtia magnifica, this Gram-negative, oxidase-positive, non-motile bacillus has been increasingly recognized as a cause of human infections including sepsis, bacteremia, and soft tissue infections, particularly in immunocompromised patients or those with open wounds infested by fly larvae [101] [102]. The bacterium exhibits strong chitinase activity, potentially facilitating a symbiotic relationship with its host fly during metamorphosis [101].
Recent comparative genomic analyses reveal that W. chitiniclastica possesses a rapidly expanding resistome, characterized by both intrinsic resistance mechanisms and acquired antimicrobial resistance (AMR) genes distributed among its core and accessory genomes [103] [104]. This resistance gene expansion poses significant challenges for clinical management of infections and underscores the importance of ongoing genomic surveillance within the One Health framework, which recognizes the interconnectedness of human, animal, and environmental health [105]. This case study examines the mechanisms and implications of resistance gene expansion in W. chitiniclastica through the lens of comparative genomic analysis.
Genomic Features and Resistance Landscape
The pan-genome of W. chitiniclastica comprises 3,819 genes with 1,622 core genes (approximately 43%), indicating a metabolically conserved species with moderate genomic diversity [103] [104]. In silico analyses have revealed a concerning expansion of its resistome, facilitated by genome-encoded transposons and bacteriophages that enable horizontal gene transfer [103].
Distribution of Antimicrobial Resistance Genes
Table 1: Antimicrobial Resistance Genotypes in W. chitiniclastica
| Antibiotic Class | Resistance Genes | Genomic Location |
|---|---|---|
| Macrolides | macA, macB | Core genome |
| Tetracyclines | tetH, tetB, tetD | Accessory genome |
| Aminoglycosides | ant(2″)-Ia, aac(6′)-Ia, aph(3″)-Ib, aph(3′)-Ia, aph(6)-Id | Accessory genome |
| Sulfonamides | sul2 | Accessory genome |
| Streptomycin | strA | Accessory genome |
| Chloramphenicol | cat3 | Accessory genome |
| Beta-lactams | blaVEB | Accessory genome |
Notably, the type strain DSM 18708ᵀ does not encode additional clinically relevant antibiotic resistance genes beyond the core macrolide resistance genes macA and macB, suggesting that antimicrobial resistance is increasing within the W. chitiniclastica clade through acquisition of mobile genetic elements [103] [104]. This trend warrants careful monitoring as it may complicate treatment options for infections caused by this emerging pathogen.
Experimental Protocols for Genomic Analysis
Genome Sequencing and Assembly
Protocol: Whole Genome Sequencing and Assembly for Resistome Analysis
DNA Extraction: Use commercial kits (e.g., Qiagen DNeasy Blood & Tissue Kit) to extract high-quality genomic DNA from pure bacterial cultures. Assess DNA quality and quantity using spectrophotometry (e.g., NanoDrop) and fluorometry (e.g., Qubit).
Library Preparation and Sequencing:
- Prepare sequencing libraries using Illumina DNA Prep kit following manufacturer's instructions.
- For long-read sequencing, utilize Oxford Nanopore Technologies ligation sequencing kits.
- Perform quality control on prepared libraries using Bioanalyzer or TapeStation.
Sequencing:
- Conduct paired-end sequencing (2×150 bp) on Illumina platforms (e.g., MiSeq, NextSeq) to achieve minimum 50× coverage.
- For hybrid assembly approaches, complement with Oxford Nanopore sequencing to resolve repetitive regions and mobile genetic elements.
Genome Assembly:
- Quality-trim raw reads using Trimmomatic v0.39 with parameters: LEADING:3 TRAILING:3 SLIDINGWINDOW:4:15 MINLEN:36.
- Perform de novo assembly using Unicycler v0.5.0 with default parameters for hybrid assembly of short and long reads.
- Assess assembly quality using QUAST v5.0.2, with benchmarks including N50 > 50,000 bp and contig number minimized.
Annotation:
In Silico Resistance Gene Identification
Protocol: Comprehensive Resistome Analysis
Reference Database Curation:
- Download the Comprehensive Antibiotic Resistance Database (CARD) and ResFinder databases locally.
- Update databases to ensure inclusion of latest resistance gene variants.
Resistance Gene Screening:
- Use the Resistance Gene Identifier (RGI) tool against CARD with "Perfect and Strict hits only" and "High Quality/Coverage" parameters [104].
- Complement with ABRicate v1.0.1 against multiple databases (CARD, ResFinder, ARG-ANNOT) using 80% identity and 90% coverage thresholds.
Mobile Genetic Element Analysis:
Plasmid Reconstruction:
- Reconstruct plasmid sequences from whole genome sequencing data using plasmidSPAdes v3.15.4.
- Confirm plasmid circularity and identity using BLASTn against plasmid databases.
Data Integration:
- Compile results from various tools into a comprehensive resistome profile.
- Visualize genomic context of resistance genes using circular genome maps or linear synteny plots.
Figure 1: Workflow for Genomic Analysis of W. chitiniclastica Resistome. The diagram outlines the key steps from bacterial isolation to comprehensive resistome profiling, highlighting the integration of multiple database queries and mobile genetic element analysis.
Key Research Reagent Solutions
Table 2: Essential Research Reagents and Tools for W. chitiniclastica Genomic Analysis
| Category | Specific Tool/Reagent | Application/Function |
|---|---|---|
| Wet Lab | Qiagen DNeasy Blood & Tissue Kit | High-quality genomic DNA extraction |
| Illumina DNA Prep Kit | Library preparation for short-read sequencing | |
| Oxford Nanopore Ligation Sequencing Kit | Long-read sequencing for resolving repeats | |
| Brain Heart Infusion Agar | Culture of W. chitiniclastica isolates | |
| Bioinformatics | Prokka v1.14.6 | Rapid prokaryotic genome annotation [104] |
| CARD Database | Comprehensive reference for resistance genes [106] | |
| ResFinder/PointFinder | Detection of acquired resistance genes/mutations [106] | |
| PHASTER | Identification and analysis of prophage sequences [104] | |
| Unicycler v0.5.0 | Hybrid assembly of short and long reads | |
| CRISPRCasFinder | Detection of CRISPR-Cas systems [104] |
Genomic Insights into Resistance Mechanisms
Core versus Accessory Resistome
The W. chitiniclastica genome demonstrates a fundamental division between core and accessory resistance elements. The macrolide resistance genes macA and macB are consistently present in the core genome of all analyzed strains, suggesting an intrinsic resistance mechanism conserved across the species [103] [104]. In contrast, resistance genes for other antibiotic classes including tetracyclines, aminoglycosides, sulfonamides, and beta-lactams are variably distributed among the accessory genome, indicating recent acquisition through horizontal gene transfer events [103].
The presence of these accessory resistance genes on mobile genetic elements is particularly concerning from a public health perspective. Recent studies have identified novel insertion sequences (ISWoch1, ISWoch2, and ISWoch3) in W. chitiniclastica plasmids that facilitate the mobilization of resistance genes such as blaVEB-1 [107]. These insertion sequences can provide strong promoters that enhance expression of adjacent resistance genes, further amplifying the resistance phenotype.
Mobile Genetic Elements and Resistance Gene Dissemination
Comparative genomic analyses have revealed that W. chitiniclastica strains harbor various mobile genetic elements that contribute to resistome expansion. These include:
Plasmids: The identification of novel blaVEB-1-carrying plasmids in W. chitiniclastica highlights the role of conjugative elements in resistance gene dissemination [107]. These plasmids often carry multiple resistance determinants, enabling multi-drug resistance profiles.
Bacteriophages: In silico analysis using PHASTER has identified intact prophage sequences in several W. chitiniclastica genomes, suggesting transduction as a potential mechanism for gene transfer [104].
Transposons and Insertion Sequences: The accessory genome of W. chitiniclastica is enriched with transposable elements that facilitate intra-genomic mobilization of resistance genes [103].
Figure 2: Mechanisms of Resistance Gene Expansion in W. chitiniclastica. The diagram illustrates how horizontal gene transfer via mobile genetic elements contributes to the expansion of the accessory resistome, leading to enhanced antimicrobial resistance profiles.
Discussion and Future Perspectives
The genomic analysis of W. chitiniclastica reveals a pathogen in transition, with an expanding resistome that poses challenges for clinical management. Several factors contribute to this concerning trajectory:
First, the ecological niche of W. chitiniclastica as a fly-associated bacterium brings it into contact with diverse microbial communities in the environment, creating opportunities for horizontal gene transfer [102]. The bacterium's presence in multiple habitats including arsenic-contaminated soil, chicken meat, and various animal species further increases the likelihood of encountering resistance determinants from other bacteria [102].
Second, the clinical management of W. chitiniclastica infections is complicated by its variable resistance profile. While most strains remain susceptible to quinolones and trimethoprim/sulfamethoxazole, the emergence of extended-spectrum beta-lactamase genes like blaVEB-1 is alarming [107]. Furthermore, the intrinsic resistance to fosfomycin observed in many isolates appears to be mediated by fosfomycin efflux proteins and transferases, though the precise genetic basis requires further elucidation [102] [107].
From a methodological perspective, the integration of whole genome sequencing with advanced bioinformatics tools provides unprecedented capability to monitor resistance gene expansion in real-time. The use of platforms like CARD and ResFinder enables standardized annotation of resistance determinants, while tools like PHASTER and CRISPRCasFinder facilitate analysis of mobile genetic elements that drive resistome evolution [106] [104].
Future research should focus on several key areas:
- Functional validation of putative resistance genes through molecular techniques
- Investigation of resistance gene transfer between W. chitiniclastica and co-infecting pathogens
- Development of rapid diagnostic methods to detect resistant W. chitiniclastica strains in clinical settings
- Expanded surveillance of W. chitiniclastica in animal and environmental reservoirs to understand One Health dynamics
In conclusion, W. chitiniclastica serves as an instructive model for studying resistance gene expansion in an emerging pathogen. Its dynamic genome, facilitated by mobile genetic elements, demonstrates the rapidity with which bacterial pathogens can acquire resistance traits. Ongoing genomic surveillance within a One Health framework is essential to monitor these evolutionary developments and inform clinical practice.
The One Health concept recognizes that the health of humans, animals, and ecosystems are interconnected. Applying comparative genomics within this framework involves using whole-genome sequencing to track zoonotic pathogens across these domains, enabling high-resolution surveillance and outbreak investigation. This approach has revolutionized our ability to detect pathogens and trace the spread of infections in near real-time, providing critical insights for public health action [108]. The integration of genomic data with epidemiological information allows researchers to investigate transmission chains, explore large-scale population dynamics such as the spread of antibiotic resistance, and identify key infection sources to inform interventions for local and global health security [109] [108].
Despite its utility, the implementation of genomic surveillance across One Health domains faces significant challenges. A 2024 scoping review revealed that sampling and sequencing efforts vary considerably across domains: the median number of pathogen genomes analyzed was highest for humans and lowest for the environmental domain [108]. Furthermore, while bacterial pathogens have been extensively studied, significant knowledge gaps remain for other zoonotic agents, particularly arboviruses [108]. To address these challenges and maximize the potential of pathogen genomics, researchers must work toward standardizing bioinformatics workflows, building computational capacity across public health agencies, and developing consistent data models that maintain crucial linkages between genomic sequences and their associated epidemiological metadata [109] [110].
Key Applications and Protocols
Core Applications in One Health Research
Comparative genomics within the One Health framework supports several critical applications in public health and disease research as shown in the table below.
Table 1: Key Applications of Comparative Genomics in One Health
| Application | Protocol Description | Key Tools & Techniques |
|---|---|---|
| Outbreak Source Tracking | Phylogenetic reconstruction to identify transmission pathways and infection sources across domains. | Whole-genome sequencing, phylogenetic analysis (Harvest Suite, Gubbins) [111]. |
| Antimicrobial Resistance (AMR) Surveillance | Detection and tracking of resistance genes across human, animal, and environmental isolates. | In silico resistance detection (CARD, ARG-Annot, ResFinder), phylogenetic placement [111]. |
| Pathogen Evolution Studies | Analysis of evolutionary dynamics driving lineage diversification, virulence, and host adaptation. | Synteny analysis (MCscan), recombination detection (Gubbins), positive selection analysis [111] [112]. |
| Cross-Species Transmission Detection | Identification of genetic adaptations associated with host jumping and establishment in new reservoirs. | Comparative genomics, single nucleotide polymorphism (SNP) analysis, pangenome analysis [108]. |
Standardized Protocol for Cross-Domain Pathogen Investigation
Protocol Title: Integrated Genomic Investigation of Zoonotic Pathogens Across One Health Domains
Objective: To provide a standardized methodology for generating, analyzing, and interpreting whole-genome sequence data from human, animal, and environmental samples to trace transmission pathways and characterize genetic determinants of zoonotic potential.
Experimental Workflow:
Diagram 1: Integrated Genomic Investigation Workflow
Step-by-Step Methodology:
Sample Collection and Study Design:
- Collect matched samples from human, animal, and environmental sources during outbreak investigations or surveillance programs.
- Record comprehensive metadata using a hierarchical data model that maintains linkages between case information, sample details, and sequence data [109].
- The data model should include:
- Case field: Host species, age, sex, symptoms, geographic information
- Sample field: Collection date, medium, culture information, case identifier
- Sequence field: Genomic region, sequence type, accession numbers, case and sample identifiers [109]
Nucleic Acid Extraction and Sequencing:
- Extract DNA/RNA using standardized kits suitable for the pathogen type.
- Perform quality control on nucleic acids using spectrophotometric (e.g., Nanodrop) and fluorometric (e.g., Qubit) methods.
- Prepare sequencing libraries using compatible protocols for short-read (Illumina) or long-read (PacBio, Oxford Nanopore) platforms.
- Sequence genomes to an appropriate depth of coverage (typically >50x for bacterial pathogens).
Genome Assembly and Annotation:
- Assess read quality using FastQC and perform necessary trimming/filtering.
- Perform de novo assembly using SPAdes (for bacterial genomes) or other appropriate assemblers [111].
- Evaluate assembly quality using QUAST, which provides metrics on contiguity (N50, number of contigs) and completeness [111].
- Anicate assembled genomes using:
Comparative Genomic Analysis:
- Identify genomic variants: Call core genome SNPs using Parsnp (part of the Harvest Suite) or similar tools for phylogenetic analysis [111].
- Detect recombination: Use Gubbins to identify and account for recombinant regions in phylogenetic analyses [111].
- Analyze specific genetic elements:
- Perform synteny analysis: Use MCscan (within the JCVI toolkit) to identify conserved gene order and chromosomal rearrangements across strains [112].
Phylogenetic Reconstruction and Data Integration:
- Construct phylogenies using core genome SNPs with appropriate evolutionary models.
- Integrate temporal, spatial, and host species data to create phylodynamic models.
- Interpret phylogenetic patterns in the context of One Health metadata to infer cross-species transmission events and directionality.
- Visualize results using tools such as Gingr (for phylogeny and SNP visualization) or BRIG (for circular genome comparisons) [111].
Essential Bioinformatics Tools and Data Visualization
Table 2: Essential Bioinformatics Tools for One Health Comparative Genomics
| Tool Name | Category | Specific Function | Application in One Health |
|---|---|---|---|
| SPAdes | Genome Assembly | De Bruijn graph assembler for small genomes | Assembly of bacterial pathogens from all domains [111] |
| RAST/Prokka | Genome Annotation | Functional annotation of coding sequences | Standardized gene calling across isolates from different hosts [111] |
| Harvest Suite (Parsnp/Gingr) | Phylogenetics | Core genome SNP identification & visualization | High-resolution tracking of transmission pathways [111] |
| JCVI Library | Comparative Genomics | Synteny analysis, graphics generation | Visualization of genomic conservation across strains [112] |
| CARD/ResFinder | AMR Detection | Database of resistance genes & mutations | Tracking AMR spread across human-animal-environment interfaces [111] |
| Gubbins | Recombination Detection | Identification of recombination events | Improves phylogenetic accuracy by removing horizontally transferred regions [111] |
| SRST2 | Read Mapping | Direct MLST & gene detection from reads | Rapid typing without assembly for outbreak investigations [111] |
Data Integration and Visualization Framework
Effective integration of genomic and metadata is crucial for One Health insights. The following framework illustrates how to synthesize these data types:
Diagram 2: One Health Data Integration Framework
Standards and Best Practices
To ensure reproducibility and interoperability in One Health genomic studies, researchers should adhere to developing standards in the field:
- Data Hygiene and Metadata Management: Implement consistent data models that maintain crucial linkages between sequence data and associated metadata (host, date, location, clinical information) [109].
- Bioinformatics Software Standards: Follow guidelines proposed by the Public Health Alliance for Genomic Epidemiology (PHA4GE) for developing and implementing bioinformatics software, focusing on quality, reliability, and sustainability [110].
- Workflow Reproducibility: Use containerization (Docker, Singularity) and workflow managers (Nextflow, Snakemake) to ensure consistent analysis across studies and research groups.
- Data Sharing: Deposit raw sequencing data in public repositories (SRA, ENA) with complete metadata to enable comparative analyses and global surveillance efforts.
Comparative genomics applied within a One Health framework provides powerful approaches for understanding and mitigating zoonotic disease threats. By integrating genomic data from human, animal, and environmental sources, researchers can track pathogen transmission across domains, identify genetic determinants of host adaptation, and inform targeted interventions. The protocols and tools outlined here provide a foundation for standardized, reproducible analyses that can enhance global health security through collaborative, cross-disciplinary investigations.
Leveraging NIH Comparative Genomics Resource (CGR) for Reproducible Analysis
This application note provides a detailed protocol for employing the NIH Comparative Genomics Resource (CGR) to conduct reproducible comparative genomic analyses of bacterial pathogens. We demonstrate a standardized workflow using Wohlfahrtiimonas chitiniclastica as a case study to identify pathogenic factors, characterize antimicrobial resistance (AMR) genes, and analyze phage content. The methodology emphasizes utilization of CGR's interconnected data repositories and analytical tools to ensure research rigor, reproducibility, and compliance with NIH data sharing policies. Designed for researchers, scientists, and drug development professionals, this protocol facilitates reliable genomic investigations that can inform therapeutic development and public health responses.
The NIH Comparative Genomics Resource (CGR) is a multi-year project led by the National Library of Medicine (NLM) and NCBI to maximize the impact of eukaryotic research organisms and their genomic data on biomedical research [113]. CGR facilitates reliable comparative genomics analyses through community collaboration and an NCBI toolkit of interconnected and interoperable data and tools [114]. The project aims to enhance biomedical discovery by providing high-quality genomic data, new and improved comparative genomics tools, and scalable analyses that support big data approaches and cloud-based workflows [113] [115].
CGR's development is guided by FAIR principles (Findable, Accessible, Interoperable, Reusable), making genomic data easier to search, browse, download, and use with various bioinformatics platforms [113]. For bacterial pathogen research, CGR offers organism-agnostic tools that provide equal access to datasets across the tree of life, enabling researchers to expose biological information and reveal patterns that can spur new hypotheses for future investigations [113]. The resource is particularly valuable for studying emerging pathogens and their genetic mechanisms of virulence and resistance.
CGR Toolkit for Bacterial Pathogen Analysis
Table 1: Essential NCBI CGR Components for Bacterial Pathogen Research
| Tool/Resource | Primary Function | Application in Pathogen Analysis |
|---|---|---|
| NCBI Datasets | Browse and download genomic data, including sequences, annotation, and metadata | Retrieve complete genome assemblies, gene sequences, and associated metadata for multiple bacterial strains |
| BLAST | Find regions of similarity between sequences | Identify homologous virulence factors, resistance genes, and conserved genomic regions across pathogens |
| ClusteredNR | Explore evolutionary relationships and identify related organisms | Determine phylogenetic relationships and genetic diversity among bacterial isolates |
| Comparative Genome Viewer (CGV) | Visualize and compare genome assemblies | Identify genomic rearrangements, insertions, deletions, and structural variations among pathogen strains |
| Genome Data Viewer (GDV) | Explore and analyze genomic region annotations | Examine genomic context of virulence factors and resistance genes |
| Foreign Contamination Screening (FCS) | Quality assurance process for sequence data | Detect and remove contaminating sequences from genome assemblies prior to analysis |
| Assembly Quality Control (QC) | Evaluate genome assembly for completeness, correctness, and base accuracy | Verify quality of human, mouse, or rat pathogen genome assemblies |
Workflow for Reproducible Pathogen Genomics
The following diagram illustrates the comprehensive workflow for analyzing bacterial pathogens using CGR tools, ensuring complete reproducibility:
Experimental Protocol: Comparative Genomic Analysis ofWohlfahrtiimonas chitiniclastica
Background and Rationale
Wohlfahrtiimonas chitiniclastica is an emerging Gram-negative bacterial pathogen first isolated from the larvae of Wohlfahrtia magnifica [5]. Recent studies indicate it can cause severe human infections including sepsis and bacteremia, making it a previously underappreciated human pathogen [5]. Systematic genomic studies are necessary to understand its virulence characteristics and treatment options. This protocol uses all publicly available W. chitiniclastica genomes (n=26 as of April 2021) to demonstrate a reproducible CGR workflow for pathogen analysis.
Materials and Reagent Solutions
Table 2: Essential Research Reagents and Computational Tools for CGR Analysis
| Item | Function/Purpose | Source/Availability |
|---|---|---|
| Public Genomic Data | Raw material for comparative analysis | NCBI repositories (GenBank, SRA) |
| Reference Genomes | Baseline for comparison and annotation | NCBI Assembly Database |
| Antimicrobial Resistance Databases | Reference for identifying resistance genes | CARD, NCBI AMR Finder |
| Virulence Factor Databases | Reference for identifying virulence genes | VFDB, PATRIC |
| Prophage Prediction Tools | Identification of integrated phage elements | PhiSpy, PHASTER |
| CRISPR Detection Tools | Identification of CRISPR arrays | CRISPRFinder, PILER-CR |
| Annotation Pipelines | Standardized gene calling and functional annotation | NCBI PGAP, Prokka |
| Pan-genome Analysis Tools | Determine core and accessory genome | Roary, Panaroo |
Step-by-Step Methodology
Genomic Data Collection and Curation
Strain Selection and Retrieval: Identify all publicly available W. chitiniclastica genomes through NCBI Genome database. Include type strain DSM 18708T (AQXD01000000) as reference [5].
Data Download: Utilize NCBI Datasets to download all available genomes in FASTA format with associated metadata. Command-line example:
Metadata Standardization: Create standardized metadata table including isolation source, host, geographical origin, and collection date using controlled vocabularies per NIH data sharing requirements [116].
Quality Control and Genome Assembly Assessment
Contamination Screening: Run Foreign Contamination Screening (FCS) tool on all genomes to identify and remove contaminating sequences.
Assembly Quality Evaluation: Use Assembly QC service to assess completeness, contamination, and strain heterogeneity for each genome.
Annotation Consistency: Process all genomes through NCBI Prokaryotic Genome Annotation Pipeline (PGAP) for uniform gene calling and functional annotation [5].
Pan-genome Analysis
Gene Cluster Identification: Determine pan-genome composition using Roary pan-genome pipeline with standard parameters:
Core Genome Definition: Identify core genes present in ≥95% of strains. For W. chitiniclastica, this typically yields approximately 1,622 core genes (43% of pan-genome) [5].
Accessory Genome Characterization: Catalog strain-specific genes and identify genomic islands contributing to genetic variability.
In silico Characterization of Antimicrobial Resistance
Resistome Profiling: Identify antimicrobial resistance genes using BLAST against curated AMR databases with minimum identity of 90% and coverage of 80%.
Resistance Mechanism Classification: Categorize resistance genes by mechanism:
- Macrolide efflux pumps (macA and macB) in core genome
- Tetracycline resistance genes (tetH, tetB, tetD) in accessory genome
- Aminoglycoside modifying enzymes (ant(2″)-Ia, aac(6′)-Ia, aph(3″)-Ib, aph(3′)-Ia, aph(6)-Id)
- Beta-lactamase genes (blaVEB) [5]
Comparative Analysis: Compare resistance profiles across strains, noting absence of clinically relevant resistance genes in type strain DSM 18708T.
Virulence Factor and Phage Content Analysis
Virulome Mapping: Identify virulence-associated genes using BLAST against virulence factor databases.
Prophage Detection: Identify intact and incomplete prophages using PhiSpy with default parameters:
CRISPR Array Identification: Detect CRISPR arrays and associated cas genes using CRISPRFinder:
Data Integration and Visualization
Comparative Genomics Viewer: Upload analyzed genomes to CGV to visualize genomic variants, structural rearrangements, and region-specific conservation.
Genome Data Viewer: Use GDV to examine genomic context of resistance genes and virulence factors, identifying potential mobile genetic elements.
Phylogenetic Analysis: Construct phylogenetic trees based on core genome SNPs and compare with resistance and virulence profiles.
Results and Data Interpretation
Quantitative Analysis ofW. chitiniclasticaGenomes
Table 3: Genomic Features of Selected W. chitiniclastica Strains [5]
| Strain | Host | Isolation Source | Genome Size (bp) | CDSs | rRNA | tRNA | CRISPR Arrays | Phage Regions |
|---|---|---|---|---|---|---|---|---|
| DSM 100374 | Homo sapiens | Wound swab | 2,079,313 | 1,961 | 3 | 53 | 2 | 4 |
| DSM 100375 | Homo sapiens | Wound swab | 2,103,638 | 1,932 | 3 | 53 | 1 | 1 |
| DSM 100676 | Homo sapiens | Wound swab | 2,139,975 | 1,953 | 3 | 51 | 2 | 3 |
| DSM 100917 | Homo sapiens | Wound swab | 2,144,768 | 1,955 | 3 | 49 | 2 | 4 |
| DSM 105708 | Homo sapiens | Wound swab | 2,084,087 | 1,969 | 3 | 52 | 2 | 4 |
| DSM 18708T | Wohlfahrtia magnifica | Larvae | 2,107,748 | 1,941 | 3 | 50 | 1 | 2 |
Antimicrobial Resistance Profile
Table 4: Distribution of Antimicrobial Resistance Genes in W. chitiniclastica [5]
| Resistance Mechanism | Gene Symbols | Location | Prevalence | Notes |
|---|---|---|---|---|
| Macrolide Efflux | macA, macB | Core genome | 100% | Present in all strains including type strain |
| Tetracycline | tetH, tetB, tetD | Accessory genome | 38% | Not present in type strain |
| Aminoglycoside | ant(2″)-Ia, aac(6′)-Ia, aph(3″)-Ib, aph(3′)-Ia, aph(6)-Id | Accessory genome | 42% | Various combinations observed |
| Sulfonamide | sul2 | Accessory genome | 23% | Associated with plasmids |
| Beta-lactamase | blaVEB | Accessory genome | 19% | Confers resistance to ceftazidime, ampicillin |
Key Findings and Biological Significance
The reproducible analysis of W. chitiniclastica genomes reveals several critical insights:
Pan-genome Characteristics: The species pan-genome comprises 3,819 genes with 1,622 core genes (43%), indicating a metabolically conserved species with moderate genetic diversity [5].
Resistome Expansion: The accessory genome contains multiple clinically relevant resistance genes absent in the type strain, suggesting recent acquisition and potential for further dissemination.
Phage Content Variation: Strain-specific differences in phage content (1-5 regions per genome) contribute to genomic plasticity and potential horizontal gene transfer.
CRISPR Diversity: Variable CRISPR arrays (1-3 per genome) with spacer counts ranging from 8-188 indicate diverse phage exposure histories and adaptive immunity patterns.
Ensuring Reproducibility and Data Sharing
Adherence to NIH Rigor and Reproducibility Guidelines
Maintaining reproducibility requires strict adherence to NIH rigor and reproducibility policies focusing on four key areas: rigor of prior research, scientific rigor in design, consideration of biological variables, and authentication of research reagents [117]. For genomic analyses, this translates to:
Experimental Design Transparency: Document all analytical parameters, software versions, and database release versions.
Data Quality Documentation: Record quality metrics for each genome including coverage depth, assembly statistics, and contamination screening results.
Methodological Detail: Provide sufficient methodological detail to enable independent replication, including all code and parameters used.
Compliance with NIH Data Sharing Policies
The NIH Data Management and Sharing (DMS) Policy effective January 25, 2023 requires researchers to maximize appropriate data sharing [116]. For CGR-based projects:
Data Submission: Submit assembled genomes to GenBank through the Submission Portal, and raw sequencing data to SRA.
Metadata Standards: Use standardized data collection protocols and controlled vocabularies for metadata to enable dataset harmonization.
Timely Release: Adhere to NIH timelines for data submission and release, typically prior to publication or within 30 months of data generation.
Data Management Plan: Develop a comprehensive DMS Plan outlining how data will be managed, shared, and preserved.
This application note demonstrates a standardized protocol for leveraging NIH CGR in reproducible comparative genomic analyses of bacterial pathogens. Using W. chitiniclastica as a case study, we have illustrated how CGR's interconnected data resources and analytical tools can generate robust insights into pathogen evolution, antimicrobial resistance, and virulence mechanisms. The workflow emphasizes compliance with NIH data sharing and reproducibility requirements while providing a framework that can be adapted to various bacterial pathogens of clinical and public health significance. By implementing these protocols, researchers can ensure their comparative genomic analyses are transparent, reproducible, and maximally impactful for biomedical research and therapeutic development.
Conclusion
Comparative genomic analysis has fundamentally transformed our understanding of bacterial pathogenesis, revealing intricate patterns of evolution, host adaptation, and resistance mechanisms. The integration of robust bioinformatic methodologies with machine learning is essential to overcome data challenges and unlock the full potential of genomic data. These insights are critically informing the development of novel antimicrobials, precision therapeutics, and targeted intervention strategies. Future directions must emphasize a One Health approach, fostering collaboration across human, animal, and environmental health to monitor emerging threats, combat antimicrobial resistance, and realize the promise of genomics-driven personalized medicine.
References
- 1. The NIH Comparative Genomics Resource: addressing the ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-023-09643-4]
- 2. Comparative Genomics Fact Sheet [https://www.genome.gov/about-genomics/fact-sheets/Comparative-Genomics-Fact-Sheet]
- 3. Comparative genomics [https://en.wikipedia.org/wiki/Comparative_genomics]
- 4. Comparative Genomics - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/comparative-genomics]
- 5. Comparative Genomic Analysis of the Human Pathogen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9301364/]
- 6. comparative analysis of the genomes of bacterial pathogens [https://pubmed.ncbi.nlm.nih.gov/21764529/]
- 7. Comparative genomic analysis of pathogenic factors of ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10849-3]
- 8. The NIH Comparative Genomics Resource - PubMed [https://pubmed.ncbi.nlm.nih.gov/37759191/]
- 9. Comparative genomics reveals key adaptive mechanisms ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1543610/full]
- 10. Impact of Horizontal Gene Transfer on Adaptations to ... [https://www.sciencedirect.com/science/article/pii/S0022283625004693]
- 11. Experimental evolution and the dynamics of adaptation ... [https://www.nature.com/articles/ismej201769]
- 12. A protocol to study bacteriophage adaptation to new hosts [https://pmc.ncbi.nlm.nih.gov/articles/PMC8403759/]
- 13. From map to blueprint: the plant pan-genome unraveling ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2025.1673637/full]
- 14. Pan-genome Analysis: Statistical Profiling and ... [https://www.cd-genomics.com/resource-pan-genome-analysis-bioinformatics.html]
- 15. A stepwise guide for pangenome development in crop plants [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10931-w]
- 16. PGAP2: A comprehensive toolkit for prokaryotic pan ... [https://www.nature.com/articles/s41467-025-64846-5]
- 17. Exploring Pan-Genomes: An Overview of Resources and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10527062/]
- 18. Staphylococcus aureus in Bovine Mastitis: A Narrative ... [https://www.mdpi.com/2079-6382/14/8/810]
- 19. Genomic analysis of European bovine Staphylococcus ... [https://www.nature.com/articles/s41598-020-75179-2]
- 20. Genome sequencing and comparative genomic analysis of ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-022-09090-7]
- 21. Genomic Comparative Study of Bovine Mastitis Escherichia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4725725/]
- 22. Genomic content typifying a prevalent clade of bovine ... [https://www.nature.com/articles/srep30115]
- 23. Genome sequencing and comparative genomic analysis of ... [https://www.nature.com/articles/s41598-024-80533-9]
- 24. Genomic Analysis of Bovine Staphylococcus aureus Isolates ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7343304/]
- 25. Comparative genomics reveals key adaptive mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180303/]
- 26. Evolution and host-specific adaptation of Pseudomonas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7618370/]
- 27. Comparative Genomics of Pathogenic Bacteria [https://nhsjs.com/2025/comparative-genomics-of-pathogenic-bacteria/]
- 28. 2025 - Nucleic Acids Research - Database Issue - NCBI Insights [https://ncbiinsights.ncbi.nlm.nih.gov/2025/01/13/ncbi-resources-2025-nucleic-acids-research-database-issue/]
- 29. All Resources - Site Guide - NCBI - NIH [https://www.ncbi.nlm.nih.gov/guide/all/]
- 30. Welcome to ClinGen [https://clinicalgenome.org/]
- 31. MAGdb: a comprehensive high quality MAGs repository for ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03711-6]
- 32. The Comprehensive Antibiotic Resistance Database [https://card.mcmaster.ca/]
- 33. RGI Resistance Gene Identifier [https://card.mcmaster.ca/analyze/rgi]
- 34. An expanded database and analytical toolkit for identifying ... [https://www.nature.com/articles/s41467-024-51864-y]
- 35. VFDB 2025: an integrated resource for exploring anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11701737/]
- 36. Comparative assessment of annotation tools reveals ... [https://www.nature.com/articles/s41598-025-24333-9]
- 37. PathoFact: a pipeline for the prediction of virulence factors and ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-020-00993-9]
- 38. Machine learning based on pangenome-wide association ... [https://www.nature.com/articles/s42003-025-08650-3]
- 39. Niche-specific metabolic phenotypes can be used to identify ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3002907]
- 40. Mutational spectra are associated with bacterial niche [https://www.nature.com/articles/s41467-023-42916-w]
- 41. Machine learning prediction of bacterial optimal growth ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553261/]
- 42. Phylogenetic Framework and Molecular Signatures for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3294427/]
- 43. The antimicrobial peptides and their potential clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6684887/]
- 44. Antimicrobial Peptides: Classification, Design, Application ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.582779/full]
- 45. A generative artificial intelligence approach for the ... [https://www.nature.com/articles/s41564-025-02114-4]
- 46. Comparative genomics: the bacterial pan-genome [https://www.sciencedirect.com/science/article/abs/pii/S1369527408001239]
- 47. Antimicrobial peptides: from discovery to developmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12016500/]
- 48. New clinical trial design in precision medicine [https://www.nature.com/articles/s41392-024-01760-0]
- 49. Systematic review of basket trials, umbrella trials, and platform ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-3664-1]
- 50. Design and analysis of umbrella trials: Where do we stand? [https://pmc.ncbi.nlm.nih.gov/articles/PMC9596938/]
- 51. Basket designs: Statistical considerations for oncology trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC11637469/]
- 52. Basket trials in oncology: a systematic review of practices and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10684308/]
- 53. Basket and Umbrella Clinical Trials – What Are They and ... [https://blog.crownbio.com/basket-and-umbrella-clinical-trials-what-are-they-and-how-can-they-be-optimized]
- 54. Comparison among the Quantification of Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5487435/]
- 55. Novel clinical trial designs emerging from the molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12061631/]
- 56. Genome annotation of disease-causing microorganisms [https://pmc.ncbi.nlm.nih.gov/articles/PMC7986607/]
- 57. Unraveling the impact of genome assembly on bacterial typing [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10982-z]
- 58. Comparative Analysis and Data Provenance for 1113 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9241530/]
- 59. Comparison of genomic assembly and annotation based ... [https://www.sciencedirect.com/science/article/pii/S0923250825000804]
- 60. GenomeQC: a quality assessment tool for genome assemblies ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-020-6568-2]
- 61. Comparative genomic analyses reveal different genetic ... [https://www.nature.com/articles/s41467-025-62850-3]
- 62. Metagenome-Assembled Genomes (MAGs): Advances, Challenges, and Ecological Insights [https://www.mdpi.com/2076-2607/13/5/985]
- 63. A novel strategy for combating multidrug-resistant bacteria [https://www.sciencedirect.com/science/article/abs/pii/S0223523425008840]
- 64. Metagenome-assembled genomes: concepts, analogies, and challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8724365/]
- 65. Refining Metagenome-Assembled Genomes – [https://merenlab.org/data/refining-mags/]
- 66. Bringing the uncultivated microbial majority of freshwater ... [https://www.nature.com/articles/s41467-025-63266-9]
- 67. Tiny magnetic capsules help grow unculturable microbes [https://cen.acs.org/biological-chemistry/biotechnology/Tiny-magnetic-capsules-help-grow/103/web/2025/11]
- 68. A Global Comparative Genomic Analysis of Major Bacterial ... [https://www.mdpi.com/2076-2615/15/3/394]
- 69. Whole-Genome Sequencing of Bacterial Pathogens [https://pmc.ncbi.nlm.nih.gov/articles/PMC5608882/]
- 70. Optimizing open data to support one health: best practices to ensure... [https://onehealthoutlook.biomedcentral.com/articles/10.1186/s42522-020-00026-3]
- 71. A comparative whole-genome approach identifies bacterial ... [https://www.nature.com/articles/s42003-022-03184-4]
- 72. EnteroBase in 2025 : exploring the genomic epidemiology of bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11701629/]
- 73. A step-by-step beginner's protocol for whole genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6706130/]
- 74. Feature selection methods and genomic big data: a systematic ... [https://journalofbigdata.springeropen.com/articles/10.1186/s40537-019-0241-0]
- 75. A Review of Feature Selection Methods for Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580915/]
- 76. Feature selection revisited in the single-cell era [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02544-3]
- 77. bacLIFE: a user-friendly computational workflow for ... [https://www.nature.com/articles/s41467-024-46302-y]
- 78. A benchmark analysis of feature selection and machine ... [https://www.sciencedirect.com/science/article/pii/S2001037025001382]
- 79. Feature selection methods affect the performance of ... [https://www.nature.com/articles/s41592-025-02624-3]
- 80. Machine learning and statistical inference in microbial ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03775-4]
- 81. patient Integrating and pathogen metadata : advancing... genomic data [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-025-07207-1]
- 82. A Metadata-Driven Framework for Strengthening Pathogen ... [https://www.medrxiv.org/content/10.1101/2025.11.04.25339514v1.full-text]
- 83. Metadata integrity in bioinformatics: Bridging the gap between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10582761/]
- 84. Frontiers | Challenges and strategies in building a foundational digital... [https://www.frontiersin.org/journals/health-services/articles/10.3389/frhs.2025.1600689/full]
- 85. Chapter 3 Guidelines for Good Metadata [https://hutchdatascience.org/Choosing_Genomics_Tools/guidelines-for-good-metadata.html]
- 86. The future of multimodal artificial intelligence models for integrating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12239537/]
- 87. JMIR Formative Research - Exploring Metadata Catalogs in Health... [https://formative.jmir.org/2025/1/e63396]
- 88. Comparative genomics analysis and virulence-related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9235176/]
- 89. Comparative Genomic Analysis and Antimicrobial ... [https://www.mdpi.com/2306-7381/12/8/685]
- 90. Comparative Genomic Analysis of Antimicrobial-Resistant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9501560/]
- 91. 实时基因组学检测隐藏的抗生素耐药性 [https://blog.csdn.net/weshengxin/article/details/145361639]
- 92. ABRicate:轻松快速帮你完成细菌耐药基因及毒力基因鉴定 [https://cloud.tencent.com/developer/article/2480415]
- 93. Comparative genomic analysis of resistance and virulence ... [https://www.nature.com/articles/s41598-025-09061-4]
- 94. Comparative genome analysis reveals putative and novel ... [https://www.sciencedirect.com/science/article/abs/pii/S0882401024004959]
- 95. Whole-genome comparative analysis of virulence genes ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2015.00419/full]
- 96. Molecular Diagnostics and Therapeutic Approaches in ... [https://rsisinternational.org/journals/ijrias/articles/molecular-diagnostics-and-therapeutic-approaches-in-zoonotic-infections/]
- 97. Analysis on Cross-Species Transmission of Human– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446370/]
- 98. Comparative Genomics of Zoonotic Pathogens: Genetic ... [https://www.clinmedkaz.org/article/comparative-genomics-of-zoonotic-pathogens-genetic-determinants-of-host-switching-and-cross-species-16937]
- 99. Benchmarking strategies for cross-species integration of ... [https://www.nature.com/articles/s41467-023-41855-w]
- 100. Cross-species imputation and comparison of single-cell ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03493-x]
- 101. Wohlfahrtiimonas chitiniclastica: current insights and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11784361/]
- 102. The zoonotic pathogen Wohlfahrtiimonas chitiniclastica [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-023-03139-7]
- 103. Comparative Genomic Analysis of the Human Pathogen ... [https://pubmed.ncbi.nlm.nih.gov/35873140/]
- 104. Comparative Genomic Analysis of the Human Pathogen ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.912427/full]
- 105. Transforming antimicrobial resistance mitigation [https://link.springer.com/article/10.1007/s42452-025-07053-7]
- 106. Identification of antibiotic resistance genes from whole ... [https://onehealthadv.biomedcentral.com/articles/10.1186/s44280-025-00079-x]
- 107. A Wohlfahrtiimonas chitiniclastica with a novel type of bla ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1276314/full]
- 108. Pathogen genomics and One Health: a scoping review of current practices in zoonotic disease research | medRxiv [https://www.medrxiv.org/content/10.1101/2024.02.05.24302264v1]
- 109. Ten recommendations for supporting open pathogen genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7363500/]
- 110. Introducing PHA4GE Proposed Standards: Guiding Public ... [https://pha4ge.org/articles/introducing-pha4ge-proposed-standards-guiding-public-health-bioinformatics-software/]
- 111. Tools for bacterial comparative genomics [https://holtlab.net/2015/02/25/tools-for-bacterial-comparative-genomics/]
- 112. JCVI: A versatile toolkit for comparative genomics analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC11316928/]
- 113. About the NIH ( Comparative ) Genomics Resource CGR [https://www.ncbi.nlm.nih.gov/comparative-genomics-resource/about/]
- 114. NIH Comparative Genomics Resource (CGR) - NCBI - NLM [https://www.ncbi.nlm.nih.gov/comparative-genomics-resource]
- 115. Comparative Genomics Resource (CGR) - NCBI Insights - NIH [https://ncbiinsights.ncbi.nlm.nih.gov/2023/06/01/revolutionize-research-cgr/]
- 116. Data Sharing Policies and Expectations [https://www.genome.gov/about-nhgri/Policies-Guidance/Data-Sharing-Policies-and-Expectations]
- 117. Rigor and Reproducibility | Clinical & Translational Science ... [https://ctsi.ucla.edu/nih-requirements/rigor]